
Does the patellofemoral joint need articular cartilage?—clinical relevance
The patellofemoral joint (PFJ) is enigmatic and we know the pathomorphology for anterior knee pain (AKP) is multifaceted. I will here try to point some observations and reflections that might help to understand this complicated joint a little more and initiate further research. Previous studies have tried to outline the pathoanatomic background for AKP and more and more factors are revealed. Nevertheless, the multifaceted aspects of functional imbalance, patellofemoral malalignment (PFM) and cartilage lesions, as well as other still unknown factors, have made it difficult to find significantly differences when AKP patients are compared to controls.
As orthopedic surgeons we always strive to correct anatomical abnormalities and correct pathology to help patients experience less pain and to reach a higher level of activity. It is therefore entirely logical to argue that abnormal articular cartilage should be repaired. As surgeons we are very eager to repair the cartilage lesions as if cartilage lesions are obvious sources for the pain, but clearly we have yet not established the precise link between pain and cartilage lesions (1). Articular cartilage does not contain nerves and in itself cannot experience pain. The sources of pain in with cartilage lesions still remain obscure, and the pain may come from any of the different innervated tissues (2). According to Scott Dye the loss of tissue homeostasis is more important than the biomechanical/structural characteristic and he says that the PFJ mostly becomes symptomatic due to supraphysiologic loading (1,3). To try to describe the origin of the pain, Scott Dye (3) has said that increased cartilage wear leads to synovitis and that leads to pain.
In an MRI study by Kaplan et al. among asymptomatic elite basketball players, cartilage lesions were found in 47% of them and of those 50% were grade III/IV lesions. Patella site cartilage lesions were seen in 35% and trochlear lesions in 25% (4). The etiology for knee pain, if it is not the cartilage lesion themselves, is still an unsolved issue. Some of the most common theories are either synovitis secondary to cartilage debris or increased bone pressure and subchondral edema causing pain induced from the highly innervated subchondral bone (1). Radiologic isolated patellofemoral osteoarthritis (PFOA) has an incidence in the age group above 55 years of 24% in women and 11% in men and becomes symptomatic in 8% of women and 2% of men (5). It is well-known that some of the worst cases of cartilage lesions in the PFJ arise among patients with recurrent patellar dislocation, and despite that, a high percentage of those feel little or no pain between their dislocations.
PFJ chondral procedures have not always been as successful as similar cartilage procedures in the tibiofemoral joint. The lack of success likely reflects the fact that the PFM has not been concomitantly addressed. Cartilage repair should be accompanied by the assessment of any potential malalignment or instability of the patella focusing on the correction of the background factors. The correction of those abnormalities is considered to be necessary for the cartilage treatment to be effective and durable (6) (Figure 1). The PFM is complex and multifaceted and clearly not very well explored and the focus mostly been on the frontal plane, and to a limited degree the transverse plane, while the sagittal plan has only been touched sporadic. We know that a lateral tracking patella may occur when the TT-TG distance is increased, based upon a medialized trochlear groov or an external rotated tibia or when femoral anteversion is present or in a valgus knee (7-9). Opposite to this is a medial tracking patella, that may only be seen secondary to previous overcorrected tibial tubercle medialisation osteotomy or a tibial rotational osteotomy. Another well described cause of PFM is a tilted patella that can be secondary to trochlear dysplasia (TD) or a tight lateral retinaculum (10). We also know that when patella alta is present, this will postpone the engagement the distal pole of the patella into the trochlea groove. Patella alta have been found to predispose the patient to chondromalacia patella (11) and this is another source for PFM or patellofemoral incongruity in the transverse plane, and measured on sagittal MRI projections (12). PFM in the sagittal plane has been focused by Aksahin et al. (13) and by using sagittal MRI projections, they introduced the P-PT angle and defined it as the angle between the upper patellar pole and the lower patellar pole, and the tuberositas tibia. They compared a group of normal individuals and group of patients having chondromalacia after having excluded those individuals having TD, tilted patella or subluxations. They found a significant lower P-PT angle in the group having chondromalacia. TD is another source for PFM in the sagittal plane where the articulation between the patella and the trochlea is abnormal (14). Biedert and Bachmann found by evaluating axial MRI projections that the center of the trochlea was significantly higher when TD was present compared to normal (15) and thereby when TD is present it means that the PFM is affected in the sagittal plane. Also when TD is present you will more frequently see the type Wiberg type III patella, with a short medial facet, and in these situations only the lateral facet of the patella articulates with the flat trochlear groove (16). TD is the most important precursor for patellar instability, and it is also associated with AKP and development of PF osteoarthritis (17,18). When compared to pain-free subjects there is a greater probability that young patients with AKP will also have TD (19). Keser et al. (14) observed that the lateral trochlear inclination angle (LTI), which is associated with TD, was significantly lower in subjects with AKP compared to patients without. A reduced LTI has also been closely associated with patellofemoral instability (20) and is reported to be the single most important measurement for TD evaluation (21). So how could TD induce the pain? Biedert and Bachmann’s (15) MR findings show that the trochlear height in the center is significantly higher in knees with TD. This means that the patella tracks over the dysplasia trochlea, that has too much bone in its center, which increases the joint reaction force. An increased hydrostatic pressure and water content in the patella (8) has been found in patients with TD and AKP. In a different study MRI scan measurements showed that patients with AKP had significantly higher post-exercise chondral thinning when compared to normal individuals (22,23). Draper et al. (24) used PET/CT scans to show a greater metabolic activity in the patella and in the trochlea. He detected an important correlation between the tracer uptake and the level of pain. Van Haver et al. (25) found a greater pressure increase in the PF joint by using a simulated TD cadaver model. Studies have found a relationship between low LTI and cartilage wear or PFOA (17,18,26). If TD leads to increased pressure in the PFJ then, logically, removing the excessive bone formation central in the trochlea with a deepening trochleoplasty will unload the joint as well as better the PFJ congruence in order to determine smooth kinematics. To support this the author has in a small number of cases experienced that arthroscopic deepening trochleoplasty has reduced chronic AKP when severe trochlea dysplasia seemed to be the only underlying pathomorphology (27), and from personal message other trochleoplasty surgeons have similar observations. The increased pressure theory has been the rationale for the Maquet and the Fulkerson tibial tubercle osteotomies, and here the cartilage is unloaded by placing the tibial tubercle in a more anterior position (28). To support the theory of a positive consequence by unloading the PF joint is the positive effect a patella-thinning osteotomy has in patients having chronic AKP and OA (29).
One of the profound mysteries is why some patients despite having PFM continue to be non-symptomatic. However, a similar observation is for bowlegs, with only an undetermined proportion gets symptomatic. Nevertheless, we know that patients with bowlegged knees associated with medial pain, respond very well to a valgus tibial osteotomy, and positive observations have been found in patients having PFM, however with approximately one third having negative results (30,31). The problem with PFM is that the maltracking often involves combined factors such as TD, patella alta and increased femoral antetorsion and failure to correct all may explain why a relatively high proportion do not respond positively on surgery. Another explanation could be that cartilage lesions needed to be addressed.
Today it is clear that before considering cartilage procedures in the medial compartment of the knee, varus malalignment needs to be corrected, otherwise the wear will continue and the cartilage procedure will not last for long (32). In a recent study Ebert et al. compared ACI procedures in the tibiofemoral joint and the PFJ and actually found comparable good results. In this study, the PFM was corrected by tibial tubercle medialization and lateral release, in those patients having a TT-TG distance above 9 mm (26 pt out of 67 pt) (33). In the follow-up study after cartilage repair in the PF joint from Vasiliadis and Peterson about one third had concomitantly different types of realignment surgery including tibia tubercle transfer, trochleoplasty, proximal realignment, lateral retinaculum release and tibial osteotomy for varus or valgus deformity (6). The question arises what proportion that might have responded positively by the cartilage procedure or the realignment in isolation.
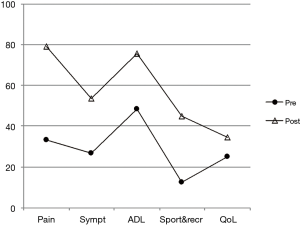
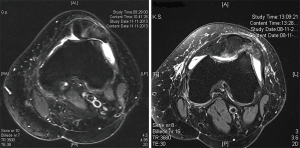
In an editorial in 2017 we reported on seven patients who presenting with TD and exposed bone on both sides of the PFJ (34). These patients had severe chronic AKP and a patellofemoral arthroplasty was most likely indicated, but the patients wanted to avoid a prosthesis and requested a less invasive procedure. As an alternative they had a resection arthroplasty including a re-shaping of the trochlea to form a groove leaving the cancellous bone exposed and un-resurfaced, a technique that is comparable to the proximal groove plasty but used only for patients with recurrent patellar instability and TD (35). Interestingly all the patients had significant reduction of their AKP. Two patients have been followed prospectively for more than 2 years and the median Kujala score improved from 37 to 69 and the Knee injury and Osteoarthritis Outcome Score (KOOS) scores can be seen in Figure 2. The procedures were in the two cases done by arthroscopic technique using round shaver burrs (Figure 3). Based upon the positive results from those controversial surgeries the question arises whether the PFJ really needs articular cartilage? When the cartilage is worn away, does it really need replacing? Given that we have patients without patellofemoral articular cartilage who are pain-free following surgery, it seems logical to conclude that, in the PFJ, congruency and smooth kinematics are more important than “normal” articular cartilage.
The abovementioned observation in respect of patella resurfacing is comparable with the trends in total knee arthroplasty. In Sweden the proportion of resurfacing of the patella has been reduced, so it is now below 2% and the advantage of resurfacing is considered limited or insignificant (36).
A recent and very important observation, was the study from Conchie et al. (37). They were the first to finally document, that there is a link between AKP in adolescence and later development of osteoarthritis in the PFJ later in life. Based on their data, they calculated that there was a 7.5 times higher risk of PFOA if they had AKP in adolescence. The result has been expected for some time, since the logic have told us that if PFM predispose to AKP and since PFM causes wear of cartilage then there should be a link between AKP and PFOA. Next would be to analyze if realignment surgery not only reduces AKP, but if it also can reduce wear of cartilage and thereby hopefully also reduce the risk of PFOA. Clearly large databases on AKP patients and a wider use of big data can help to identify and analyse the multifaceted pathomorphology of AKP. Only when we have clearly mapped the pathogenesis of AKP, can we develop algorithms for treatment protocols.
In summary, this paper tries to review alignment and biomechanical factors associated with AKP both in the younger generation with or without cartilage changes and discusses the importance or obscurity of cartilage in the PFJ. The take home message should be that any significant deviation in patellofemoral alignment should be corrected before considering cartilage procedures in the PFJ.
Acknowledgments
Thanks to Dr. Sheila Strover for correcting grammatical errors.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vicente Sanchis-Alfonso and Scott F. Dye) for the series “The Patellofemoral Joint” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.05.01).The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. LB reports personal fees from Consultan Arthrex, outside the submitted work. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sanchis-Alfonso V. Background: Patellofemoral Malalignment versus Tissue Homeostasis. In: Sanchis-Alfonso V. editor; Anterior Knee Pain and Patellar Instability. London: Springer, 2011:3-19.
- Sanchis-Alfonso V. Pathophysiology of Anterior Knee Pain. In: Zaffagnini S, Dejour D, Arendt E. editors; Patellofemoral Pain, Instability, and Arthritis. Berlin, Heidelberg: Springer 2010.
- Dye SF. The pathophysiology of patellofemoral pain: a tissue homeostasis perspective. Clin Orthop Relat Res 2005;100-10. [Crossref] [PubMed]
- Kaplan LD, Schurhoff MR, Selesnick H, et al. Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy 2005;21:557-61. [Crossref] [PubMed]
- McAlindon TE, Snow S, Cooper C, et al. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis 1992;51:844-9. [Crossref] [PubMed]
- Vasiliadis HS, Lindahl A, Georgoulis AD, et al. Malalignment and cartilage lesions in the patellofemoral joint treated with autologous chondrocyte implantation. Knee Surg Sports Traumatol Arthrosc 2011;19:452-7. [Crossref] [PubMed]
- Carlson VR, Boden BP, Shen A, et al. The Tibial Tubercle-Trochlear Groove Distance Is Greater in Patients With Patellofemoral Pain: Implications for the Origin of Pain and Clinical Interventions. Am J Sports Med 2017;45:1110-6. [Crossref] [PubMed]
- Wittstein JR, O’Brien SD, Vinson EN, et al. MRI evaluation of anterior knee pain: Predicting response to nonoperative treatment. Skeletal Radiol 2009;38:895-901. [Crossref] [PubMed]
- Dickschas J, Harrer J, Reuter B, et al. Torsional osteotomies of the femur. J Orthop Res 2015;33:318-24. [Crossref] [PubMed]
- Pagenstert G, Wolf N, Bachmann M, et al. Open lateral patellar retinacular lengthening versus open retinacular release in lateral patellar hypercompression syndrome: A prospective double-blinded comparative study on complications and outcome. Arthroscopy 2012;28:788-97. [Crossref] [PubMed]
- Luyckx T, Didden K, Vandenneucker H, et al. Is there a biomechanical explanation for anterior knee pain in patients with patella alta?: influence of patellar height on patellofemoral contact force, contact area and contact pressure. J Bone Joint Surg Br 2009;91:344-50. [Crossref] [PubMed]
- Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 2006;14:707-12. [Crossref] [PubMed]
- Aksahin E, Aktekin CN, Kocadal O, et al. Sagittal plane tilting deformity of the patellofemoral joint: a new concept in patients with chondromalacia patella. Knee Surg Sports Traumatol Arthrosc 2017;25:3038-45. [Crossref] [PubMed]
- Keser S, Savranlar A, Bayar A, et al. Is there a relationship between anterior knee pain and femoral trochlear dysplasia? Assessment of lateral trochlear inclination by magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 2008;16:911-5. [Crossref] [PubMed]
- Biedert RM, Bachmann M. Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc 2009;17:1225-30. [Crossref] [PubMed]
- Fucentese SF, von Roll A, Koch PP, et al. The patella morphology in trochlear dysplasia--a comparative MRI study. Knee 2006;13:145-50. [Crossref] [PubMed]
- Kalichman L, Zhang Y, Niu J, et al. The association between patellar alignment and patellofemoral joint osteoarthritis features--an MRI study. Rheumatology (Oxford) 2007;46:1303-8. [Crossref] [PubMed]
- Stefanik JJ, Roemer FW, Zumwalt AC, et al. Association between measures of trochlear morphology and structural features of patellofemoral joint osteoarthritis on MRI: the MOST study. J Orthop Res 2012;30:1-8. [Crossref] [PubMed]
- Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther 2000;80:965-78. [PubMed]
- Carrillon Y, Abidi H, Dejour D, et al. Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 2000;216:582-5. [Crossref] [PubMed]
- Paiva M, Blønd L, Hölmich P, et al. Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc 2018;26:746-55. [Crossref] [PubMed]
- Farrokhi S, Colletti PM, Powers CM. Differences in Patellar Cartilage Thickness, Transverse Relaxation Time, and Deformational Behavior. A Comparison of Young Women With and Without Patellofemoral Pain Shawn. Am J Sports Med 2011;39:384-91. [Crossref] [PubMed]
- Ho KY, Keyak JH, Powers CM. Comparison of patella bone strain between females with and without patellofemoral pain: A finite element analysis study. J Biomech 2014;47:230-6. [Crossref] [PubMed]
- Draper CE, Fredericson M, Gold GE, et al. Metabolic Activity At the Patellofemoral Joint. J Orthop Res 2012;30:209-13. [Crossref] [PubMed]
- Van Haver A, De Roo K, De Beule M, et al. The Effect of Trochlear Dysplasia on Patellofemoral Biomechanics: A Cadaveric Study With Simulated Trochlear Deformities. Am J Sports Med 2015;43:1354-61. [Crossref] [PubMed]
- Mofidi A, Veravalli K, Jinnah RH, et al. Association and impact of patellofemoral dysplasia on patellofemoral arthropathy and arthroplasty. Knee 2014;21:509-13. [Crossref] [PubMed]
- Blønd L. Arthroscopic deepening trochleoplasty for chronic anterior knee pain after previous failed conservative and arthroscopic treatment. Report of two cases. Int J Surg Case Rep 2017;40:63-68. [Crossref] [PubMed]
- Hall MJ, Mandalia VI. Tibial tubercle osteotomy for patello-femoral joint disorders. Knee Surg Sports Traumatol Arthrosc 2016;24:855-61. [Crossref] [PubMed]
- Vaquero J, Calvo JA, Chana F, et al. The patellar thinning osteotomy in patellofemoral arthritis: four to 18 years’ follow-up. J Bone Joint Surg Br 2010;92:1385-91. [Crossref] [PubMed]
- Rosso F, Rossi R, Governale G, et al. Tibial Tuberosity Anteromedialization for Patellofemoral Chondral Disease: Prognostic Factors. Am J Sports Med 2017;45:1589-98. [Crossref] [PubMed]
- Jack CM, Rajaratnam SS, Khan HO, et al. The modified tibial tubercle osteotomy for anterior knee pain due to chondromalacia patellae in adults: A five-year prospective study. Bone Joint Res 2012;1:167-73. [Crossref] [PubMed]
- van Heerwaarden RJ, Hirschmann MT. Knee joint preservation: a call for daily practice revival of realignment surgery and osteotomies around the knee. Knee Surg Sports Traumatol Arthrosc 2017;25:3655-6. [Crossref] [PubMed]
- Ebert JR, Schneider A, Fallon M, et al. A Comparison of 2-Year Outcomes in Patients Undergoing Tibiofemoral or Patellofemoral Matrix-Induced Autologous Chondrocyte Implantation. Am J Sports Med 2017;45:3243-53. [Crossref] [PubMed]
- Blønd L, Donell S. Does the patellofemoral joint need articular cartilage? Knee Surg Sports Traumatol Arthrosc 2015;23:3461-3. [Crossref] [PubMed]
- Peterson L, Vasiliadis HS. Proximal Open Trochleoplasty (Grooveplasty). In: Zaffagnini S, Dejour D, Arendt E. editors; Patellofemoral Pain, Instability, and Arthritis. Berlin, Heidelberg: Springer, 2010.
- Fraser JF, Spangehl MJ. International Rates of Patellar Resurfacing in Primary Total Knee Arthroplasty, 2004-2014. J Arthroplasty 2017;32:83-6. [Crossref] [PubMed]
- Conchie H, Clark D, Metcalfe A, et al. Adolescent knee pain and patellar dislocations are associated with patellofemoral osteoarthritis in adulthood: A case control study. Knee 2016;23:708-11. [Crossref] [PubMed]
Cite this article as: Blønd L. Does the patellofemoral joint need articular cartilage?—clinical relevance. Ann Joint 2018;3:46.


