
Evaluation of the patient with patellar instability
Introduction
Patellofemoral instability is a result of medial retinacular deficiency in combination with insufficient bony constraint. The lack of bony constraint can be due to either trochlear dysplasia, patella alta, or both. Patella alta exacerbates instability by causing the patella to engage late within the trochlea, therefore the patella spends a greater proportion of early flexion in a precarious state where only the ligaments constrain its mediolateral motion. The medial patellofemoral ligament (MPFL) is the primary soft tissue restraint to lateral patellar displacement, providing up to 60% of lateral restraint from 0° to 30° of knee flexion (1-3). Reconstruction of the MPFL, either in isolation or in conjunction with other procedures, is considered to reestablish patellar constraint (2,4-7).
In full extension, the patella depends on soft tissues for stability. With flexion, initial contact is distal/lateral on the patella and proximal/lateral on the trochlea. The trochlear anatomy provides an inherent mechanism to catch the patella in early knee flexion deflecting it medially into the center of the groove. The lateral facet of the trochlea provides maximal constraint in extension, with decreasing osseous constraint as the knee goes into flexion due to the diminishing height of the lateral facet of the trochlear groove from proximal to distal. With further flexion, the contact area moves distal on the femur and proximal on the patella. The extensor mechanism provides a posterior force as the knee flexes, seating the patella into the trochlea and increasing patellar stability. In deep flexion, the distal pole of the patella lifts off the center of the trochlear groove. During extreme flexion of 120 degrees, the medial “odd” facet comes into contact with the lateral margin of the medial femoral condyle (8).
Risk factors
The typical morphotype (9) of the patient with patellar instability has been characterized extensively as an adolescent female (10) with ligamentous laxity and multiple developmental anomalies (11) including patella alta (12), trochlear dysplasia (13), and rotational and angular bony malalignment (14). Trochlear dysplasia and patella alta, which reduce the “containment” of the patella within the femoral trochlea at any given flexion angle compared to the normal knee, contribute directly to the risk of recurrent patellar dislocation by reducing the relative height of the lateral trochlear buttress.
Patella alta without trochlear dysplasia is also strongly associated with patellar dislocation (15,16). Little to no trauma is required to produce a dislocation in patients with patella alta (17) because a high-riding patella does not engage the trochlea rapidly enough to control the rotational and lateralizing forces produced by weightbearing activities.
Patellar tilt and lateral subluxation, the two most frequently observed abnormalities, are caused by imbalance in the soft tissues (18). These effects can be produced by muscle imbalance (19), medial laxity, lateral tightness (20), degenerative wear of the lateral patellar cartilage, or a combination of these factors. Thus, the finding of tilt or lateral subluxation is ambiguous and offers only a vague suggestion as to the pathologic anatomy of the soft tissues.
Soft tissue dysplasia is seen more commonly among patients with patellar instability than among normal subjects (21). Ligamentous hyperlaxity, which has been described in patients with patellar instability (22), can reduce the ability of the medial ligamentous tethers to resist lateral patellar displacement. Dysplasia of soft tissues can contribute directly to patellar dislocation if it results in hyperlaxity of the ligaments responsible for preventing lateral patellar displacement.
Familial history of patellar dislocations has been reported to increase the risk of failed surgical stabilization (23). Reportedly, at least some of the anatomical factors that contribute to patellar instability are heritable (24,25).
Clinical evaluation
History
Obtaining a detailed history is critical when planning to treat a patient with patellar instability. A careful history should include total number of dislocation events, age at first dislocation, mechanism, amount of swelling present after dislocation, description of sensation at time of episode(s) and whether the knee cap came out of place, prior treatments (including whether a reduction was necessary), symptomatology between instability episodes, and family history regarding patellar instability and/or systemic hypermobility (26). The clinician should ascertain whether the primary complaint is pain or instability. Patients with recurrent instability will have pain associated with the dislocation events, but will not have significant pain in the intervening periods. A primary complaint of pain does not respond well to treatments and surgeries that are designed to treat instability, and the converse is true.
Elements of the history can influence the treatment plan. A history of contralateral patellar dislocation would increase the risk of recurrence six-fold, which is as much as a previous dislocation on the index knee (27). Non-contact and episodic instability is more likely to require surgical stabilization than a first-time traumatic dislocation (28). Locking or catching symptoms, in addition to reports of significant swelling, may correlate with osteochondral loose bodies, which may require removal for small fragments and fixation for larger fragments.
A history of prior surgery can greatly influence our understanding of the pathology. For patients who have had prior surgery, ask them to bring operative reports and intra-operative pictures. A history of prior lateral release can reduce resistance to lateral displacement (7) and increase the risk of iatrogenic medial dislocations (29-32). Prior MPFL reconstructions can also affect patellar mobility, but an adequate reconstruction should prevent lateral instability. However, a history of an MPFL reconstruction along with a history of a lateral release can lead to medial instability. Patients cannot reliably discern the direction of instability, but this can be determined in clinic and occasionally requires an examination under anesthesia. MPFL reconstructions with a graft that is too tight in extension may contribute to prolonged extensor lag postoperatively (33). In contrast, a graft that tightens excessively in flexion could restrict knee flexion. Prior tibial tubercle osteotomy (TTO) can also alter patellofemoral mechanics. Over, distalization can lead to a loss in terminal flexion, whereas over medialization can contribute to iatrogenic medial instability. Symptomatic hardware has also been reported (34), although this should be easily distinguished from instability.
Physical exam
Every patient should receive a thorough knee examination, including evaluation of gait, bilateral hips, knee ligament exam, and alignment in all planes. The objective in the patellofemoral examination is to verify and understand the excessive motion of the patella due to lack of constraint, and the exam starts with ensuring that the patella is currently reduced. After obtaining a thorough history, the patient should easily be classified into one of the following three categories:
- First time patellar instability;
- Recurrent patellar instability;
- Patients having undergone previous surgery.
For an acute dislocation, whether first time or recurrent, effusion with tenderness to palpation over the medial retinaculum is a typical finding. If the effusion is large and tense, aspiration can serve as a palliative measure and can also assist in diagnosing an osteochondral fracture. Other important examination findings for both patients with first time and recurrent patellar dislocations include:
- Lateral and medial patellar translation at full extension and 30 degrees of flexion: laxity is measured by quadrants or millimeters. Pathologic laxity is appreciated when there is apprehension and an absence of an endpoint with lateral translation at 30 degrees of flexion. In full extension, translation in the pathologic knee is asymmetric and without a firm endpoint. In patients with recurrent dislocations, tight lateral structures may be encountered indicating that a lateral lengthening procedure might be a beneficial adjunct.
- J sign: the patella abruptly translates laterally as the knee is fully extended, moving in an upside-down “J” pattern. For a patient who has failed non-operative treatment and is having recurrent dislocations, a persistent J sign may be encountered where the patella reduces into the trochlea at a higher flexion angle.
- Patellar facet palpation: tenderness may indicate an osteochondral or avulsion injury.
- Hip rotation: particularly in the patient with recurrent dislocations when operative intervention is being considered, a more complete rotational profile should be assessed to determine if additional factors may be contributing to the patellar instability. Excessive hip anteversion is best assessed in the prone position with the knees flexed and hips extended. If internal rotation exceeds external rotation by 45° or more, then consider a CT for axial lower extremity rotational alignment.
- If considering a TTO with distalization for patella alta, it is particularly important to assess knee flexion in this position. Patellar instability is often associated with a constellation of symptoms called “miserable malalignment”, which is increased femoral anteversion, hyperpronation of the foot, and external tibial torsion (35). Patients with significant valgus when standing should be more closely evaluated for these other anomalies.
- Hypermobility: an emphasis should be placed on evaluation of knee hyperextension. General ligamentous laxity should be assessed using the Beighton hypermobility score (36).
The Q-angle is rarely helpful, as it is imprecise and changes with patellar mobility. If a patella is subluxed laterally, the Q-angle measurement is falsely low. On the other hand, femoral and tibial torsion can play a role in patellar instability, with the largest lateral force placed on the patella when the tibia rotates externally in terminal knee extension.
Patients having undergone previous surgery for patellar instability should be carefully evaluated for medial patellar instability. Some of these exam maneuvers include a gravity subluxation test (29), medial apprehension test (31), and relocation test (37). The gravity provoked medial subluxation test is positive if medial patella subluxation occurs in lateral decubitus position. The relocation test occurs when the patella is manually displaced medially and the knee is quickly flexed. The test is positive if the maneuver reproduces the symptom of the patella moving from too far medial back into the trochlear groove.
Imaging
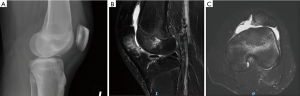
AP, lateral, and merchant radiographs are used to confirm patellar location, presence of osteochondral fracture, and patellofemoral relationships. An osteochondral fracture that is visible on conventional radiographs is likely a significant lesion that should be more closely evaluated with an MRI and possible surgical excision or fixation (Figure 1). The lateral view with the knee flexed 30° can help determine patella height. A Caton-Deschamps ratio of more than 1.2 implies patella alta, which predisposes to lateral instability as the medial patellar facet is not captured by the lateral femoral condyle in early flexion. A perfect lateral view (with the posterior condyles aligned) can evaluate trochlear dysplasia. The “crossing” sign, where the curve of the trochlear floor crosses the anterior contour of the lateral femoral condyle, represents flattening of the trochlear groove and absence of trochlear constraint against patellar displacement. Trochlear prominence (also called a trochlear “boss”, “bump” or “eminence”) is represented by the distance between the most anterior point of the trochlear floor and a line drawn along the distal 10cm of the anterior femoral cortex. The degree of trochlear prominence on a lateral radiograph correlates with severity of dysplasia. Although MPFL reconstruction does not directly address trochlear dysplasia, it is helpful to understand the forces contributing to patellar instability when performing the procedure. In patients with prior MPFL reconstructions, the tunnel positions need to be critically evaluated (Figure 2).

In evaluating a patient with recurrent dislocations that has failed non-operative measures and is being considered for operative treatment, all factors that can contribute to instability need to be evaluated such as trochlear dysplasia type, patella alta, and TT-TG [or tibial tubercle-posterior cruciate ligament (TT-PCL) offset].
Dejour et al. (18) identified four factors in knees with symptomatic patellar instability: (I) trochlear dysplasia, as defined by the crossing sign and quantitatively expressed by the trochlear bump (>3 mm) and trochlear depth (≤4 mm); (II) quadriceps dysplasia, which they defined as present when the patellar tilt in extension was more than 20° on the CT scans; (III) patella alta (Caton-Deschamps) index greater than or equal to 1.2; and (IV) increased tibial tubercle-trochlear groove (TT-TG) distance (≥20 mm). Like many other authors before and since, they concluded from these data that the etiology of patellar instability is multifactorial.
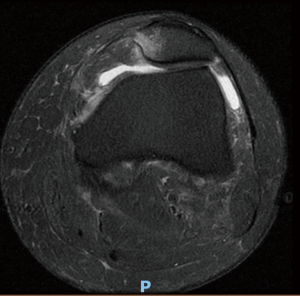
We advocate for an MRI examination on all first-time dislocations for the primary objective of assessing for osteochondral or chondral injuries that are amenable to surgical intervention. The secondary objective of the MRI is to ascertain the location of the MPFL lesion (Figure 3), which has prognostic value. An MPFL avulsion at the femoral attachment in primary traumatic patellar dislocations predicts subsequent patellar instability. Sillanpää et al. (38) suggest that MPFL injury location be taken into account when planning treatment of primary traumatic patellar dislocation. Axial MRI images are also used to determine TT-TG distance (or TT-PCL offset), which drives the decision to perform a TTO in addition to the MPFL reconstruction.
Conclusions
Patellofemoral instability is a result of medial retinacular deficiency in combination with insufficient bony constraint. It is a multifactorial entity that must be critically evaluated prior to undergoing operative intervention. We advocate evaluating patients based on whether they have experienced a first dislocation event, recurrent dislocations, or have recurrent dislocations after failed surgical management. Evaluation of all the above groups of patients involves evaluating all potential contributors (patella alta, trochlear dysplasia, generalize laxity). As with most orthopaedic diagnoses, history and physical exam provide much of the information needed to make a treatment decision. Imaging modalities can be used to assess factors contributing to instability and determine which interventions might be most beneficial.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vicente Sanchis-Alfonso and Scott F. Dye) for the series “The Patellofemoral Joint” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The series “The Patellofemoral Joint” was commissioned by the editorial office without any funding or sponsorship. DCF is a paid consultant for Breg, Inc. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee 2000;7:121-7. [Crossref] [PubMed]
- Hautamaa PV, Fithian DC, Kaufman KR, et al. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 1998;174-82. [Crossref] [PubMed]
- Davis DK, Fithian DC. Techniques of medial retinacular repair and reconstruction. Clin Orthop Relat Res 2002;38-52. [Crossref] [PubMed]
- Fithian DC, Mishra DK, Balen PF, et al. Instrumented measurement of patellar mobility. Am J Sports Med 1995;23:607-15. [Crossref] [PubMed]
- Teitge RA, Faerber W, Des Madtyl P, et al. Stress radiographs of the patellofemoral joint. J Bone Joint Surg Am 1996;78:193-203. [Crossref] [PubMed]
- Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682-93. [Crossref] [PubMed]
- Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 1998;26:59-65. [Crossref] [PubMed]
- Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-5. [Crossref] [PubMed]
- Lerat JL. Morphotypes of patellar instability. Rev Chir Orthop Reparatrice Appar Mot 1982;68:50-2. [PubMed]
- Floyd A, Phillips P, Khan MR, et al. Recurrent dislocation of the patella. Histochemical and electromyographic evidence of primary muscle pathology. J Bone Joint Surg Br 1987;69:790-3. [Crossref] [PubMed]
- Mäenpää H, Lehto MU. Patellar dislocation has predisposing factors. A roentgenographic study on lateral and tangential views in patients and healthy controls. Knee Surg Sports Traumatol Arthrosc 1996;4:212-6. [PubMed]
- Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am 2007;89:1749-55. [PubMed]
- Dejour H, Walch G, Neyret P, et al. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot 1990;76:45-54. [PubMed]
- Post WR, Teitge R, Amis A. Patellofemoral malalignment: looking beyond the viewbox. Clin Sports Med 2002;21:521-46. [Crossref] [PubMed]
- Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med 2000;28:472-9. [Crossref] [PubMed]
- Simmons E Jr, Cameron JC. Patella alta and recurrent dislocation of the patella. Clin Orthop 1992;265-9. [PubMed]
- Geenen E, Molenaers G, Martens M. Patella alta in patellofemoral instability. Acta Orthop Belg 1989;55:387-93. [PubMed]
- Dejour H, Walch G, Nove-Josserand L, et al. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 1994;2:19-26. [Crossref] [PubMed]
- Delgado-Martínez AD, Estrada C, Rodriguez-Merchan EC, et al. CT scanning of the patellofemoral joint. The quadriceps relaxed or contracted? Int Orthop 1996;20:159-62. [Crossref] [PubMed]
- Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography. A preliminary study. Clin Orthop 1986;286-93. [PubMed]
- Rünow A. The dislocating patella. Etiology and prognosis in relation to generalized joint laxity and anatomy of the patellar articulation. Acta Orthop Scand Suppl 1983;201:1-53. [Crossref] [PubMed]
- Stanitski CL. Articular hypermobility and chondral injury in patients with acute patellar dislocation. Am J Sports Med 1995;23:146-50. [Crossref] [PubMed]
- Mäenpää H, Lehto MU. Surgery in acute patellar dislocation--evaluation of the effect of injury mechanism and family occurrence on the outcome of treatment. Br J Sports Med 1995;29:239-41. [Crossref] [PubMed]
- Beighton PH, Horan FT. Dominant inheritance in familial generalised articular hypermobility. J Bone Joint Surg Br 1970;52:145-7. [Crossref] [PubMed]
- Miller GF. Familial recurrent dislocation of the patella. J Bone Joint Surg Br 1978;60-B:203-4. [Crossref] [PubMed]
- Post WR, Fithian DC. Patellofemoral Instability: A Consensus Statement From the AOSSM/PFF Patellofemoral Instability Workshop. Orthop J Sports Med 2018;6:2325967117750352 [Crossref] [PubMed]
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history. Am J Sports Med 2004;32:1114-21. [Crossref] [PubMed]
- Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 2007;93-101. [Crossref] [PubMed]
- Nonweiler DE, DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med 1994;22:680-6. [Crossref] [PubMed]
- Sanchis-Alfonso V, Merchant AC. Iatrogenic medial patellar instability: an avoidable injury. Arthroscopy 2015;31:1628-32. [Crossref] [PubMed]
- Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 1988;16:383-8. [Crossref] [PubMed]
- Merican AM, Kondo E, Amis AA. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech 2009;42:291-6. [Crossref] [PubMed]
- Erasmus PJ, Thaunat M. MPFL reconstruction: Principles and complications. In: Sanchis-Alfonso V. editor. Anterior Knee Pain and Patellar Instability. London: Springer, 2011:389-96.
- Payne J, Rimmke N, Schmitt LC, et al. The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy 2015;31:1819-25. [Crossref] [PubMed]
- James SL, Bates BT, Osternig LR. Injuries to runners. Am J Sports Med 1978;6:40-50. [Crossref] [PubMed]
- Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis 1973;32:413-8. [Crossref] [PubMed]
- Fulkerson J. A clinical test for medial patella tracking (medial subluxation). Tech Orthop 1997;12:144. [Crossref]
- Sillanpää PJ, Salonen E, Pihlajamäki H, et al. Medial patellofemoral ligament avulsion injury at the patella: classification and clinical outcome. Knee Surg Sports Traumatol Arthrosc 2014;22:2414-8. [Crossref] [PubMed]
Cite this article as: Khan N, Stewart R, Fithian DC. Evaluation of the patient with patellar instability. Ann Joint 2018;3:56.


