Treatment of the medial collateral ligament injuries
Introduction
An injury of the medial compartment occurs when a valgus force is applied to the knee, with a contact or non-contact mechanism. It may present more frequently as an isolated lesion, or in association with a wide spectrum of ligament injuries (1). The indications regarding the treatment of the medial aspect of the knee still present some controversies, mainly in cases of associated lesions. The controversy arises from the significant intrinsic repairing capacities of the medial structures and from the possibility of joint arthrofibrosis secondary to repair or surgical reconstruction (2). Unlike other structures, a unique decision algorithm shared by all authors is not yet available. Furthermore, numerous surgical techniques have been described with specific challenges, complications and results, which makes it difficult to choose which specific technique to use in every situation.
Functional and surgical anatomy
The anatomical basis for the medial compartment is now widely known. Warren et al. (3) initially divided the medial structures into 3 layers. Layer I includes the crural fascia, layer II the medial patellofemoral ligament, the superficial medial collateral ligament (sMCL) and part of the ligament components of the posteromedial corner (PMC) and layer III encloses the deep medial collateral ligament (dMCL), the joint capsule and the remaining components of the PMC. Thus, there is a connection between the two deeper layers.
Subsequently, Robinson et al. (4) described the medial structures dividing them into thirds. There is the anterior third comprising the capsular ligaments covered by the medial retinaculum of the extensor apparatus, the middle third comprising the sMCL and dMCL and the posterior third comprising the PMC. The latter includes, from the most superficial to the deepest layer, the fascia, the posterior oblique ligament (POL), the insertions of the semimembranosus, the oblique popliteal ligament and the posteromedial portion of the meniscus.
A further description, extensive and detailed, has been more recently reported by LaPrade et al. (5). The important concepts to remember for a correct approach to the pathology of this area are the biomechanics of every single structure and their anatomical insertions.
The sMCL has an ovoid semi-circular femoral insertion on average 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. There are two distal insertions onto the tibia. The sMCL attaches 12.2 mm distally from the joint line, and the POL mostly an insertion into soft tissues of this region, particularly to the most anterior head of the semimembranosus muscle. The more distal insertion is just anterior to the posteromedial crest of the tibia, approximately 61.2 mm from the joint line, inserting directly into the cortical bone. This structure has main control of the valgus throughout the full range of motion and helps to limit internal rotation of the tibia when the knee is beyond 30° of flexion as the posteromedial complex is loose (6).
The dMCL is a capsular thickening that strongly adheres to the meniscal wall and divides into the meniscofemoral (MF) ligament and the meniscotibial ligament (MT). The first has a femoral insertion located approximately 1 mm distal and posterior to the medial epicondyle, the latter is only 3 mm distal to the articular cartilage of the tibia. The biomechanical importance of this structure is mainly to control the anterior tibial translation of the flexed and externally rotated knee. Its role in controlling valgus stress is less relevant. Sectioning of dMCL does not increase the instability of a knee subjected to valgus stress if the sMCL is intact (7).
The POL is a thickening of the posteromedial capsule with a femoral origin approximately 7 mm distal and 6 mm posterior to the adductor tubercle, just distal and anterior to the gastrocnemius tubercle. Directed distally, it assumes a fan shape, mainly inserted on the insertion of the semimembranosus muscle but also on the meniscal wall, the posteromedial tibial cortex and the medial head of the gastrocnemius. This structure is tight in extension and in the first degrees of knee flexion to ensure valgus stability. The role of the POL is even more pronounced in the case of an sMCL deficient knee. It also controls internal tibial rotation and posterior tibial translation, especially if the posterior cruciate ligament (PCL) is absent (8).
This role makes the posteromedial capsule of great importance in the case of a multi-ligament lesion. If its function is not reconstituted, it increases the stress on the reconstructed sMCL or PCL.
Incidence
The medial collateral is the most frequently injured ligament of the knee. It has an increasing incidence linked to more widespread participation in traumatic sporting activities. Isolated lesions of the medial compartment in the sports active population stands at around 7.3/1,000 people/year. Of those, 73% are grade I injuries, 23% grade II and only 4% grade III (9).
The most frequent sports involved are football (soccer), American football and skiing. The use of some prophylactic bracing is still controversial as the results of clinical trials on the prevention and decrease in MCL lesions are contradictory (10).
Grade III lesions are normally associated with at least one of the cruciate ligaments injury in 78% of the cases, most frequently the anterior cruciate ligament (95%) (11). Multi-ligament injuries are more closely related to high-energy trauma or within the scenario of a knee dislocation.
Patient evaluation
The stability of the knee should be tested on all planes in order to evaluate antero-posterior, lateral, and rotational instability. The standard evaluation is based on the valgus stress in both extension and at 30° of flexion. It is important to recognize pure valgus instability from instability in valgus and internal rotation. Valgus stress is not always meaningful in this sense. In the case of an isolated lesion of the medial compartment, the persistence of instability in both flexion and extension indicates the involvement of the PMC. However, in case of involvement of the central pivot, this test is less specific. Therefore, it is better to use the anterior drawer test keeping the tibia in external rotation. Significant translation will indicate a lesion of the PMC (12).
Moreover, with a significant anteromedial translation can appear a positive dial test, which is mostly true for POL injuries. In order to differentiate anteromedial instability from posterolateral corner insufficiency, the dial test can be performed in the prone position to visually evaluate the subluxation of the medial tibial plateau on the medial condyle or alternatively carry out a varus stress test to exclude lateral lesions.
The two most used classifications of the medial compartment lesions are the American Medical Association Classification and the Fetto and Marshall Classification. To these, we can add a further clinical classification of valgus stress at 30° measured in millimeters of aperture compared to the contralateral knee. The three classifications are summarized in Table 1.

Full table
A long-standing X-ray of the lower limbs should always be acquired to evaluate the axis and evaluate any potential deviation in the follow-up due to the medial lesion. In addition, a lateral view is necessary to avoid misdiagnosis of fractures, avulsions and dislocations. Stress radiographs in the acute setting are only required in the pediatric population to distinguish between ligament and physeal injuries (13).
In the chronic setting, it is useful to quantify the degree of instability with valgus stress X-rays in all the patients. The isolated section of the sMCL causes a medial opening in valgus stress compared to the contralateral knee of about 3.2 mm. This opening increases to 9.8 mm in the case of a complete section of the medial structures (sMCL, dMCL, POL) (14).
MRI helps to diagnose associated injuries. Furthermore, it accurately shows the location of the lesion of the medial collateral and its possible relationships to closely related structures such as the ligament entrapped under the medial meniscus or at hamstring tendon insertions (Stener-type lesion). A wave sign is typical of tibial avulsion injuries (Figure 1). Bone bruise in the lateral compartment in isolated injuries of the MCL is present in only 45% of cases and should warn of possible serious lesions (15).

In chronic cases, if doubts persist after careful clinical evaluation, an MRI with intra-articular contrast may be taken. T1-weighted fat-saturated sequences acquired after injection of intraarticular contrast have demonstrated the best visualization of the POL and posteromedial capsule (13).
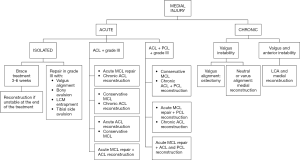
Treatment algorithm
The rationale behind non-operative treatment is the high intrinsic healing potential of the medial structures that derives from numerous predisposing factors (16). The physiological varus alignment of the knee and the concave geometry of the medial tibial plateau favors healing from an anatomical point of view while the generous local vascularization and the absence of contact with the synovial fluid do the same from the biological point of view (16). In animal models early mobilization showed a favorable stimulus to healing in cases of non-operative treatment (17).
Conversely, some factors negatively affect healing during nonoperative treatment, such as smoking and valgus mechanical axis. Smoking is probably due to the reduction in local micro vascularization and a valgus mechanical axis is because the medial structures are more stressed. Finally, a distal avulsion of the MCL at its insertion on the tibial cortex, being smooth, makes spontaneous re-insertion more difficult (18,19).
Prolonged immobilization must be avoided, firstly, for the consequent reduction of the healing response and, secondly, for the possibility of post-immobilization stiffness. To avert this complication, reaching early full extension is recommended. This is particularly true for lesions located at the femoral insertion. Therefore, immobilization and the use of crutches are recommended for a very short period. Isometric strengthening exercises can be started from the first moment of rehabilitation. Varus-valgus stress should be avoided by using a hinged knee brace for 3–6 weeks.
The use of Mesenchymal Stem Cells and PRP to accelerate and promote healing is still contradictory as only animal studies and some case reports on the subject are currently available. Some animal studies even demonstrate a possible reduction in the quality of the regenerated tissue in the case of excessive local administration of PRP (20).
In the case of isolated grade I and II lesions of the medial collateral, non-operative treatment is always indicated. This type of treatment has demonstrated a rapid return to sporting activity, 11 days for grade I and 20 days for grade II (21). Long-term clinical results are also excellent (22).
In the past, the recommendation for grade III injury was acute surgical repair. Currently, many authors also recommend the same non-operative protocol used for grade I and II lesions, reserving a chronic reconstruction in the event of a residual subjective instability. Cases series have been reported of returns to sport at 9 weeks after non-operative treatment of grade III lesions (23).
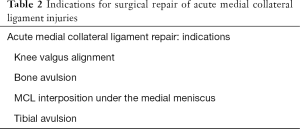
Surgical repair of an isolated acute lesion (<3 weeks) of grade III lesions is recommended in the case of considerable knee valgus alignment, bone avulsion, MCL interposition under the medial meniscus, tibial dislocation and medial gapping in full extension (Table 2).
Full table
In the first case (valgus alignment), there is a disadvantage from a biomechanical point of view for the healing of the lesion. In the case on a bony avulsion, the ligament itself remains intact and the healing must take place on the bone side and then fixation appears more effective. If the MCL is interposed under the medial meniscus, conservative treatment may affect the meniscal biomechanics and must also be addressed surgically. Finally, tibial side lesions have less healing potential because the tibial cortex appears smoother than that of the femoral epiphysis. In addition, lesions at this level could be entrapped at the level of the hamstring tibial insertion (Stener-like lesion), which prevents healing far from its native footprint (19).
Grade III injuries associated with ACL ruptures may have different therapeutic approaches. The first possibility is non-operative treatment of the medial collateral injury followed by a late reconstruction of ACL. It may be associated with reconstruction of the medial component if valgus instability persists at the time of surgery. In this case, a single procedure has been reported to achieve better outcomes. Caution must be placed in the evaluation of any residual valgus laxity at the intraoperative assessment. Medial laxity can lead to an overload on the reconstructed cruciate ligament with consequent failure (24).
It should be kept in mind that the ACL is the primary restraint to anterior translation and acts as a secondary restraint to valgus stress. On the other hand, the MCL is the primary restraint to valgus stress at 30 degrees, whereas the POL, the posteromedial capsule, and the posterior horn of the medial meniscus all act as secondary restraints to anterior instability.
The second alternative is acute reconstruction of the ACL with subsequent non-operative treatment of the MCL. Some studies claim that the restoration of the kinematics of the knee with an intact ACL would give a mechanical stimulus to the healing of the medial structures (25,26).
The problem with this second possibility is that the patient would need a second surgery to treat the medial instability in case of failure of the non-operative treatment of the MCL.
Another strategy is acute reconstruction of the ACL associated with a repair and/or reconstruction of the MCL. It is currently the least recommended as it seems to increase the possibility of postoperative stiffness compared to the same result in terms of stability (11,27).
The last treatment option is acute repair of the MCL and late reconstruction of the ACL. In this case, we avoid a double reconstruction at the same time but the patient certainly undergoes two surgeries. This approach is to be reserved in easily repairable lesion patterns such as femoral avulsions (28).
In grade III injuries of the medial side with concomitant injuries of both cruciate ligaments, different alternatives are to be considered. They are (I) non-operative treatment of the medial structures with delayed ACL and PCL reconstruction; (II) acute medial repair and acute reconstruction of PCL with chronic reconstruction of ACL; (III) acute treatment of all 3 structures with MCL repair and ACL/PCL reconstruction.
The first option ensures the avoidance of a medial approach in cases where there is acceptable healing with non-operative treatment. Given the close correlation between the posteromedial capsule and PCL, the treatment of these two structures must always take place in a consensual way if a surgical approach to the medial side is necessary.
In cases of chronic ruptures, the alignment of the knee needs to be evaluated. In the case of a valgus knee and isolated valgus instability, a femoral varus osteotomy is recommended.
If the axis of the lower limb is neutral or varus, capsular procedures associated with augmentation/medial reconstruction are indicated. In cases of combined valgus and anteroposterior instability, reconstruction of the ACL and an intraoperative evaluation of residual instability is recommended. If it is greater than 4 mm, the combined reconstruction of the medial structures should be performed (6).
Flow chart is resumed in Figure 2.
Surgical options
Several techniques have been suggested over time for the repair, reconstruction, augmentation and capsular advancement of the medial structures.
In the case of repair, the recognition of the injured structures is of outmost importance given that the patients will have poor outcomes in cases of insufficient repair of the PMC (13).
Evaluation under anesthesia and a diagnostic arthroscopy can confirm the degree of injury and associated lesions. If a diagnostic arthroscopy is carried out, the use of low inflow pressure is suggested to decrease fluid extravasation that can make the succeeding surgical steps more complex.
The indications for acute repair as compared to chronic reconstruction have already been discussed. With regard to the superiority of one over the other, we only emphasize the superiority of the reconstruction compared to the repair in patients with a knee dislocation. Stannard et al. have, in fact, found a failure rate of 4% in the first and up to 20% in the second (29). The indication for acute repair or reconstruction/augmentation is based on the quality of the remaining tissue and the location of the lesion.
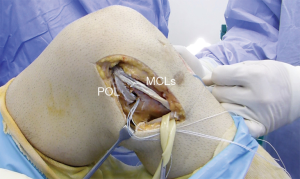
When an acute repair is performed: tibial and femoral avulsions are generally fixed while augmentation or reconstructions are indicated for midsubstance lesions due to the poor quality of the tissue. A femoral avulsion of the POL can be approached with an anchor while distal avulsions, in particular the branch directed to the semimembranosus, can be done with direct suturing to the semimembranosus or on the posterior portion of the sMCL. It is important to recognize and always perform a repair of the meniscotibial ligament with an anchor at the tibial border. Peripheral lesions of the medial meniscus can be found in about 33% of cases and repaired directly (30).
The fixation of these deep structures must take place keeping the knee in extension and slightly varus. Avulsions of the sMCL usually allow for reintegration with anchors, staples or screws, given the quality of the tissue. Femoral reinsertions are associated with greater postoperative stiffness than at other sites (27). Repairs at this level must take place slightly varus and at 30° of flexion.
Capsular re-tensioning is rarely used today. The posteromedial capsule can be detached from the meniscal wall and sutured to a more anterior position on the meniscus itself again. In the case of generalized laxity, you can go for “en masse” elevation with a complete dislocation at the tibial or femoral level and a more distal or proximal relocation after having identified an isometric point (31).
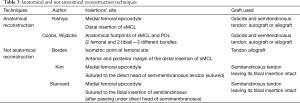
More modern reconstructions can be subdivided into non-anatomical or anatomical (Table 3). Yoshiya et al. described an isolated anatomical reconstruction of the sMCL with a dual autograft made up of the gracilis and semitendinosus tendons (19).
Full table
The technique is to be reserved for patients with an isolated valgus instability at 30° of flexion. The technique involves 2 small incisions centred on the medial epicondyle of the femur and at the center of the distal insertion of the sMCL. Fixation requires a cortical button for the tibial insertion and an interference screw for the femur at the posterosuperior level of the medial epicondyle. The author suggests harvesting the two tendons distally since the hamstring is inserted more anteriorly than the sMCL at the level of the tibia. Likewise, the length of the graft must also be considered to restore anatomical stability (32).
Coobs et al. and Wijdicks et al. described a complete anatomical reconstruction that handled instability in both extension and flexion (33,34). The technique consists in the reconstruction of the sMCL and of the POL using 2 distinct autografts or allograft. The grafts are fixed with interference screws in tunnels located at the anatomical footprints of the two structures, both on the femoral and at the tibial side. The authors emphasize that the anatomical reconstruction of the sMCL is crucial. It is necessary to reach the distal insertion on the tibia at 6 cm from the joint line and to fix the graft at the level of the posterior margin of the native sMCL as anterior insertions lead to graft overload, at maximum degrees of flexion, and failure of the construct.
Furthermore, the proximal tibial insertion of the sMCL must also be reconstituted. Being anatomically an insertion prevalently in soft tissues, a direct suture to the anterior head of the semimembranosus can be sufficient. Alternatively, an anchor can be positioned at this level. The tension of the sMCL must take place at 30° of flexion and that of the POL in extension. In vitro studies have shown how this technique can restore correct stability resulting in a medial opening under valgus stress of less than 2 mm (35). Then again, a clinical study has shown a decrease in the opening during valgus stress from 6.2 to 1.3 mm in 28 patients (36).
Most of the non-anatomic techniques used involve only one femoral tunnel, which, of course, is not in line with the knowledge about the anatomical insertions of the medial structures. This tunnel should be located at a defined isometric point. The isometric point might be approximated by the intersection of a line drawn down from the anterior aspect of the posterior femoral cortex and Blumensaat line (13).
As a more accurate alternative to the use of fluoroscopy, pins can be used to evaluate the real isometry of the desired tunnel placement. This can be done by passing a wire or the graft chosen around the first pin inserted at the femoral level and the second placed at the desired tibial insertion and the movement is then evaluated during a complete ROM. Movements of less than 2 mm during complete knee ROM are considered acceptable (37). Some authors do not calculate the isometric point but rather locate the femoral tunnel posterior and proximal from the medial epicondyle.
The tunnel is directed approximately 30° proximally and 30° anteriorly to avoid interference with tunnels for the ACL, PCL, and posterolateral corner reconstructions in patients with multi-ligament knee injuries (38).
Borden et al. first suggested reconstruction with an allograft fixed at the proximal femoral level and with 2 bundles distally. Both bundles are fixed at the level of the distal insertion of the sMCL. The first is done at the anterior margin of the medial collateral and the second about 2.5 cm more posterior (39).
Kim et al. described a technique using the autologous semitendinosus tendon, leaving its tibial insertion intact. The technique involves fixation of the semitendinosus midsubstance at the medial epicondyle. The remaining tendon is finally sutured to the direct head of the semimembranosus tendon, thus recreating the central portion of the POL (37).
Stannard suggested a modification to the latter technique. The semitendinosus is similarly fixed to the femur, but it is then passed under the direct head of the semimembranosus and fixed with sutures to the tibial insertion of the semitendinosus (13). The advantage of this technique is that once fixation is complete, it is possible to suture the 2 distal heads of this triangular construction together in a V-Y fashion, which increases its tension, if the stability of the PMC is not sufficient. Stannard reported 2 years outcomes in patients with knee dislocation treated with this technique. Only 3.7% of the cases using an autograft and in 4.8% using an allograft failed (29).
Lind et al. has suggested a more anatomical modification (Figure 3). The semitendinosus is also similarly fixed to the femur, but then the free end is fixed in the tibia through a tunnel, recreating the POL more anatomically. This tunnel must be drilled in an antero-posterior direction, exiting at the level of the posteromedial condyle of the tibia approximately 10 mm distally from the articular line, posteriorly and laterally to the insertion of the semimembranosus. This allows for more stable fixation via an interference screw (40).

To more anatomically reproduce the distal insertion of the sMCL, the distal attachment of the semitendinosus may be detached and fixed more posteriorly (16).
At 2-year follow up, this technique has demonstrated a laxity in valgus stress of less than 5 mm in 98% of the cases and an IKDC A or B in 74% (40).
In case of combined PCL/MCL reconstructions, there are some techniques in the literature that use the same graft for the reconstruction of both structures with a single femoral tunnel (41).
In any contemporary reconstruction technique of the sMCL and PMC with a single femoral tunnel, the use of an allograft with bone plug (e.g., Achilles tendon) allows for bone-to-bone femoral fixation and the use of soft tissues divided into two ends for tibial fixation (Figure 4).
The techniques described may include the use of different grafts. They include the hamstring or quadriceps tendons autograft as well as the hamstring, tibialis anterioris and Achilles allografts. So far, there is no evidence to support one graft or technique over another (30,42).
An allograft is typically recommended in multiligamentous injuries as it eliminates graft site morbidity, reduces dissection time, and decreases postoperative pain and stiffness. However, allografts introduce an added cost and carry the risk of disease transmission, although very low nowadays (43).
Different fixation methods have also been described: metal interference screws, bioabsorbable interference screws, suspensory fixation systems, screws and washers and staples. It has been well established that fixation methods are essential to limiting graft loosening and residual instability. The current literature for Achilles allografts recommends the use of metal interference screws for fixation of the bone plug. Screw-and-washer constructs are suggested to be used in osteopenic patients (35,44). The bioabsorbable interference screw is the most used fixation method (64% of the studies) (45).
In recent years, some authors have advocated the use of a synthetic systems that act like an internal bracing fixed by anchors to protect the posteromedial reconstructions or to assist in the healing of medial lesions not treated with repair or reconstruction techniques. The idea is that autographs have morbidity, allografts have some risk and economic disadvantages and bone tunnels for interference screw fixation sacrifice bone stock that would be precious in a multiligament setting (46).
Some biomechanical studies indicate that these devices have properties superior to simple repair and are equivalent to allograft reconstruction techniques (47). However few clinical informations are still present in literature, and randomized controlled trial are needed to eventually confirm benefits from these devices.
Outcomes and complications
The majority of the available studies in the literature are of level 4 evidence. Mean study quality, as evaluated by Modified Coleman Methodology Score (MCMS), is poor (45).
Most of the studies present heterogeneous study groups: different associated lesions, different postoperative protocols, different techniques. The superiority of one technique over another has not been demonstrated (48).
Recent systematic reviews show that the use of different techniques does not seem to influence the final outcome from the point of view of valgus laxity, ROM and clinical-functional scores assessed at a mean follow-up of 33 months (45).
With all the techniques described, there is a substantial improvement in the restoration of medial compartment laxity, IKDC objective and subjective scores and the Lysholm score. Only 2 out of 275 patients evaluated in the review by Varelas et al. (45). showed residual medial instability.
The most reported complication is alteration of the ROM, present in about 12% of the patients. Of these, 27.2% have a deficit of >6° of extension and 75.7% with a deficit of >10° of flexion (45).
The incidence rate of arthrofibrosis is higher in patients undergoing a single-stage multiple ligament reconstruction (e.g., MCL and ACL) than in patients undergoing a staged procedure (49,50). Although the tendency is to delay the reconstruction of grade III lesions associated with ACL lesions, there are studies showing that the acute repair of the MCL/PMC and a late reconstruction of ACL lead to coronal stability in 100% of cases with no patients complaining of a ROM deficit (28).
Moreover, with regard to multiligament lesions (more than two of the 4 major knee ligaments torn), there are contradictory studies in terms of failure and long-term PRO scores comparing patients who have undergone repair or reconstruction of the medial structures (51,52).
In this setting, patients undergoing ACL/MCL reconstruction exhibit higher functional scores than those undergoing PCL/MCL (44).
An infrequent complication described is calcification along the course of the sMCL, particularly at the level of its femoral insertion area. It is defined as the Pellegrini-Stieda syndrome and may show up in patients treated non-operatively as well as those undergoing repair or reconstruction of the medial structures. The deposition of calcium along the ligament leads to inelasticity of the structure and generates pain. There are numerous suggested therapeutic possibilities when facing this complication. They include local infiltrations, extracorporeal shock waves, roentgen therapy, release and surgical debridement.
Conclusions
The incidence of injuries on the medial side of the knee is the highest among all knee ligaments, mainly in the sports active population. Thanks to the intrinsic healing ability of the medial structures, most of these cases can be managed non-operatively. However, in the setting of multiligament injuries, grade III medial lesions should be properly recognized and treated to avoid residual instability or poor outcomes of the concomitant cruciate ligament reconstruction. Both for repair and reconstruction, a deep knowledge of the functional anatomy of each structure is crucial to restoring or reproducing the physiological biomechanics of the medial side of the knee. By strictly following this anatomy, several surgical techniques can be performed, depending on the surgeon’s preferences, as the superiority of any specific surgical technique has not been demonstrated. In any case, all the techniques have shown good results in terms of return to sport activity and subjective and objective scores.
Clinical randomized controlled studies indicating which approach should be followed in each specific case are still lacking.
Acknowledgments
We would like to thank Mr. Eric L. Goode for his help with the English correction.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.09.07). The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fanelli GC, Harris JD. Surgical treatment of acute medial collateral ligament and posteromedial corner injuries of the knee. Sports Med Arthrosc Rev 2006;14:78-83. [Crossref] [PubMed]
- Millett PJ, Wickiewicz TL, Warren RF. Motion loss after ligament injuries to the knee, part I: causes. Am J Sports Med 2001;29:664-75. [Crossref] [PubMed]
- Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am 1979;61:56-62. [Crossref] [PubMed]
- Robinson JR, Sanchez-Ballester J, Bull AM, et al. The posteromedial corner revisited. An anatomical description of the passive restraining structures of the medial aspect of the human knee. J Bone Joint Surg Br 2004;86:674-81. [Crossref] [PubMed]
- LaPrade RF, Engebretsen AH, Ly TV, et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000-10. [PubMed]
- Bonasia DE, Bruzzone M, Dettoni F, et al. Treatment of medial and posteromedial knee instability: indications, techniques, and review of the results. Iowa Orthop J 2012;32:173-83. [PubMed]
- Warren LA, Marshall JL, Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am 1974;56:665-74. [Crossref] [PubMed]
- Petersen W, Loerch S, Schanz S, et al. The role of the posterior oblique ligament in controlling posterior tibial translation in the posterior cruciate ligament-deficient knee. Am J Sports Med 2008;36:495-501. [Crossref] [PubMed]
- Roach CJ, Haley CA, Cameron KL, et al. The epidemiology of medial collateral ligament sprains in young athletes. Am J Sports Med 2014;42:1103-9. [Crossref] [PubMed]
- Najibi S. The use of knee braces, part 1: prophylactic knee braces in contact sports. Am J Sports Med 2005;33:602-11. [Crossref] [PubMed]
- Grant JA, Tannenbaum E, Miller BS, et al. Treatment of combined complete tears of the anterior cruciate and medial collateral ligaments. Arthroscopy 2012;28:110-22. [Crossref] [PubMed]
- Bauer KL, Stannard JP. Surgical approach to the posteromedial corner: indications, technique, outcomes. Curr Rev Musculoskelet Med 2013;6:124-31. [Crossref] [PubMed]
- Stannard JP. Medial and posteromedial instability of the knee: evaluation, treatment, and results. Sports Med Arthrosc 2010;18:263-8. [Crossref] [PubMed]
- Laprade RF, Bernhardson AS, Griffith CJ, et al. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med 2010;38:330-8. [Crossref] [PubMed]
- Miller MD, Osborne JR, Gordon WT, et al. The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med 1998;26:15-9. [Crossref] [PubMed]
- Tandogan NR, Kayaalp A. Surgical treatment of medial knee ligament injuries: Current indications and techniques. EFORT Open Rev 2017;1:27-33. [Crossref] [PubMed]
- Thornton GM, Johnson JC, Maser RV, et al. Strength of medial structures of the knee joint are decreased by isolated injury to the medial collateral ligament and subsequent joint immobilization. J Orthop Res 2005;23:1191-8. [Crossref] [PubMed]
- Wright R, Mackey RB, Silva M, et al. Smoking and mouse MCL healing. J Knee Surg 2010;23:193-9. [Crossref] [PubMed]
- Yoshiya S, Kuroda R, Mizuno K, et al. Medial collateral ligament reconstruction using autogenous hamstring tendons: technique and results in initial cases. Am J Sports Med 2005;33:1380-5. [Crossref] [PubMed]
- LaPrade RF, Goodrich LR, Phillips J, et al. Use of platelet-rich plasma immediately after an injury did not improve ligament healing, and increasing platelet concentrations was detrimental in an in vivo animal model. Am J Sports Med 2018;46:702-12. [Crossref] [PubMed]
- Derscheid GL, Garrick JG. Medial collateral ligament injuries in football. Nonoperative management of grade I and grade II sprains. Am J Sports Med 1981;9:365-8. [Crossref] [PubMed]
- Lundberg M, Messner K. Long-term prognosis of isolated partial medial collateral ligament ruptures. A ten-year clinical and radiographic evaluation of a prospectively observed group of patients. Am J Sports Med 1996;24:160-3. [Crossref] [PubMed]
- Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res 1990;174-7. [PubMed]
- Battaglia MJ 2nd, Lenhoff MW, Ehteshami JR, et al. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: a biomechanical evaluation in a cadaveric model. Am J Sports Med 2009;37:305-11. [Crossref] [PubMed]
- Engle CP, Noguchi M, Ohland KJ, et al. Healing of the rabbit medial collateral ligament following an O’Donoghue triad injury: effects of anterior cruciate ligament reconstruction. J Orthop Res 1994;12:357-64. [Crossref] [PubMed]
- Hara K, Niga S, Ikeda H, et al. Isolated anterior cruciate ligament reconstruction in patients with chronic anterior cruciate ligament insufficiency combined with grade II valgus laxity. Am J Sports Med 2008;36:333-9. [Crossref] [PubMed]
- Robins AJ. Newman Ap, Burks RT. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med 1993;21:20-5. [Crossref] [PubMed]
- Pandey V, Khanna V, Madi S, et al. Clinical outcome of primary medial collateral ligament-posteromedial corner repair with or without staged anterior cruciate ligament reconstruction. Injury 2017;48:1236-42. [Crossref] [PubMed]
- Stannard JP, Black BS, Azbell C, et al. Posteromedial corner injury in knee dislocations. J Knee Surg 2012;25:429-34. [Crossref] [PubMed]
- Phisitkul P, James SL, Wolf BR, et al. MCL injuries of the knee: current concepts review. Iowa Orthop J 2006;26:77-90. [PubMed]
- Benjamin Jackson J 3rd, Ferguson CM, Martin DF. Surgical treatment of chronic posteromedial instability using capsular procedures. Sports Med Arthrosc 2006;14:91-5. [Crossref] [PubMed]
- Van den Bogaerde JM, Shin E, Neu CP, et al. The superficial medial collateral ligament reconstruction of the knee: effect of altering graft length on knee kinematics and stability. Knee Surg Sports Traumatol Arthrosc 2011;19:S60-8. [Crossref] [PubMed]
- Coobs BR, Wijdicks CA, Armitage BM, et al. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med 2010;38:339-47. [Crossref] [PubMed]
- Wijdicks CA, Griffith CJ, Johansen S, et al. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am 2010;92:1266-80. [Crossref] [PubMed]
- Wijdicks CA, Michalski MP, Rasmussen MT, et al. Superficial medial collateral ligament anatomic augmented repair versus anatomic reconstruction: an in vitro biomechanical analysis. Am J Sports Med 2013;41:2858-66. [Crossref] [PubMed]
- Laprade RF, Wijdicks CA. Surgical technique: development of an anatomic medial knee reconstruction. Clin Orthop Relat Res 2012;470:806-14. [Crossref] [PubMed]
- Kim SJ, Lee DH, Kim TE, et al. Concomitant reconstruction of the medial collateral and posterior oblique ligaments for medial instability of the knee. J Bone Joint Surg Br 2008;90:1323-7. [Crossref] [PubMed]
- Gelber PE, Masferrer-Pino A, Erquicia JI, et al. Femoral tunnel drilling angles for posteromedial corner reconstructions of the knee. Arthroscopy 2015;31:1764-71. [Crossref] [PubMed]
- Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy 2002;18:E19 [Crossref] [PubMed]
- Lind M, Jakobsen BW, Lund B, et al. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med 2009;37:1116-22. [Crossref] [PubMed]
- Bonadio MB, Helito CP, Foni NO, et al. Combined reconstruction of the posterior cruciate ligament and medial collateral ligament using a single femoral tunnel. Knee Surg Sports Traumatol Arthrosc 2017;25:3024-30. [Crossref] [PubMed]
- Woo SL, Vogrin TM, Abramowitch SD. Healing and repair of ligament injuries in the knee. J Am Acad Orthop Surg 2000;8:364-72. [Crossref] [PubMed]
- Rihn JA, Groff YJ, Harner CD, et al. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg 2004;12:334-46. [Crossref] [PubMed]
- Rue JPH, Lewis PB, Detterline AJ, et al. Minimally invasive medial collateral ligament reconstruction using Achilles tendon allograft. Tech Knee Surg 2007;6:266-73. [Crossref]
- Varelas AN, Erickson BJ, Cvetanovich GL, et al. Medial collateral ligament reconstruction in patients with medial knee instability: a systematic review. Orthop J Sports Med 2017;5:2325967117703920 [Crossref] [PubMed]
- Lubowitz JH, MacKay G, Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech 2014;3:e505-8. [Crossref] [PubMed]
- Gilmer BB, Crall T, DeLong J, et al. Biomechanical analysis of internal bracing for treatment of medial knee injuries. Orthopedics 2016;39:e532-7. [Crossref] [PubMed]
- Madonna V, Screpis D, Condello V, et al. A novel technique for combined medial collateral ligament and posterior oblique ligament reconstruction: technical note. Knee Surg Sports Traumatol Arthrosc 2015;23:2814-9. [Crossref] [PubMed]
- Noyes FR, Berrios-Torres S, Barber-Westin SD, et al. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: a prospective study in 443 knees. Knee Surg Sports Traumatol Arthrosc 2000;8:196-206. [Crossref] [PubMed]
- Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res 1978;206-18. [PubMed]
- Hanley JM, Anthony CA, DeMik D, et al. Patient-reported outcomes after multiligament knee injury: MCL repair versus reconstruction. Orthop J Sports Med 2017;5:2325967117694818 [Crossref] [PubMed]
- King AH, Krych AJ, Prince MR, et al. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy 2016;32:1814-9. [Crossref] [PubMed]
Cite this article as: Gelber PE, Perelli S. Treatment of the medial collateral ligament injuries. Ann Joint 2018;3:78.