
Morbidity, mortality and cost of osteoporotic fractures—should proximal humerus fractures be taken as seriously as hip fractures?
Introduction
Proximal humerus fractures are a common orthopaedic injury in people over the age of 65. The incidence is approximately 250 per 100,000 Medicare patients making it the third most common insufficiency fracture (1). Due to the multiple comorbidities often present in patients in this age group, the mortality rate associated with this fracture is a concern (2).
Several studies have demonstrated high morbidity and mortality rates associated with certain osteoporotic fracture types such as hip fractures, distal radius fractures and vertebral compression fractures (3). This is likely not just attributable to the fracture itself, but rather may be representative of the poor overall health of the population that sustains them. This populations is generality frail and has been shown to be at increased risk for both injury as well as increase hospital length of stay and post-surgical complications (4). Jorgensen et al.’s registry study from Sweden suggests that the incidence of proximal humerus fractures and hip fractures are comparable (5). Similar to hip fractures, proximal humerus fractures have also been shown to be related to osteoporosis (6). However, no large studies exist evaluating if proximal humerus fractures carry the same risk factors, morbidity and mortality rates, and costs as the other three fracture types. This finding would be of clinical significance, as it has been shown that early detection and treatment for osteoporosis can reduce the risk of proximal humerus fractures and be cost effective (7). In addition, prevention of osteoporotic fractures and their associated morbidity and mortality has been shown to lower overall healthcare costs as well as Medicare expenditures.
The purpose of this study was to investigate and compare the risk factors, morbidity, mortality, and cost of proximal humerus, distal radius, hip and vertebral compression fractures in the Medicare population.
Methods
This was a level III retrospective cohort study. Prior to the start of this study, institutional review board approval was obtained.
From the Medicare Registry, insurance records from 2010 to 2014 were accessed to identify patients diagnosed with a proximal humerus, distal radius, hip or vertebral compression fracture based on ICD-9 coding for the admitting diagnosis. ICD-9 codes meeting inclusion criteria were: 812.00, 812.01, 812.02, 812.03, 812.09, 812.10, 812.11, 812.12, 812.13, and 812.19 for proximal humerus fracture, 813.42, 813.44, 813.45, 813.47, 813.52, 813.54, 813.81, 813.83, 813.91, and 813.93 for distal radius fracture, 820.00, 820.01, 820.02, 820.03, 820.09, 820.10, 820.11, 820.12, 820.13, 820.19, 820.20, 820.21, 820.22, 820.30, 820.31, 820.32, 820.8, 820.9, 733.14 and 905.3, for hip fracture, and 805, 805.4, 805.00, 805.01, 805.01, 805.03, 805.04, 805.05, 805.06, 805.07, 805.08, 805.2, 805.6, and 805.8 for vertebral compression fracture.
If the same patient was admitted multiple times for an osteoporotic fracture during the study period, the fracture type for each admission individually was recorded to determine if any patients suffered from multiple different subsequent fracture types.
From the patients who were admitted with these fractures, the following demographic and outcome data was collected: sex, race, age, Medicare status, fracture type, ICD-9 codes, healthcare cost, mortality during index admission, blood transfusion requirement, and number of comorbidities. Health care cost were determined from the Medicare database, which recorded the costs associated with the particular Medicare claim associated with the index admission. This number was used as the number for the health care cost. Specific comorbidities of interest include osteoporosis and osteopenia.
Statistical analysis
Descriptive statistics including mean, range, and standard deviation were calculated for all continuous variables. Ratios and percentages were calculated for the nominal variables.
The incidence of each fracture was calculated by dividing the number of people in the database with the specific fracture by the overall number of medicate database subjects. The mortality rate was calculated by diving the number of documented deaths associated with a specific fracture by the overall number of subjects who sustained a specific fracture. The incidence and mortality rate of proximal humerus fractures was compared with that of distal radius, hip, and vertebral compression fractures combined for all 5 years. In addition, the incidence and mortality rate of each fracture was calculated per year and trended over time. The Chi-squared analysis was used to compare sex, race, age, Medicare status, and mortality rate between the four fracture types. Analysis of variance (ANOVA) with a post-hoc Tukey test was used to compare the health care cost, number of blood transfusions, and comorbidities.
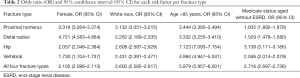
For all identified risk factors for the four fracture types, the odds rate (OR) with its 95% confidence interval (95% CI) was calculated and reported.
Data processing and analysis was performed using Statistical Package for the Social Sciences (SPSS) (version 20, IBM Corporation Armonk, New York, USA).
Results
Between 2010 and 2014 there were 50,237,330 inpatient claims and 1,183,966 (2.4%) of those were specifically for 1 of the 4 osteoporotic fracture types. Of these patients 88,861 (7.5%) sustained a proximal humerus fracture, 34,217 (2.9%) a distal radius fracture, 876,697 (74.0%) a hip fracture, and 184,191 (15.6%) a vertebral compression fracture. From the 1,183,966 total admissions for an osteoporotic fracture, 101,946 (8.6%) patients were admitted more than once. This was twice in 93,666 patients (91.9%), three times in 7,376 (7.2%) and 4 to 8 times in 782 (0.8%).
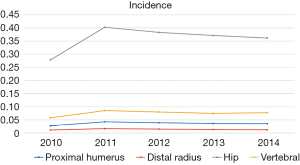
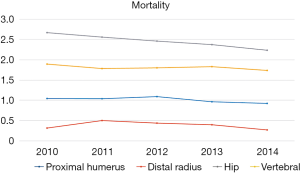
Most patients with an osteoporotic fracture were female (850,653 subjects, 71.8%), white (1,089,769 subjects, 92.0%) and age 85 or older (506,781 subjects, 42.8%) (Table 1). Mortality during index admission for all four fractures combined was 2.2%. For proximal humerus fractures mortality rate was 1%, as compared to 0.4% for distal radius, 2.5% for hip, and 1.8% for vertebral compression fractures. The incidence and mortality rate for each fracture per year can be referenced in Figures 1,2.
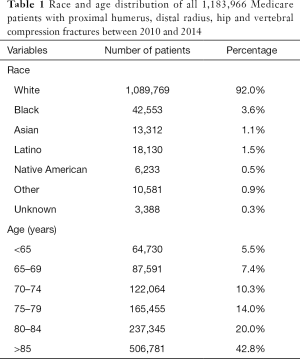
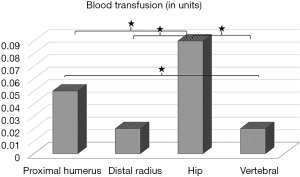
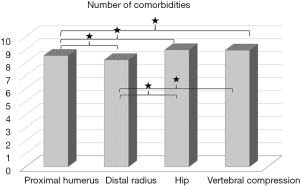
Full table
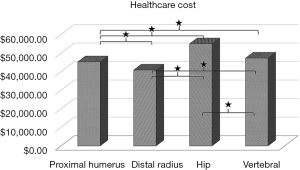
There was a significant difference between all four fracture types with regards to health care cost (P<0.001 for all comparisons), with the highest cost associated with hip fractures and the lowest cost with distal radius fractures (Figure 3). The number of required blood transfusions was also greatest in the hip fracture cohort as compared to any of the other three fracture types (P>0.001 for all comparisons). Number of transfusions was greater in proximal humerus fractures compared to vertebral compression fractures (P=0.011) (Figure 4). The hip and vertebral compression fracture patients had the most documented comorbidities (P<0.001 for all comparisons) (Figure 5). Only 5.4% of patients had received an additional diagnosis of osteoporosis or osteopenia with no difference in this between the fracture types. For all fracture types, patients were more likely to be female, white, and 85 years of age or older and receiving Medicare due to advanced age, and were without associated end-stage renal disease (ESRD). The odds ratios for the identified risk factors for the four fracture types can be found in (Table 2)
Full table
Discussion
The results of this study demonstrate that the incidence, mortality and health care costs of proximal humerus fractures lie somewhere between that of distal radius fractures (lower) and vertebral compression and hip fractures (higher). Blood transfusion was most common in proximal humerus and hip fractures, most likely because these are more frequently treated with surgery and because tourniquet use is not applicable for these cases. Although there was a statistically significant difference in comorbidities between the fracture types, all of them had on average between 7 and 9 concomitant diagnoses. The risk for all four fractures was highest in white, female patients age 85 or older.
These findings are consistent with previously published literature. A study from the United Kingdom identified 629 patients treated at a single trauma center with a proximal humerus fracture. Their study indicated that most of these fractures occurred in women (82%). Mortality rate at 1 year was as high as 10% (8). Mortality rate in the present study was 1%, but this was only mortality during the index admission. The study from the United Kingdom also assessed clinical outcome which indicated that over 25% of patients had poor functional outcomes. This was increasingly so when they were unable to return to their own home, participate in recreational activities, perform their own shopping, or dress themselves (8).
A study on 569 trauma patients over the age of 65, showed that distal radius fractures and proximal humerus fractures were the most common in a level I trauma center. Hip and proximal humerus fractures were associated equally with mortality rate (9). In addition, fractures specifically associated with mortality also included proximal humerus fractures (9). A study on the incidence and mortality of distal radius fractures in the Korean population showed that incidence was 0.47%, as compared to 0.01% in the present study. Mortality rate in their study was 1.4%, compared to 0.4% in the present study (3). This is consistent with prior literature which suggests that osteoporosis rates are higher in Korea than in the United States, possibly related to lower body mass index (BMI) as well as socio-economical and nutritional differences (10). Similar to the present study, a previously published study also suggests that white, elderly females are at increased risk for mortality in the context of fracture (11). Interestingly, in that study, if men did sustain a distal radius fracture, they were 2.65 times more likely to die than women (95% CI: 1.31–5.36).
A Medicare database study on vertebral compression fractures between 1997 and 2004 estimated the 3-, 5- and 7-year survival after diagnosis to be 53.9%, 30.9%, and 10.5% respectively (12). This appears high when compared to the 1.8% mortality rate during admission found in the present study. Improvement in treatment modalities over the past two decades could explain this disparity. A more recent study showed the standardized mortality rate after vertebral compression fractures to be highest during the first 3 months after injury, with gradual decline in mortality rate to 2.53% in men and 1.86% in women at 2 years (13).
Although in the present study it was not possible do distinguish between those subjects treated with or without surgery, several other studies have reported on this. A recent study reported the post-operative mortality after fixation of proximal humerus fractures to be 3.5% (14). Risk factors for mortality were a higher Charlson comorbidity index (OR =1.5), male sex (OR =1.7), and patient age of 75 years or older (OR =3.6) (14). Hardeman et al. showed a 15.3% failure rate and re-operation rate of 23.8% at 4.3 years in their cohort of 368 surgically treated proximal humerus fractures (15). Outcomes of surgery have been shown to be negatively affected by the presence of low local bone mineral density. Similar to hip fractures, a study on proximal humerus fractures showed that delaying surgery is associated with increased inpatient morbidity, postoperative length of stay, and non-routine discharge (16).
For distal radius fractures treated operatively, the complication rate was 3%. That study evaluated different risk factors than the present study and showed that American Society of Anesthesiologists (ASA) class III or IV, dependent functional status, hypertension, and myocardial infarction/congestive heart failure were risk factors for any early complication (17). Interestingly, surgical management in patients with a vertebral compression fracture lowered the morbidity and improved the survival rates in several studies (18). However, there are also studies demonstrating no difference, as long as only symptomatic subjects were treated surgically (19).
The present study does have limitations. First, it does not contain any information from private insurances, does not include patients from a Medicare managed-care plan, or include patients treated for 1 of the 4 fracture types in an outpatient setting. However, the results are likely generalizable to the geriatric population, as most of the population over the age of 65 in the United States is enrolled in Medicare and because the large number of patients in this database allows sufficient statistical power for significant conclusions. However, some a small number of Medicare patients may receive this while under the age of 65 and the database did not provide a lower age limit for this small subset of patients. In addition, age is not synonymous with osteoporosis as some younger patients will have osteoporotic fractures and some older ones may have non-osteoporotic fractures. Second, although it was possible to determine if the same patient was admitted multiple times, it was not possible to definitively say if this was for the same fracture or a different one. This is largely due to the use of ICD-9 instead of ICD-10 in the Medicare database, which does not include laterality. For example, if a patient was admitted for a “proximal femur fracture” in 2010 and also in 2012, it was not possible to determine if this was still the same fracture, a new fracture in the same extremity or a new fracture in the contralateral extremity. With regards to health care cost, the database only recorded health care costs associated with that particular Medicare claim. It was not possible to discern if those costs were associated with a surgery. Nor did the database document whether patients were treated conservatively of surgically for any of the fractures. In addition, the database did not document the reason for or timing of the blood transfusion. Therefore, it is not possible to discern whether a blood transfusion was the result of a surgery, or a preexisting comorbidity. Lastly, the calculated mortality rate only describes mortality during the hospital admission. As a result, the mortality rate presented in this study for all fractures may significantly underestimate both the 1-year and overall mortality rates associated with these fractures. However, this circumstance was the same for all included patients. Therefore, although the numbers underestimate the 1-year and overall mortality, they are comparable amongst fracture types in this study.
The findings of the present study are clinically relevant, as life expectancy continues to increase and the Medicare population continues to grow. This will undoubtedly lead to an increase in the incidence of osteoporotic fractures (20). However, only 5.4% of patients in the present study had received additional diagnosis of osteoporosis or osteopenia during their admission for their fracture. This while there is strong evidence to suggest that with proper screening and treatment of osteoporosis, some of these fractures can be prevented (21). Moreover, the first fragility fracture that brings us the osteoporotic patient is the better chance to prevent a future one. Health care cost for proximal humerus fractures in the present study lay somewhere in the middle between the cost of hip and distal radius fractures. Reducing proximal humerus fractures and their associated morbidity and mortality may effectively reduce health care and Medicare costs (21).
Conclusions
In conclusion, the incidence, mortality rate and health care costs of proximal humerus fractures were higher than that of distal radius fractures, but lower than that of vertebral compression and hip fractures. Blood transfusion was most common in proximal humerus and hip fractures. Caucasian race, female sex and an age over 85 were risk factors for all four fracture types.
Acknowledgments
Funding: None.
Footnote
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.01.01). JMI: Acumed LLC: paid consultant, paid presenter/ speaker, research support; Arthrex Inc: paid consultant, paid presenter/ speaker; Tornier: royalties, paid presenter/ speaker. CF van Eck serves as an unpaid editorial board member of Annals of Joint from Jul 2018 to Jun 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Asentral, Inc. Institutional Review Board (IRB number 2015-366A). Individual consent for this retrospective study was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Calvo E, Morcillo D, Foruria AM, et al. Nondisplaced proximal humeral fractures: high incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg 2011;20:795-801. [Crossref] [PubMed]
- Kannus P, Palvanen M, Niemi S, et al. Osteoporotic fractures of the proximal humerus in elderly Finnish persons: sharp increase in 1970-1998 and alarming projections for the new millennium. Acta Orthop Scand 2000;71:465-70. [Crossref] [PubMed]
- Kwon GD, Jang S, Lee A, et al. Incidence and Mortality after Distal Radius Fractures in Adults Aged 50 Years and Older in Korea. J Korean Med Sci 2016;31:630-4. [Crossref] [PubMed]
- Kistler EA, Nicholas JA, Kates SL, et al. Frailty and Short-Term Outcomes in Patients With Hip Fracture. Geriatr Orthop Surg Rehabil 2015;6:209-14. [Crossref] [PubMed]
- Jørgensen TS, Hansen AH, Sahlberg M, et al. Falls and comorbidity: the pathway to fractures. Scand J Public Health 2014;42:287-94. [Crossref] [PubMed]
- Lee SH, Dargent-Molina P, Breart G, et al. Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study. J Bone Miner Res 2002;17:817-25. [Crossref] [PubMed]
- Nayak S, Roberts MS, Greenspan SL. Impact of generic alendronate cost on the cost-effectiveness of osteoporosis screening and treatment. PLoS One 2012;7:e32879 [Crossref] [PubMed]
- Clement ND, Duckworth AD, McQueen MM, et al. The outcome of proximal humeral fractures in the elderly: predictors of mortality and function. Bone Joint J 2014;96-B:970-7. [Crossref] [PubMed]
- Keller JM, Sciadini MF, Sinclair E, et al. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma 2012;26:e161-5. [Crossref] [PubMed]
- Kim MH, Lee JS, Johnson MA. Poor Socioeconomic and Nutritional Status Are Associated with Osteoporosis in Korean Postmenopausal Women: Data from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES) 2009. J Am Coll Nutr 2015;34:400-7. [Crossref] [PubMed]
- Shauver MJ, Zhong L, Chung KC. Mortality after distal radial fractures in the Medicare population. J Hand Surg Eur Vol 2015;40:805-11. [Crossref] [PubMed]
- Lau E, Ong K, Kurtz S, et al. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am 2008;90:1479-86. [Crossref] [PubMed]
- Lee YK, Jang S, Jang S, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int 2012;23:1859-65. [Crossref] [PubMed]
- Petrigliano FA, Bezrukov N, Gamradt SC, et al. Factors predicting complication and reoperation rates following surgical fixation of proximal humeral fractures. J Bone Joint Surg Am 2014;96:1544-51. [Crossref] [PubMed]
- Hardeman F, Bollars P, Donnelly M, et al. Predictive factors for functional outcome and failure in angular stable osteosynthesis of the proximal humerus. Injury 2012;43:153-8. [Crossref] [PubMed]
- Menendez ME, Ring D. Does the timing of surgery for proximal humeral fracture affect inpatient outcomes? J Shoulder Elbow Surg 2014;23:1257-62. [Crossref] [PubMed]
- Schick CW, Koehler DM, Martin CT, et al. Risk factors for 30-day postoperative complications and mortality following open reduction internal fixation of distal radius fractures. J Hand Surg Am 2014;39:2373-80.e1. [Crossref] [PubMed]
- Edidin AA, Ong KL, Lau E, et al. Morbidity and Mortality After Vertebral Fractures: Comparison of Vertebral Augmentation and Nonoperative Management in the Medicare Population. Spine (Phila Pa 1976) 2015;40:1228-41. [Crossref] [PubMed]
- McDonald RJ, Achenbach SJ, Atkinson EJ, et al. Mortality in the vertebroplasty population. AJNR Am J Neuroradiol 2011;32:1818-23. [Crossref] [PubMed]
- Krause O, Junius-Walker U, Wiese B, et al. Are even geriatric patients becoming older and older?: Changes in the age structure of geriatric inpatients in the course of two decades. Z Gerontol Geriatr 2018;51:81-4. [Crossref] [PubMed]
- Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012;CD007146 [PubMed]
Cite this article as: van Eck CF, Klein CM, Rahmi H, Scheidt KB, Schultzel M, Lee BK, Itamura JM. Morbidity, mortality and cost of osteoporotic fractures—should proximal humerus fractures be taken as seriously as hip fractures? Ann Joint 2019;4:3.


