
Three-dimensional bioprinting for bone and cartilage transplantation
Introduction
Additive manufacturing, which is also termed three-dimensional (3D) printing technology, is driving innovations in various fields, including manufacturing, healthcare, engineering, art, service, and medicine (1). Recently, advances have made 3D printings using by biocompatible materials feasible, and tissue regeneration studies are currently focused on printing additive cells and supporting components into complicated 3D functional tissues (2). Especially, for clinical applications, 3D printing, as a novel manufacturing technique, is being applied mainly in orthopedics. Recently, 3D printing-based, patient-specific surgical and dental implants were approved by the United States Food and Drug Administration and Caritas Europa for clinical use (3).
3D bioprinting is considered a useful method in tissue engineering because of its effective control over scaffold fabrication and cell distribution. The 3D printing technology was first mentioned at 1986 by C. Hull, who named it “stereolithography”. In his design, thin layers of some materials cured using ultraviolet (UV) light were sequentially were built layer-by-layer to form a 3D structure (1). This technology has been used to create resin molds for 3D scaffolds made from biomaterials. Water soluble systems allows the additive manufacturing of biological materials, including growth factors and peptides, into 3D structures that could be transplanted directly, with or without cells (4). The following step is 3D bioprinting procedure as a method of tissue engineering for additive manufacturing technology, materials engineering, and cell biology. 3D bioprinting could also be used to produce patient-specific medical devices, such as splints and stents (5).
For use in orthopedic surgery, 3D printing faces considerable challenges in cases of injuries that feature multiple bone fragmentation, as well as bone deformities. X-ray imaging is used routinely for orthopedic surgical planning. Yet, X-rays can provide inadequate information concerning the precise spatial lesion of bone defects (6). In spite of the advances in 3D anatomical reconstructions, the ex vivo 3D-printed product cannot perfectly match the defective lesion that needs to be regenerated. Current animal studies are based on an experimental bone defect model that can be filled with a scaffold that adopts the exact shape and dimensions (6). However, this is not the case clinically and although more defined defects can be generated (such as the ones made for mosaicplasty), this is not ideal as it further increases the area that needs to be repaired.
In addition, many studies have reported high molecular weight materials, such as poly-lactic-co-glycolic acid (PLGA), poly-lactic acid (PLA), and polycaprolactone (PCL), which are mixed with hydrogels to generate 3D printable materials that are compatible with cartilage component and cells (7). Although this research is rapidly growing, in vivo data of the capability of 3D printed material to reconstruct cartilage tissue are very limited (8). In particular, maintaining the long-term stability of the implanted tissue remains the major unresolved barrier.
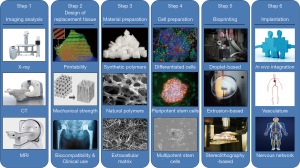
Bioprinting 3D tissues typically involve imaging, design, material selection, cell selection, bioprinting, and implantation steps (Figure 1) (1). Imaging of the defected lesion and its environmental situation can be used for design of 3D-bioprinted tissues. The choices of biomaterials and cells are essential and specific to the formation and function of the tissue or organ, and these components have to integrate with bioprinting systems. Some tissues and organs may require maturation through in vitro culture before transplantation.
Here, we review the typical procedure for 3D bioprinting of bone or cartilage for transplantation in orthopedic surgery. We also discuss a stepwise procedure for regenerating a complicated tissue, and present advances of 3D bioprinting technology for bone and cartilage regeneration.
Imaging analysis
The first step for 3D bioprinting is the generation of a medical image by the extraction of the target geometry from the patient. The imaging segmentation process make partition with an image area into non-overlapping connected regions that are homogeneous with respect to certain signal characteristics (9). Applicable noninvasive imaging modalities include magnetic resonance imaging (MRI) and computed tomography (CT). Computer-aided manufacturing (CAM) and tools computer-aided design (CAD) are also used to gather and digitalize the complex tomographic information of tissues and organ (10). The 3D image is divided into horizontal or vertical slices that can be imported into the 3D printer system for additive deposition (11).
Main objective in the imaging process is to reduce the noise in the original image, leaving a comprehensive representation of the target characteristics. The difficulty of image partitioning depends on the degree of complexity. Image segmentation from diagnostic devices, such as MRI and CT, should end when the target lesion has been located. Actually, the image segmentation consists of assigning a label to each pixel, which is a component of a particular group (12). Classification using several segmentation algorithms has been described. All involve modifications of the anatomical analysis, therefore, the choice of the optimal way depends on the characteristics of the material characteristics (6).
A variety of commercial software enables medical image segmentation. The image segmentation procedure of each step starts from the appointment of a gray scale including all of the gray shades in target (13). The next step is to indicate one or more starting points in the images, which are curved surfaces where the algorithm will begin. The algorithm will develop within and through every slice till the user stops. If the structure or surfaces contrast well represented with its surroundings, the algorithm could be allowed to evolve until the region is identified without any further contrast (14). The processing depends on many parameters, including an expanded factor which can control the acting forces inwards and outwards on the imaging segmentation surface, and a curvature factor that can control how the 3D modeling surface loses its sphere shape and adapts to the detail 3D image (6). With complete algorithm process, the result is a 3D surface. The virtual 3D model can be navigable whenever and wherever a user interacts with it, with modification of the transparency or colors of 3D modeling, as are complex views of the interactions in the anatomical structures (15). The final process of imaging involves the transformation of the optimal format for subsequent 3D printing.
The global standard for 3D printing process is the standard triangulation language file format. This format represents a geometric of the target through the mesh, such as a series of triangles or honeycomb structures. Increasing numbers of oriented triangles generates an increasingly better surface quality object. In order to use in clinic, additional post-processing of the final 3D clinical imaging, such as removing noise, will be needed.
Design of replacement tissue
The raw data from the clinical image requires imaging modalities. Thus, the imaging process has to pass through tomographic reconstruction to generate cross-sectional images. In this process, the 3D design of replacement tissue from clinical imaging process can be produced for further modification (16). This process is described as the changes from an analytical anatomy to a synthetic anatomy (17). A method to produce 3D modeling of tissue structures is CAD-CAM and 3D modeling. This 3D modeling produces views of tissue structure while retaining the voxel information from clinical raw image that can be used for volume rendering and 3D imaging representation. Imaging reconstruction can be represented in various ways, such as wire-frame models, contour stacks, and solid and shaded model (18).
To generate an accurate design of artificial tissue from the imaging analysis, two-dimensional (2D) cross-sections and 3D representations could be applied for 3D bioprinting. Alternative speaking, a direct copy of patient’s tissue may not be desirable and economically feasible. In these cases, data-based modeling may contribute to establish the structure of anatomical design (19). Additionally, computer modeling based on a patient’s data can help predicting the biochemical and biomechanical properties of fabricated tissue manufacture (20,21). X-ray, CT, and MRI imaging have been used to provide accurate data of tissue dimensions and volume for the design of 3D printing constructs.
The 3D modeling of patient tissue is interfaced with 3D bioprinting systems through numerical control for protoprinting. This method is established by reversing from 2D to 3D reconstruction of which the 3D modeling is divided into horizontal or vertical slices that are imported to the 3D bioprinting system. The structure containing the data of the 2D horizontal slices provides instructions for the layer by layer deposition (22). In addition, variations in the 3D bioprinting technique affects design of tissue. Some 3D bioprinting systems continuously deposit materials to form 3D structure. Another systems deposit two or three materials in extra spaces.
The 3D printing design has to be considered with four major principles for selection (23). Firstly, the biomaterials for 3D printing should have optimal properties to set the specific 3D bioprinter requirements, known as printability, which means the capability of the biomaterial to support manufacturing hardness. The interrelation of biomaterials and substrates must be investigated to accurate manufacture. Secondly, biomaterials have to possess appropriate mechanical and physical characteristics, including wetting and swelling properties, degradation kinetics, internal and external structures ranging from the nano to macro scale, and structural stability. Thirdly, biological activity and biocompatibility must be considered the development and remodeling of tissues over long-term in vivo implantation. The biomaterial should provide engraftment with the endogenous tissue without any immune response, as well as a spectrum of biochemical cues such as growth factors, chemokines, and signaling proteins, which could affect cell motility, proliferation, and differentiation. Finally, the biomaterials should be affordable and readily available commercially with suitable regulations for clinical use.
Material preparation
3D bioprinting is an additive manufacturing process of laying-down successive materials, which include PLA, PLGA, and PCL, to fabricate physical objects from digital design, usually layer-by-layer, until the objects are created (24). In addition, ceramics like β-tricalcium phosphate (β-TCP) and hydroxyapatite (HA) are preferred for bone reconstruction. Bone graft substitutes are usually made from a composite of PLGA, PCL, and β-TCP. An effort to improve the biological function of 3D-printed synthetic scaffolds involves ornamentation with extracellular matrix (ECM) from the patient’s tissue. The objective of tissue engineering is to lead to the repair and regenerate bone defects using a matrix scaffold as a platform to retain the indicated cells or therapeutic agents at the lesion site. The optimal scaffold has a similar complex of mechanical and biochemical properties as the native human tissue. To obtain these properties, construct must have a proper architecture favoring the flow of oxygen and nutrients for proliferation and differentiation of involved cells. It must possess osteoconductivity and be able to support cells through a suitable surface chemistry.
For cartilage bioprinting, the archiving of chondrocytes and stem cells encapsulated within alginate hydrogels is an attractive approach, since the cells retain their viability and metabolic activity (25). The main obstacle of the use of hydrogels for cartilage bioprinting is the difficulty in maintaining a uniform 3D structure. To avoid this problem, hydrogels should be mixed with synthetic biomaterials such as PGA, PCL, and HA (7). A combination of hydrogel, alginate-gelatin, and HA can be printed with a stable 3D architecture for bone and cartilage regeneration. This mixture allows living human mesenchymal stem cells to be added to the biomaterials. This method has reportedly maintained cell viability after 3 days of in vitro culture despite the printing process and complete cross-linking synthesis (26).
Cell preparation
The 3D bioprinting technique accept the creation of novel constructs that lead to the precise deposition of cells to create an environment that is similar to native human tissue. The choice of cells for 3D bioprinting is critical for the proper function of the fabricated architecture. Whatever the specification of the 3D bioprinting method—whether the cells are combined with other biomaterials or are printed directly layer-by-layer on a construct or scaffold—the rate-limitation depends on the number of prepared cells (27). The optimum number of involved cells depends on the case of 3D bioprinter, and can range from 1×106 to 1×108 cells per mL (28). A large number of cells are required to synthesize the ECM support and enable the function of the construct. In addition, most tissues containing cells that provide supportive functions are involved in vascularization and nerve generation, or provide a niche for stem cell proliferation and differentiation. Current options of 3D bioprinting with cells involve either the deposition of multiple cell types into a complex that faithfully represents the native human tissue or the printing of stem cells that can proliferate and differentiate (29).
Cells for 3D bioprinting should possess several properties (30). The first is a sufficient number of cells that can be expanded during in vitro culture. The second is cells that are sufficiently robust to survive the printing process. The third is optimal properties of cell proliferation and differentiation in the scaffolds for either in vitro culture or in vivo implantation. The fourth is the ability to maintain cellular functions during in vitro culture and proliferate/differentiate after implantation by stimulation with the native surrounding, including growth factors or physical forces. The fifth is the structural and functional characteristics of the different cell types. The last is the interaction with multiple cell types for tissue development involving various biological signaling pathways.
The prolonged expansion and passage of cultured cells can result in the dedifferentiation of cells, and can affect cell physiology and genomic stability. Genomic and phenotypic changes as consequences of cell expansion lead to loss of cell function (31). Identification of the optimal cell type and functionality result in the successful production and maintenance of a printed matrix as cells are specifically selected for their ability to synthesize a matrix that will offer integrity and robustness to architecture. Therefore, it is necessary to identify the cell type and functionality by investigation of properties like genomic state, phenotype, cell activity, and metabolism.
Bioprinting
3D bioprinting involves cells alive during the matrix fabrication process with the advantages of fast prototyping. Various printing technology has been developed to make up 3D networks of living tissue. Each has different restriction in terms of the available properties, which include printing speed, resolution, biological materials, and cell activity. The established technologies for 3D bioprinting used for deposition and patterning of involved materials are droplet-based, extrusion-based, and stereolithography. The different characteristics of these techniques have to be considered in light of the most critical factors in 3D bioprinting, which are cell viability, the involved materials and surface resolution (1,32).
Droplet-based bioprinting depends on diverse energy sources (electric, thermal, laser beam, acoustic, or pneumatic mechanisms) to deposit the microdroplets of biomaterial with living cells in high-throughput manners (33). Advantages are its simple characteristics and agility with precise control of biological components, including growth factors and cells for tissue regeneration. In addition, it is the most common method for pharmaceutical use because of its simplicity, versatility, and high-throughput capability.
Extrusion-based (direct writing or dispensing) 3D bioprinting, that originated from fused deposition printing, is used in mechanical, pneumatic, or electric systems to deposit cells and biomaterials using a “needle-syringe” format. During 3D bioprinting process, materials are precisely dispensed by the deposition system to print the cell-laden filaments and form the desired 3D architecture.
Stereolithography-based (vat photo-polymerization) 3D bioprinting employs laser beam to deposit the cell-laden biomaterial in a reservoir through beam scanning, allowing the molding of high-resolution patterns. Advantages include the precise control of the deposition of biological components and the very precise patterning.
Implantation
After the in vitro development of 3D architecture, the manufactured tissue would be implanted into the patient’s body for integration with another tissue or organ. This step involves immune acceptance, efficacy, and safety, and monitoring of the integrity and function of the 3D architecture after implantation. The most common and critical challenge is the integration with vascular and nervous networks in the 3D-printed architecture.
Endothelial cells and smooth muscle cells have been encapsulated in 3D bioprinted constructs without perfusable channels for the self-assembly of connected vascular (34). This process, which has been used to generate blood vessels in manufactured tissues, depends on the activities of endothelial cells to organize the blood vessels autonomously. Although designs of the implanted tissue lead to the formation of the vascular architecture, sometimes capillaries may be located too far from the arteriovenous loop, and the implanted tissue can be prone to necrotic process. In addition, from a 3D bioprinting standpoint, fabrication of the capillaries does not have to be considered, due to sprout from blood vessels based on endogenous angiogenesis, which is stepwise process of events that includes endothelial cell activation, migration, proliferation, and arrangement.
The human nervous system is widely distributed throughout the body. It controls the processes that coordinate voluntary actions, as well as the transfer of signals to different regions. Overall, regeneration of nervous networks means the involvement of a neural scaffold or conduit fabricated in vitro to the target site. The neural scaffold offers a direct framework for neurons to proliferate and secrete the inductive factors needed for axonal elongation. In the living body, neuronal cell resides within the 3D-ECM with micro- and nano-structures, and spatiotemporal physical and chemical cues. A conventional scaffold provides restrict control over geometry, especially for the oriented feature. The various 3D bioprinting techniques have allow more control over the internal structure and surface shape of the conduits, and has large potential for replicating the complicated nervous network.
Limitations of 3D bioprinting for clinical use
Bone and cartilage 3D bioprinting studies are exploding. Still, there is a paucity of in vivo data concerning the capability of 3D bioprinted constructs to regenerate bone and cartilage tissue. Especially, the long-term stability of the implanted tissue remains a formidable obstacle. Few studies have investigated the superiority of these techniques for clinical strategies. Thus, we are far from the clinical use of 3D bioprinting constructs. One of the critical problems is the difficulty in gaining ethical approval for the harvesting of stem cells from patients and their expanded proliferation in the laboratory environment, as well as their subsequent use in surgery. This “bench-to-bedside” application of stem cells for therapeutic use remains more theoretical than real. There are obstacles to overcome before the discoveries made in the laboratory can be safely and successfully translated to clinical use (35,36). Another problem is the matching of a bench-based 3D bioprinted product to what is needed during surgery. In spite of the advances in 3D anatomic reconstructions, in vitro printed construct cannot perfectly match the lesion defect that is the focus of repair. Many recent studies have involved the creation of regular defects that are subsequently filled with a 3D printed scaffold having the exact desired shape and dimensions (36). However, in the clinical setting, although more defined defects can be created, this is not ideal, as it further increases the area that needs to be repaired.
Conclusions
Orthopedics and maxillofacial surgery were the first medical fields to use 3D printing technology. While there have been successes, the need remains for a printing system that can be used directly by the surgeon in real-time during the surgical procedure. This direct tissue engineering using 3D bioprinting techniques in bone and cartilage regeneration would avoid some of the laboratory-based manipulations that are now required. There are ethical and technical challenges to this goal. Moreover, using a single approach that avoids two or more surgical interventions would increase patient compliance and hasten recovery.
Although there are challenges to overcome for the use of 3D bioprinting in bone and cartilage regeneration, further multidisciplinary exploration and refinement of printing techniques, printable biomaterials, and 3D designs will hopefully realize the emerging potential of 3D tissue and organ bioprinting in the orthopedic and traumatology fields.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Young Lae Moon) for the series “Medical 3D Application in Orthopaedics” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2018.12.06). The series “Medical 3D Application in Orthopaedics” was commissioned by the editorial office without any funding or sponsorship. YLM served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from Aug 2017 to Jul 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol 2014;32:773-85. [Crossref] [PubMed]
- Derakhshanfar S, Mbeleck R, Xu K, et al. 3D bioprinting for biomedical devices and tissue engineering: A review of recent trends and advances. Bioact Mater 2018;3:144-56. [Crossref] [PubMed]
- Honigmann P, Sharma N, Okolo B, et al. Patient-Specific Surgical Implants Made of 3D Printed PEEK: Material, Technology, and Scope of Surgical Application. Biomed Res Int 2018;2018:4520636 [Crossref] [PubMed]
- Nakamura M, Iwanaga S, Henmi C, et al. Biomatrices and biomaterials for future developments of bioprinting and biofabrication. Biofabrication 2010;2:014110 [Crossref] [PubMed]
- Zopf DA, Hollister SJ, Nelson ME, et al. Bioresorbable airway splint created with a three-dimensional printer. N Engl J Med 2013;368:2043-5. [Crossref] [PubMed]
- Auricchio F, Marconi S. 3D printing: clinical applications in orthopaedics and traumatology. EFORT Open Rev 2017;1:121-7. [Crossref] [PubMed]
- Di Bella C, Fosang A, Donati DM, et al. 3D Bioprinting of Cartilage for Orthopedic Surgeons: Reading between the Lines. Front Surg 2015;2:39. [Crossref] [PubMed]
- Kundu J, Shim JH, Jang J, et al. An additive manufacturing-based PCL-alginate-chondrocyte bioprinted scaffold for cartilage tissue engineering. J Tissue Eng Regen Med 2015;9:1286-97. [Crossref] [PubMed]
- Pham DL, Xu C, Prince JL. Current methods in medical image segmentation. Annu Rev Biomed Eng 2000;2:315-37. [Crossref] [PubMed]
- Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010;5:335-41. [Crossref] [PubMed]
- Cui H, Nowicki M, Fisher JP, et al. 3D Bioprinting for Organ Regeneration. Adv Healthc Mater 2017;6: [Crossref] [PubMed]
- Bezdek JC, Hall LO, Clarke LP. Review of MR image segmentation techniques using pattern recognition. Med Phys 1993;20:1033-48. [Crossref] [PubMed]
- McInerney T, Terzopoulos D. Deformable models in medical image analysis: a survey. Med Image Anal 1996;1:91-108. [Crossref] [PubMed]
- Chen L, Wu LY, Wang Y, et al. Revealing divergent evolution, identifying circular permutations and detecting active-sites by protein structure comparison. BMC Struct Biol 2006;6:18. [Crossref] [PubMed]
- Pietrabissa A, Marconi S, Peri A, et al. From CT scanning to 3-D printing technology for the preoperative planning in laparoscopic splenectomy. Surg Endosc 2016;30:366-71. [Crossref] [PubMed]
- Tong S, Alessio AM, Kinahan PE. Image reconstruction for PET/CT scanners: past achievements and future challenges. Imaging Med 2010;2:529-45. [Crossref] [PubMed]
- Mironov V, Trusk T, Kasyanov V, et al. Biofabrication: a 21st century manufacturing paradigm. Biofabrication 2009;1:022001 [Crossref] [PubMed]
- Sun W, Lal P. Recent development on computer aided tissue engineering--a review. Comput Methods Programs Biomed 2002;67:85-103. [Crossref] [PubMed]
- Hollister SJ. Porous scaffold design for tissue engineering. Nat Mater 2005;4:518-24. [Crossref] [PubMed]
- Peltola SM, Melchels FP, Grijpma DW, et al. A review of rapid prototyping techniques for tissue engineering purposes. Ann Med 2008;40:268-80. [Crossref] [PubMed]
- Hutmacher DW, Sittinger M, Risbud MV. Scaffold-based tissue engineering: rationale for computer-aided design and solid free-form fabrication systems. Trends Biotechnol 2004;22:354-62. [Crossref] [PubMed]
- Ozbolat IT, Yu Y. Bioprinting toward organ fabrication: challenges and future trends. IEEE Trans Biomed Eng 2013;60:691-9. [Crossref] [PubMed]
- Park JH, Jang J, Lee JS, et al. Three-Dimensional Printing of Tissue/Organ Analogues Containing Living Cells. Ann Biomed Eng 2017;45:180-94. [Crossref] [PubMed]
- Jammalamadaka U, Tappa K. Recent advances in biomaterials for 3D printing and tissue engineering. J Funct Biomater 2018;9:22. [Crossref] [PubMed]
- Khalil S, Sun W. Bioprinting endothelial cells with alginate for 3D tissue constructs. J Biomech Eng 2009;131:111002 [Crossref] [PubMed]
- Wüst S, Godla ME, Muller R, et al. Tunable hydrogel composite with two-step processing in combination with innovative hardware upgrade for cell-based three-dimensional bioprinting. Acta Biomater 2014;10:630-40. [Crossref] [PubMed]
- Xu T, Jin J, Gregory C, et al. Inkjet printing of viable mammalian cells. Biomaterials 2005;26:93-9. [Crossref] [PubMed]
- Guillotin B, Souquet A, Catros S, et al. Laser assisted bioprinting of engineered tissue with high cell density and microscale organization. Biomaterials 2010;31:7250-6. [Crossref] [PubMed]
- Ambesi-Impiombato FS, Parks LA, Coon HG. Culture of hormone-dependent functional epithelial cells from rat thyroids. Proc Natl Acad Sci U S A 1980;77:3455-9. [Crossref] [PubMed]
- Mandrycky C, Wang Z, Kim K, et al. 3D bioprinting for engineering complex tissues. Biotechnol Adv 2016;34:422-34. [Crossref] [PubMed]
- Wang Y, Zhang Z, Chi Y, et al. Long-term cultured mesenchymal stem cells frequently develop genomic mutations but do not undergo malignant transformation. Cell Death Dis 2013;4:e950 [Crossref] [PubMed]
- Billiet T, Vandenhaute M, Schelfhout J, et al. A review of trends and limitations in hydrogel-rapid prototyping for tissue engineering. Biomaterials 2012;33:6020-41. [Crossref] [PubMed]
- Tasoglu S, Demirci U. Bioprinting for stem cell research. Trends Biotechnol 2013;31:10-9. [Crossref] [PubMed]
- Wu PK, Ringeisen BR. Development of human umbilical vein endothelial cell (HUVEC) and human umbilical vein smooth muscle cell (HUVSMC) branch/stem structures on hydrogel layers via biological laser printing (BioLP). Biofabrication 2010;2:014111 [Crossref] [PubMed]
- Knoepfler PS. From bench to FDA to bedside: US regulatory trends for new stem cell therapies. Adv Drug Deliv Rev 2015;82-83:192-6. [Crossref] [PubMed]
- Wei CC, Lin AB, Hung SC. Mesenchymal stem cells in regenerative medicine for musculoskeletal diseases: bench, bedside, and industry. Cell Transplant 2014;23:505-12. [Crossref] [PubMed]
Cite this article as: Lim W, Kim B, Moon YL. Three-dimensional bioprinting for bone and cartilage transplantation. Ann Joint 2019;4:7.


