
Role of osteotomy in multiligament knee injuries
Introduction
Multiligament knee injury (MLKI) is a complex orthopedic problem that requires knowledge of lower limb biomechanics to establish an appropriate management plan and optimal patient outcome. Discussion of the acute assessment and management of MLKI is beyond the scope of this paper. As such we aim to discuss MLKI in the context of how lower limb alignment influences decision making when dealing with these complex problems. We will provide an overview of the biomechanics of gait and alignment, clinical assessment, clinical decision making and will touch briefly on the types of osteotomy when addressing different ligament patholaxities.
Biomechanical considerations of alignment in MLKI
Gait
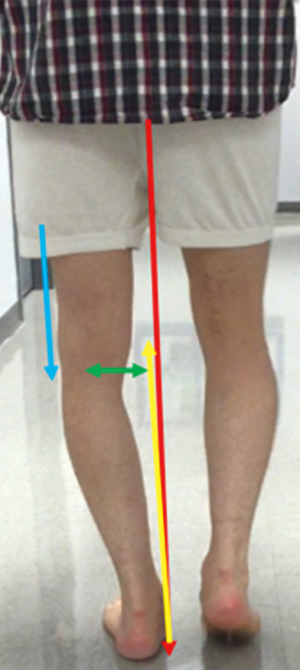
The peak force going through the knee joint is three times the body weight during mobilization (1). Amis proposed a model analyzing the forces going through the knee, to explain the increased medial compartment pressure and lateral tensile forces during gait (2). He proposed that during the stance phase the supporting foot is placed nearer to the line of action of the body weight as shown in Figure 1. This places the hip and tibia in an adducted position in the coronal plane. The equal force vector that arises from the ground reaction force (GRF) passes medial to the knee joint, creating an adduction moment, with a resultant compressive force through the medial compartment (3). There is evidence to show that the rate of loss of articular cartilage, and the progression to osteoarthritis correlates directly with the peak knee adduction moment during gait (4). Loss of medial articular cartilage further accentuates varus creating a larger adduction moment and resulting in a vicious cycle of increasing medial compartment loading and worsening articular cartilage wear (5).
Coronal plane alignment
The lateral structures around the knee counteract the adduction moment. Increasing varus alignment results in increased strain placed on the posterolateral corner (PLC), hence deficiency often results in a varus thrust gait (6). With co-existing cruciate deficiency resulting in hyperextension thrust, the concept described by Noyes of double or triple varus may be encountered (7). That is where the varus alignment is accentuated by the lateral soft tissue deficiency, and further still by the hyperextension recurvatum deformity respectively. In these instances, if a soft tissue reconstruction is performed on the lateral side without considering correction of the coronal plane alignment, there will be significant additional tensile load placed on the reconstructed ligaments, which could compromise the success of the reconstruction. A similar phenomenon may be seen in the valgus knee with medial soft tissue deficiency, although this is often not as common due to the medially placed center of mass and resultant adduction moment. The valgus deformity has to be significant before the medial soft tissues are compromised.
Varus alignment has also been shown to increase the load on the anterior cruciate ligament (ACL) (8). LaPrade showed in a cadaveric study that the forces on the ACL graft significantly increase after sequential sectioning of the lateral collateral ligament (LCL), popliteofibular ligament (PFL) and popliteus tendon (PT). Forces were noted to be significantly higher after LCL transection during varus loading (6). This was further demonstrated in a study of 32 patients with an ACL deficient knee and varus malalignment who underwent gait analysis. An increased load on the lateral soft tissue structures was demonstrated, with separation of the lateral tibiofemoral joint, “condylar lift-off” during the stance phase and an increased medial joint compartment pressure (9). Noyes et al. also investigated the cause of failed posterior cruciate ligament (PCL) reconstruction in a series of 52 patients, finding the leading cause of failure to be posterolateral ligament deficiency (40% of the patients). Importantly, 50% of the failed posterolateral surgical procedures had an underlying varus malalignment (10). In summary, untreated PLC injuries contribute to cruciate ligament graft reconstruction failure by allowing significantly higher forces to stress the graft with varus loading at varying degrees of flexion.
Sagittal plane alignment
In the sagittal plane, changes in the tibial slope have been shown to alter the stresses on the cruciate ligaments. Increasing the posterior tibial slope has been shown to result in an increased shear on the ACL in the stance phase. Giffin et al. showed that an increase of 4 degrees of posterior slope results in an increase in 3 mm of anterior translation and increased strain on the ACL (11). Similarly, a reduced tibial slope may be protective of the ACL, with a negative tibial slope placing greater strain on the PCL due to posterior translation of the tibia and/or hyperextension. Multiple studies have implicated increased tibial slope as a risk factor for ACL injury and failure of ACL reconstruction. Li et al. reviewed 40 consecutive patients who underwent ACL reconstruction with a mean follow up of 27.5 months and showed significant correlation between posterior tibial slope and postoperative anterior knee static stability, where patients with a steeper medial or lateral posterior tibial sloped showed a higher risk for anterior tibial translation of ≥5 mm at thresholds of 5.6° and 3.8°, respectively (12). In a larger series of patients, Webb observed a higher rate of ACL reconstruction failure in patients with a posterior tibial slope greater than 12 degrees (13).
Biomechanics of realignment osteotomy
The role of realignment osteotomy is to correct the mechanical axis, which helps in neutralizing the load going through the knee joint and at the same time reduce excessive stresses on the soft tissue envelope of the knee (14). The most commonly performed osteotomy is the medial opening wedge high tibial osteotomy (MOWHTO), which is an accepted procedure for the management of medial compartment osteoarthritis by reducing the knee adduction moment, a surrogate biomechanical measure of medial compartment load. Equally, as previously indicated, reducing the knee adduction moment will also reduce the tensile load on the lateral soft tissue envelope, thereby rebalancing the knee in the coronal plane. In a similar manner, varus osteotomy, either via the distal femur or proximal tibia, will reduce the knee abduction moment reducing compressive load in the lateral compartment and tensile load in the medial soft tissues.
A uniplanar sagittal correction can also be performed by either an anterior opening (increasing slope) or closing (decreasing slope) wedge osteotomy. This will either decrease the strain on the PCL or ACL, respectively (15). Bi-planar osteotomy is a concept that aims to correct both the coronal and sagittal planes to achieve a neutral mechanical axis. This can have an extremely powerful effect when dealing with complex combined patholaxities such as PCL deficiency combined with PLC injury, where a valgus producing coronal plane correction combined with an increase of the posterior tibial slope may help achieve mechanical balance, without the need for additional soft tissue procedures in some patients.
Clinical assessment
History
A standard history focusing on the patients’ main complaint is elicited, which in the context of the MLKI will be instability and/or pain. A history of pain or other mechanical symptoms may be a symptom of associated injury such as meniscal or chondral pathology which should be taken into consideration if planning an alignment correction. Pre-existing developmental problems, previous knee pathology or surgeries are enquired about. Factors affecting healing are always considered, e.g., smoking, alcohol and relevant medical problems like diabetes mellitus, as these have been associated with an increased rate of complications following osteotomy (16).
Examination
Examination starts with assessment of alignment and gait abnormalities in both the coronal and sagittal planes. Varus, valgus or a hyperextension thrust can sometimes be subtle and close attention must be given. Walking aids and braces may be a clue to instability. Any deformities encountered are examined for their ability to be corrected. Muscle power and wasting is important, as this can affect the outcome. A history of MLKI warrants a thorough assessment of collateral and cruciate ligaments including posterolateral, posteromedial, anterolateral and anteromedial corners. The presence of passive hyperextension will provide a clue to posteromedial or PLC laxity and may also be related to tibial slope. A complete neurovascular assessment is of paramount importance, including distal pulses, perfusion and common peroneal nerve function.
Radiological assessment
Radiological assessment in our institution includes bilateral weight bearing anteroposterior (AP) views of the knee in full extension, a bilateral weight bearing posteroanterior view in 45 degrees of flexion (Rosenberg view), a lateral, and skyline views. Bilateral mechanical axis alignment views [hip-knee-ankle (HKA)] are included following clinical assessment suggestive of malalignment in the coronal and/or sagittal planes. In the acute scenario, if significant coronal plane malalignment is suspected, a monopedal stance HKA view may be used of the contralateral limb to determine the extent of deformity present.
Stress radiographs provide an objective measure of the extent of injury in the coronal and sagittal planes. It is a useful adjunct for preoperative diagnosis and postoperative assessment of a successful radiological outcome. The contralateral side can be used as a control for comparison. These series include varus/valgus stress radiographs and kneeling PCL stress radiographs (17).
An MRI is performed routinely to assess the extent of injury as well as to rule out concomitant meniscal and chondral pathology (18,19), which could follow the initial injury or be a sequel of instability and/or the abnormal biomechanics across the knee joint. A CT scan may be utilized in the presence of fracture deformity or rotational abnormalities that necessitate a rotational profile.
Mechanical axis assessment
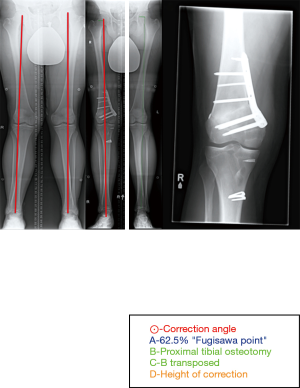
This is important for understanding the distribution of load going through the lower limb during weight bearing. In our institute, we obtain an HKA radiograph as shown in Figure 2. Mechanical axis is defined by dropping a line from the center of the femoral head (FH) and to the mid-point of the tibiotalar (TT) joint surface. In the coronal plane, we define neutral axis alignment as a line passing from FH to TT and between the 2 tibial spines. Medial and lateral axis deviation is defined when that line passes medial or lateral to the tibial spines respectively (20,21). We quantify the extent of deviation by measuring the distance from the medial end of the tibial plateau and dividing it by the distance across the tibial surface. The assumption when doing this assessment is that the knee is in full extension and in neutral rotation. Neutral rotation when taking radiographs is controversial. Oswald calculated on cadavers a modification of 0.2 degrees for every 5 degrees of internal or external rotation of the lower limb (22).
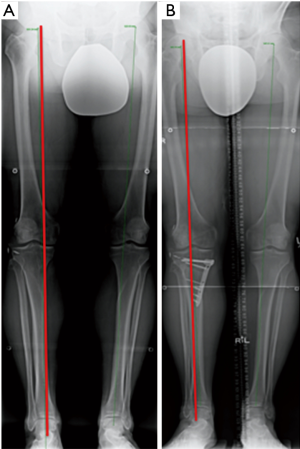
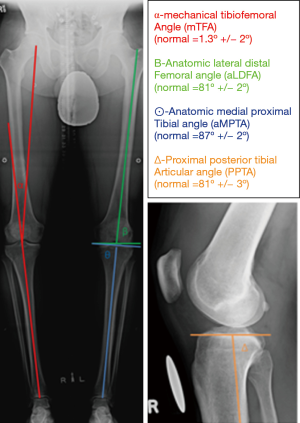
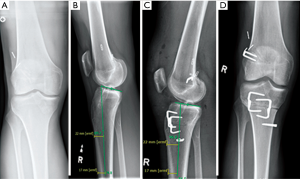
It is important to determine if there is a symmetrical or asymmetrical deformity present, and whether it is intra-articular or peri-articular. Asymmetrical malalignment is suggestive of acquired pathology. In the context of MLKI, it may be secondary to a deficiency in the soft tissue envelope of the knee and should be considered when calculating a corrective osteotomy. A periarticular deformity can be from the femoral or the tibial side. Medial and lateral distal femur and proximal tibial angles are used for assessment as shown in Figure 3. Intra-articular deformity can be assessed by drawing a line across the distal femur and proximal tibial surfaces. These lines are normally parallel and are altered with joint wear and/or ligament laxity.
Mechanical axis deviation in the context of MLKI
In the chronic MLKI it is vital that the mechanical axis is assessed prior to developing a treatment plan. In the case of a symmetric varus or valgus limb alignment, in which there is a lateral or medial sided soft tissue injury +/− cruciate deficiency, the mechanical axis should be corrected to a neutral position so as to reduce the tensile forces on the affected side, or the planned soft tissue reconstruction. Asymmetric alignment may be a result of soft tissue deficiency secondary to either coronal plane laxity or hyperextension as previously described. If the alignment is within 3 degrees of neutral on the unaffected side, it may be appropriate to perform a soft tissue reconstruction only. If it is greater than 3 degrees then an osteotomy should be performed, taking into account the soft tissue laxity that is accentuating the deformity (2).
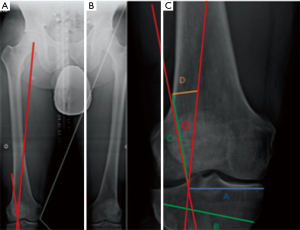
In the acute MLKI, it is generally accepted that soft tissue reconstruction alone will be performed. However, if the coronal plane alignment is significantly abnormal such that the mechanical axis is medial to the medial tibial plateau in the PLC injured knee, as assessed on the contralateral monopedal stance view, it is the authors’ preference to perform a concomitant valgus osteotomy. Similarly, in the valgus knee associated with a medial collateral ligament (MCL) injury, if the mechanical axis resides lateral to the lateral tibial spine, it is our preference to perform a varus osteotomy (Figure 4).
Simultaneously, sagittal plane assessment is key to determine causes for hyperextension recurvatum. A reduced tibial slope can increase hyperextension, accentuated by the loss of the PCL/PLC. This may be an indication for a biplanar correction as previously discussed. However, in combined ACL and PCL injured knees, slope maintenance is important so as not to negatively affect one ligament by inadvertent slope change.
Ideal mechanical axis alignment
In MLKI it is our preference to restore the mechanical axis to a point passing between the medial and lateral tibial spines. However, before proceeding with a corrective osteotomy the tibiofemoral compartment is inspected arthroscopically to assess the degree of meniscal and/or chondral damage that exists. The degree of correction may therefore be tailored to offload the affected compartment if indicated, ensuring that the coronal plane is not over-corrected past the down slope of the appropriate tibial spine.
Technical considerations for realignment osteotomy
The aim of an osteotomy following MLKI is to correct the mechanical axis, neutralizing the forces that would otherwise cause undue stress on reconstructed ligaments. Correction of mechanical axis alone, may on occasions may be sufficient in restoring functional stability, even in the absence of ligament reconstruction. A prospective study of 21 patients with initial varus and chronic PLC deficiency showed that 38% of the patients had sufficient functional improvement following HTO and didn’t require subsequent PLC reconstruction (20). An osteotomy also offers the benefit of reducing excessive loads that would accelerate cartilage wear, as would be the case in a varus corrective osteotomy reducing load on the medial compartment.
When planning for a corrective osteotomy in MLKI, there are several factors that have to be considered before implementing a successful correction:
- Patient’s symptoms;
- Examination findings;
- Correlation of imaging with symptoms and examination;
- Determination of location of deformity;
- Degree of deformity;
- Method to correct deformity;
- By how much to correct deformity?
Points I–V have been dealt with previously. The decision on which method to correct the deformity is based on all of these factors.
Realignment osteotomy can address varus/valgus in the coronal plane or commonly recurvatum deformity in the sagittal plane. Deformities involving the coronal plane can be addressed on the tibial or femoral side with an opening or closing wedge osteotomy, whereas sagittal plane deformity is most commonly addressed on the tibial side due to its relationship with tibial slope.
Valgus producing osteotomy
A valgus osteotomy is most commonly performed on the tibial side, reducing stress on the lateral soft tissue envelope. This would be utilized in the PLC deficient knee. Medial opening or lateral closing wedge osteotomies both have their pros and cons. Our preference is an MOWHTO, as it allows easier correction of both coronal and sagittal planes, and unlike the closing wedge technique, it preserves bone stock and allows easier titration of correction (Figure 3). A disadvantage may be the potential of loss of correction; however, with latest generation of fixation systems currently in use, this is seen less often (23-25).
Figure 5 illustrates how we plan the extent of deformity correction using the technique by Dugdale et al. (26).We aim for a neutral limb mechanical axis, making sure the lateral soft tissue laxity is taken into account in the correction. A general rule of thumb is that for every 1mm increase of asymmetric gapping of the lateral compartment should result in a 1mm reduction in wedge opening.
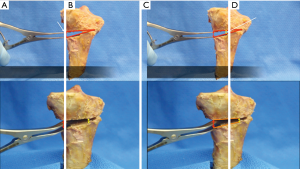
A recent meta-analysis showed the posterior tibial slope to have increased by 2.02° (P=0.005) after MOWHTO. This is most often secondary to a lack of understanding of the three-dimensional geometry of the proximal tibia. Given its triangular shape, it is imperative that close attention is paid to the geometry of the osteotomy ‘‘gap’’ to avoid inadvertently increasing the posterior tibial slope (Figure 6). To maintain slope, it is vitally important to ensure that the posteromedial gap is approximately twice as large as the anterior gap, at the level of the tibial tubercle, thereby producing a trapezoidal wedge. On the other hand, it is not uncommon that patients with chronic MLKI require a biplanar osteotomy, addressing both the tibial slope and the coronal alignment. In the instance of a combined PCL/PLC injury, a rectangular wedge opening is attained, thereby increasing the tibial slope to a greater extent than the coronal correction.

In the scenario where a reduction of slope is required, for example in the combined chronic ACL/PLC knee, a lateral closing wedge HTO (LCWHTO) can be utilized to great effect, as the aforementioned study also found that the tibial slope was decreased by 2.35° (P<0.001) after this procedure. In another study, Ranawat et al. demonstrated that MOWHTO cannot be reliably used to significantly reduce tibial slope, and a closing wedge procedure is preferred (27). However, depending upon the size of correction, a concomitant fibular osteotomy or release of the proximal tibiofibular joint is always required, with the associated risk of common peroneal nerve injury. Therefore, caution is required.
Varus producing osteotomy
Varus corrections for medial soft tissue laxity are much less common; however, they may be utilized to reduce the tensile load on the MCL as well as reduce the compressive load on the lateral compartment. A distal femoral osteotomy (DFO) is most commonly used due to the valgus deformity most often being present within the distal femur secondary to a hypoplastic lateral femoral condyle resulting in a reduced lateral distal femoral articular angle (LDFA). Our preference is to use a medial closing wedge distal femoral varus osteotomy (MCWDFVO) as it is inherently stable thereby patients can weight bear early, provides excellent bone to bone healing and results in less hardware irritation than the lateral opening wedge option (Figure 4). However, there is the risk of superficial femoral artery injury due to the proximity of the adductor canal, as well as it is not as easy to titrate the desired correction as the opening wedge option.
In cases where a varus correction and slope change is required we prefer a medial closing wedge HTO. The benefit of this procedure is that it corrects the mechanical load throughout the range of flexion, not just primarily in extension as per the DFVO (28). The MCL must also be re-tensioned following wedge removal. Care must be taken to not create an oblique joint line as this may have detrimental effects on cartilage and ligamentous strain.
Uniplanar sagittal plane corrections
A uniplanar tibial slope correction may be performed as an anterior opening wedge (Figure 7) to increase slope or as an anterior closing wedge (Figure 8) to reduce slope to address PCL and ACL deficiency respectively. The former can be useful in the chronic PCL deficient knee with co-existing hyper-extension recurvatum. A 1-degree change in slope has been shown to account for every 1 mm of anterior closure with resulting reduction in ACL strain (15). From a technical point of view, the surgery may be performed with or without a tibial tubercle osteotomy. Removing the tibial tubercle allows for excellent visualization of the proximal tibia and also provides a further method of fixation of the wedge, as a screw can be placed either side of the wedge in both the metaphysis and diaphysis providing tubercle fixation. A TTO is also useful so as to avoid patella baja, in the event of performing an anterior opening wedge proximal to the tubercle insertion.
Clinical outcome following realignment osteotomy for MLKI
There are few studies in the literature that review the functional outcomes of knee ligament instability following a realignment ostomy. A recent systematic review found only four studies discussing functional outcome following HTO in PLC-deficient and combined PLC-deficient knees. All studies confirmed the beneficial role of HTO. Arthur et al. reported on 21 patients with combined chronic PLC deficiency and genu varum (20). In their study, 38% of the patients did not require further ligament reconstruction, as they achieved stability. Naudie et al. reviewed the results of 17 opening wedge HTOs in 16 patients with a symptomatic hyperextension-varus thrust and showed that opening wedge HTO can produce good functional and radiographic results, at a mean of 56 months (29). Noyes et al. treated 41 young patients with ACL deficiency, varus deformity and posterolateral ligament instability, all with HTO (7). A 100% follow-up at a mean of 4.5 years showed a reduction of pain in 71%; elimination of giving way in 85%; and resumption of light recreational activities in 66% (27 knees). Mean Cincinnati Knee Rating Score significantly improved from 63 to 82 points. The author recommended osteotomy in addition to ligament reconstructive procedures in these knees with complex injury patterns. Finally, Badhe et al. treated 14 patients with knee instability and varus alignment with HTO with or without ligament reconstruction (30). Five patients were treated with HTO and ACL reconstruction (double varus). Six patients with varus and posterior/PLC instability were treated with ligament recon and HTO (triple varus) and 3 were treated with HTO only. At a mean follow-up of 2.8 years, 12 knees were stable while the remaining 2 were unstable. Thirteen (93%) of the patients were able to participate in light recreational activities. Mean Cincinnati Knee Score improved from a mean of 53 preoperatively to a mean of 74 postoperatively. The author recommended HTO along with ligament reconstruction in this complex group of patients.
Conclusions
Patients with chronic multiligament injuries represent a complex group of patients. Knee ligament injuries can be heterogenous and a thorough clinical and radiological assessment is required. Patients may have instability secondary to their ligament insufficiency accentuated by malalignment of the mechanical axis in the coronal and/or sagittal planes. Osteotomy plays an important role in the correction of the mechanical axis in knee ligament instability, with reported good outcomes and return to function. It helps redistribute the load through the knee joint and protects the reconstructed ligaments against excessive stress that can result in failure. Biplanar osteotomy is an important concept, as correction of the mechanical axis is achieved in the coronal and sagittal planes; however, it is very important to understand the proximal tibial geometry so as to adequately affect the tibial slope in the desired manner.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Camilo Partezani Helito and Jorge Chahla) for the series “The Multiligament Injured Knee” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: The series “The Multiligament Injured Knee” was commissioned by the editorial office without any funding or sponsorship. AG is a paid consultant for Smith and Nephew Inc. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech 2001;34:859-71. [Crossref] [PubMed]
- Bellemans J, Colyn W, Vandenneucker H, et al. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 2012;470:45-53. [Crossref] [PubMed]
- Shelburne KB, Torry MR, Pandy MG. Muscle, ligament, and joint-contact forces at the knee during walking. Med Sci Sports Exerc 2005;37:1948-56. [Crossref] [PubMed]
- Teichtahl AJ, Davies-Tuck ML, Wluka AE, et al. Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthr Cartil 2009;17:8-11. [Crossref] [PubMed]
- Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:197-205. [Crossref] [PubMed]
- LaPrade RF, Resig S, Wentorf F, et al. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med 1999;27:469-75. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD, Hewett TE. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 2000;28:282-96. [Crossref] [PubMed]
- van de Pol GJ, Arnold MP, Verdonschot N, et al. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med 2009;37:481-7. [Crossref] [PubMed]
- Noyes FR, Schipplein OD, Andriacchi TP, et al. The anterior cruciate ligament-deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med 1992;20:707-16. [Crossref] [PubMed]
- Noyes FR, Barber-Westin SD. Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med 2005;33:646-54. [Crossref] [PubMed]
- Giffin JR, Stabile KJ, Zantop T, et al. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 2007;35:1443-9. [Crossref] [PubMed]
- Li Y, Hong L, Feng H, et al. Posterior tibial slope influences static anterior tibial translation in anterior cruciate ligament reconstruction: a minimum 2-year follow-up study. Am J Sports Med 2014;42:927-33. [Crossref] [PubMed]
- Webb JM, Salmon LJ, Leclerc E, et al. Posterior Tibial Slope and Further Anterior Cruciate Ligament Injuries in the Anterior Cruciate Ligament-Reconstructed Patient. Am J Sports Med 2013;41:2800-4. [Crossref] [PubMed]
- Wada M, Imura S, Nagatani K, et al. Relationship between gait and clinical results after high tibial osteotomy. Clin Orthop Relat Res 1998;180-8. [Crossref] [PubMed]
- Giffin JR, Vogrin TM, Zantop T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 2004;32:376-82. [Crossref] [PubMed]
- Martin R, Birmingham TB, Willits K, et al. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 2014;42:1118-26. [Crossref] [PubMed]
- James EW, Williams BT, LaPrade RF. Stress radiography for the diagnosis of knee ligament injuries: A systematic review. Clin Orthop Relat Res 2014;472:2644-57. [Crossref] [PubMed]
- Richter M, Bosch U, Wippermann B, et al. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocations. Am J Sports Med 2002;30:718-27. [Crossref] [PubMed]
- Becker EH, Watson JD, Dreese JC. Investigation of multiligamentous knee injury patterns with associated injuries presenting at a level I trauma center. J Orthop Trauma 2013;27:226-31. [Crossref] [PubMed]
- Arthur A, LaPrade RF, Agel J. Proximal tibial opening wedge osteotomy as the initial treatment for chronic posterolateral corner deficiency in the varus knee: a prospective clinical study. Am J Sports Med 2007;35:1844-50. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Agel J, et al. Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am 2010;92:16-22. [Crossref] [PubMed]
- Oswald MH, Jakob RP, Schneider E, et al. Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty 1993;8:419-26. [Crossref] [PubMed]
- Yasuda K, Majima T, Tsuchida T, et al. A ten- to 15-year follow-up observation of high tibial osteotomy in medial compartment osteoarthrosis. Clin Orthop Relat Res 1992;186-95. [PubMed]
- Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am 1993;75:196-201. [Crossref] [PubMed]
- Brinkman JM, Lobenhoffer P, Agneskirchner JD, et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 2008;90:1548-57. [Crossref] [PubMed]
- Dugdale TW, Noyes FR, Styer D. Preoperative Planning for High Tibial Osteotomy: The Effect of Lateral Tibiofemoral Separation and Tibiofemoral Length. Clin Orthop Relat Res 1992;248-64. [PubMed]
- Ranawat AS, Nwachukwu BU, Pearle AD, et al. Comparison of Lateral Closing-Wedge Versus Medial Opening-Wedge High Tibial Osteotomy on Knee Joint Alignment and Kinematics in the ACL-Deficient Knee. Am J Sports Med 2016;44:3103-10. [Crossref] [PubMed]
- Collins B, Getgood A, Alomar AZ, et al. A case series of lateral opening wedge high tibial osteotomy for valgus malalignment. Knee Surg Sports Traumatol Arthrosc 2013;21:152-60. [Crossref] [PubMed]
- Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med 2004;32:60-70. [Crossref] [PubMed]
- Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc 2002;10:38-43. [Crossref] [PubMed]
Cite this article as: Abdelrahman T, Getgood A. Role of osteotomy in multiligament knee injuries. Ann Joint 2019;4:8.


