
Social 3D printing in Chile—experience and vision
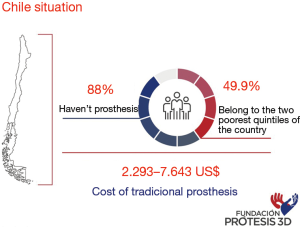
3D technology takes a long time, having a broad international progress, since 2005 when, through the RepRap Project (1), the first 3D printer is developed that can be manufactured in bulk and at low cost, since then applied in different Inclusion areas. In the field of medicine, in Chile its arrival dates to approximately 2012, however, its incorporation in the field of Social Health has been slow and complex due to the costs that this usually implies. In Chile, according to studies conducted by the National Disability Service (SENADIS) (Figure 1), about 88% cannot access them due to their health insurance. The classic prostheses (hook), have a cost that fluctuates between the 2,293 to 7,643 dollars in our country, and considering that 49.9% of the people in a situation of disability belong to the two poorest quintiles of the country, according to the II Estudio Nacional de la Discapacidad (II National Study of Disability) (2), makes these prostheses almost unattainable for a high segment of this population. The institutions that support this type of aid are the Teletón, for children and young people, and the Mutual Administrators of the law 16744 for work accidents and occupational diseases, being until not long ago, the prosthesis generated by 3D printing, outside of the benefits delivered or accessible to the vast majority of people.
Due to this reality, and the hand of a group of selfless engineers, was born the initiative to which I belong, “Fundación Prótesis 3D” (“3D Prosthetics Foundation”), which initially develops 3D printing prostheses for people with amputations or malformations of the upper limb (Figure 2), with a social and non-profit perspective, being the first foundation of these characteristics in Chile. This initiative is based initially on the work done by Zuniga (3), compatriot creator of the prosthesis model Cyborg Beast; and The “Enable The Future” Community, who through a modeling software at low cost, generated a 3D printing hand whose models are on the internet for free by placing my country on the map of this technology, making the use of such a useful tool grow. However, recently it has been incorporated with force into a policy of public support to cover the needs of those who have least and most need.
Why was it so delayed at the local level to penetrate the world of health this technology?
Perhaps, under a very personal view based on experience, as doctors we are often narcissistic and leave aside what we cannot do, do not realize, or directly exceed what we as individuals are capable of. This was experienced by the creators of our foundation, who sought help in the medical world, and institutions. Renowned upper extremity surgeons and other health teams did not believe in the usefulness that this could cause to people, moreover, I think they saw as a failure the need to include another professional that was not directly from the health area in an integral care process. If I as a doctor cannot do it, "should anyone?" This was undoubtedly one of the most complex points to overcome. The second obstacle is that all social initiative, part of the basis of a job without economic compensation, so get those who contributed, at first it was very difficult, but even without fame or external recognition for those who did. However, although I am a man of science, I am also a believer and it is here where I believe it was something of God to have crossed paths with such good people, at a difficult time for them. They had left their work, their time, for a noble cause. It did not cost anything to set aside prejudices and try to be part of a team with such noble intentions, being able to incorporate myself, receive the rejoicing of the joy of those we help, the best payments that in life can be received. My mission within the foundation was to empower the team with the necessary criteria that required the printing of prostheses and direct delivery to the user, to enter the world of Health in an appropriate manner. We include:
- Prior medical control: this is a comprehensive analysis of the future user, analyzing the type of residual stump, the presence of keloids, neuromas, rotational alterations that could be incorporated into the pre-established design, protection improvements, as well as treatment suggestions as an excess of neuromas, psychological or psychiatric treatments to those who have inconclusive processes. Remember that many of our users come from media where they have not managed to receive all this.
- Occupational therapy control: in this stage, the measurements are taken, management of suggested improvements, beginning of the rehabilitation and training for the best prosthetic use. After the prosthesis is delivered.
- Psychological control pre-delivery prosthetic and post rehabilitation: what allows to optimize how users incorporate this contribution to their life and what effect it has on them, in addition to providing accessory tools to face life.
- Continuous monitoring, serial of our users, for analysis of difficulties, skin complications, prosthesis change among others
- Research: the data collection and analysis of these allows to validate the impact of this initiative in the middle.
All the above, associated with the intense and fundamental engineering work that was born from the creation of this initiative, developing the obtaining of resources, dissemination of information, recruitment of users, strategic alliances, image positioning, resource management, preparation of prostheses, etc. It allowed, finally in metaphor, deliver a luxury car and teach how to handle it, reducing the risks of accidents, taking full advantage of the help that was being offered. It has not been an easy road, but the effort mainly of my friends and partners in this initiative, is what has led to position the foundation both nationally and internationally, as a recognized initiative in the young world of social assistance. Currently we have completed the delivery of more than 45 prostheses with patients from 3 to 65 years old. Today we moving forward with the completion of studies that demonstrate the functional and psycho-social utility of the incorporation of this technology in children and adults, as well as the completion of a prototype of myoelectric prostheses for people with transradial amputations (Figure 3), based on the Open Source model “Exii HackBerry”, which captures the muscular impulses of the biceps through an infrared sensor, which interprets the level of the impulse as the level of press that the prosthesis must make, besides changing the position of the thumb that provides a variation to the type of press made and possess a tool that allows the index finger of the prosthesis to perform an independent movement when fixing the position of the other fingers.
From this point there is still a lot to do, continue working, improving day by day and optimizing processes, helping and taking the expertise of each area forward this social initiative, which is highly replicable anywhere in the world, calling on you colleagues to contribute his knowledge in the development of a better world.
Acknowledgments
We would like to thank the TresDP Company for the sponsorship and technical support in 3D prosthesis printing. Also, to the National University Andrés Bello for the provision of an operations laboratory in its facilities and to the volunteers of Fundación Prótesis 3D that allow the successful development of this initiative.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Young Lae Moon) for the series “Medical 3D Application in Orthopaedics” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.01.05). The series “Medical 3D Application in Orthopaedics” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All parents, children and beneficiaries of the foundation were informed about the use of images and videos for future studies, signing the beneficiaries or their parents in case of being a minor.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ortiz K, Aveiga H, Medina J, et al. Los beneficios de las impresoras 3D como herramienta de innovación en la medicina”, Revista Caribeña de Ciencias Sociales (2016). Available online: http://www.eumed.net/rev/caribe/2016/06/3d.html
- Ministerio de Desarrollo Social Chile (2015). II Estudio Nacional de la Discapacidad. Available online: http://observatorio.ministeriodesarrollosocial.gob.cl/endisc/docs/Libro_Resultados_II_Estudio_Nacional_ de_la_Discapacidad.pdf
- Zuniga J, Katsavelis D, Peck J, et al. Cyborg beast: a low-cost 3d-printed prosthetic hand for children with upper-limb differences. BMC Res Notes 2015;8:10. [Crossref] [PubMed]
- González Jofré C, Toro Sepúlveda O, Retamales Gómez D, et al. Beneficiaries of 3D prosthesis. Asvide 2019;6:042. Available online: http://www.asvide.com/article/view/29980
Cite this article as: González Jofré C, Toro Sepúlveda O, Retamales Gómez D, Retamales Gómez L. Social 3D printing in Chile—experience and vision. Ann Joint 2019;4:14.



