
Turf toe: review of the literature and surgical technique
IntroductionOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Turf toe is an injury to the hallux metatarsal-phalangeal joint complex. Most commonly it is due to a hyper-dorsiflexion moment of the proximal phalanx on the metatarsal head that leads to tension failure of the plantar capso-ligamentous structures. This commonly may include injury to the plantar plate, flexor halluces brevis tendons, and the sesamoids. The term turf toe, was initially coined by Bowers in 1976 when reporting 27 such injuries after the installation of first-generation artificial turf at the University of West Virginia. At that time, the authors concluded that the injury was imparted by the combination of a stiff playing surface and relatively flexible footwear (1). Soon thereafter, Coker and colleagues reported on the same injury in those at the University of Arkansas after the implementation of similar artificial turf. The authors reported an average of 6 turf-toe injuries per season, which led to more missed game-time than ankle sprains, although ankle injuries were more than eight times more common (2). Clanton’s series, evaluating Rice University players from 1971 to 1985, estimated 4.5 cases of turf toe per season with the average player missing approximately 1 week. The authors also concluded the condition may be attributed to an overly flexible shoe on a stiff playing surface (3). Rodeo was the first to report on the injury seen in American professional football. His survey of 8- active football players found that 45% had suffered what they believed to be a turf-toe injury. Eighty-three percent of players believed the injury occurred on artificial turf (4). These early studies helped to define turf-toe injury mechanisms as well as generate discussions about the risk factors of flexible footwear with unforgiving playing surfaces. More recent studies show the incidence of turf toe injuries in high-level college and professional football players to be lower than previously reported. At the 2006 National Football League combine, 11% of athletes reported a turf toe injures with running backs, tight-ends, and linebackers being the most commonly affected positions (5). A review over 5 seasons from 2004 to 2009 in American college football players revealed turf-toe was 83% of all reported injuries with approximately 5 turf-toe injuries per team per year. They did find significantly higher rates of injury in Division I vs. Division III, actual games versus practice (13X), and artificial turf versus natural grass with 85% of injuries occurring on artificial turf (6). Pearce described the epidemiology of foot injuries in rugby players in the UK over 4 seasons. They noted 16 cases of turf toe, accounting for 11% of the total foot injuries seen in rugby (7).
AnatomyOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
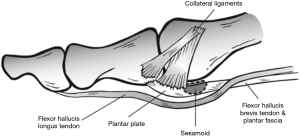
The anatomy of the first metatarsophalangeal (MTP) consists of a complex relationship between the bony, capsular, and musculotendinous elements. The first MTP joint withstands nearly 50% of the body weight during normal gait, up to 2–3 times body weight during athletic activity, and up to 8 times body weight with sprinting and jumping (8,9). The first metatarsal head and proximal phalanx join in a condyloid joint arrangement that can be classified as flat, rounded or chevron shaped and has little intrinsic stability. The medial and lateral sesamoids lie plantar to the first metatarsal head within the tendon of the flexor hallucis brevis (FHB) tendon. Ten percent of the population will have a bipartite sesamoid, with 25% of these being bilateral, and the medial sesamoid being more commonly bipartite. The medial sesamoid is larger, more distal, and bears more weight. The sesamoids function to increase plantar flexion power of the first ray by increasing the moment arm of the intrinsic flexors plantar to the metatarsal head, as well as dissipate forces across the metatarsal head (10). The sesamoids are stabilized by a network of capsoligamentous structures including the metatarsal-sesamoid, phalangeal-sesamoid, and inter-sesamoid ligaments. The plantar plate is a robust soft tissue complex the originates as a thin continuation of the periosteum of the plantar first metatarsal distal metaphysis and inserts as a firm fibrocartilaginous attachment on the proximal phalanx. Attachments to the plantar plate include the collateral ligaments, transverse metatarsal ligament, plantar fascia, abductor and adductor hallucis, and flexor hallucis brevis tendon. Johnston found the plantar plate to be approximately 2 cm long, 1 cm wide, and 2–5 mm thick (11) (Figure 1).
Mechanism of injuryOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
The most common mechanism of injury involves the foot plantarflexed and fixed to the ground with the ankle in equinus. When an axial load is applied to the ankle, commonly by another player falling onto the ankle, the MTP is driven into hyper-extension and the plantar joint capsuloligamentous structures are put under tension. This can also be combined with an element of valgus or varus that may injure other collateral stabilizing structures.
Clinical assessmentOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Patients commonly present with first MTP joint pain, and often will remember a distinct injury. However, given the vague symptoms of forefoot pain with intense activities and the rare nature of the injury, one must keep a high index of suspicion for the diagnosis. Pain, swelling, and bruising near the 1st MTP joint are common in the acute setting. Pain may be exacerbated with weight bearing especially during the heel-rise phase. Other exam signs may include weight bearing on the lateral border of the foot to off-load the injured area, decreased range of motion, and positive Lachman. A patient may also exhibit valgus or varus instability if the injury has affected the medial or lateral stabilizing structures, respectively.
GradingOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Grade I injuries are characterized by stretching of the plantar capsule with minimal symptomatology. Grade II injuries include partial tears that are often accompanied by moderate pain and swelling. Grade III injuries involve a complete tear of the plantar capsule with significant tenderness and swelling. Grade III injuries nearly always have a positive dorsal drawer exam. They may also have associated injuries to the MTP joint structures (12,13).
ImagingOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Initial imaging should include weight bearing AP and lateral radiographs of the affected foot with contralateral films for comparison if needed. With significant injury, proximal retraction of the sesamoids can be seen. Other views include the 40-degree oblique views and the axial sesamoid view which can help to visualize a sesamoid fracture. On the lateral sesamoid stress view, the sesamoids should track distally upon dorsiflexion of the proximal phalanx. Failure of appropriate tracking signifies significant injury to the plantar capsule. Waldrop showed that differences of 3 mm or more between the injured and uninjured feet have a high likelihood of injury to at least 3 of the 4 ligaments (MCL, LCL, tibial and fibular phalangeosesamoid ligaments) of the plantar capsule. Sectioning of three ligaments resulted in an average of 3.2 mm difference between the intact and the injured state. Sectioning of four ligaments resulted in an average of 7.5 mm difference between the injured and intact states. Sectioning of one or two of the four ligaments had no significant difference from the intact state. Based on this data, if there is an apparent difference on the lateral stress radiograph, there is likely a significant turf toe injury (14) (Figures 2,3).
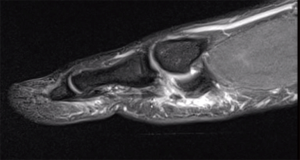
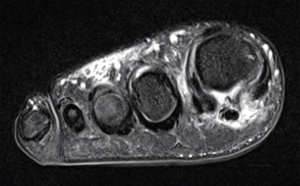
MRI can be very beneficial and is generally indicated for type II and type III injuries. Any injuries with significant swelling and tenderness or instability on physical exam or radiographs may also benefit from more advanced imaging (12,13). MR grading for turf toe is similar to grading for other ligamentous injuries. Grade I injuries will have intact fibers with surrounding edema. Grade II injuries will show partial disruption of fibers and edema. Grade III injuries show frank discontinuity of fibers and surrounding edema. Edema around a sesamoid fracture that may indicate acute fracture versus a bipartite sesamoid. T2 proton density fat saturation sequences are generally considered to be the most helpful for acute turf toe injuries (15).
Nonoperative treatmentOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Non-surgical treatment is generally considered for type I and type II turf toe injuries. Initial treatment begins with standard techniques to reduce inflammation such as rest, ice, and elevation. Depending on the degree of discomfort, a stiff soled shoe, walking boot or toe spica cast may be used to decrease torsional stress across the MTP joint. Taping is not recommended in the immediate setting due to acute swelling to avoid risk of constriction ischemia (12,13). Once swelling has resolved, conservative treatment for grade I and II injuries consists of taping the hallux in slight plantarflexion to allow apposition of any partially torn fibers and to limit any further attenuation. Range of motion can begin with passive plantarflexion during the first week. Experts recommend beginning low-impact activities with the toe protected from passive dorsiflexion, then gradually increasing activities up to full push-off as long as there is no increase in pain. In general, athletes can expect to miss at least 2 weeks for grade I injuries and sometimes up to 3 months for grade II injuries before full return to play can be expected (3,6,12,13). As players return to athletic participation, it is recommended that a carbon fiber plate or Morton’s extension be instituted into the footwear.
Operative treatmentOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
There are several well-established indications for operative treatment of a turf toe injury. These may include large capsular avulsions, diastasis of a bipartite sesamoid, sesamoid fractures, retracted sesamoids, traumatic hallux valgus, vertical instability, loose bodies, chondral injury, and failure of conservative treatment.
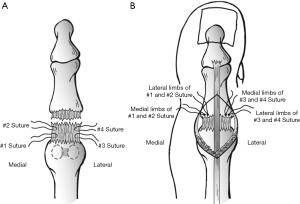
Operative intervention is generally performed through one of two approaches. Commonly an “L” shaped medial longitudinal incision that curves laterally plantar to the first MTP joint will allow for flap retraction and access to the plantar plate. A longitudinal medial incision with an independent second plantar lateral incision may also be considered. If the plantar capsule is repairable, the authors generally primarily repair the tissue with multiple simple sutures passed through the proximal and distal stumps of tissue. These are then tied with the hallux in slight plantar flexion. In the case of attenuated tissue, our preferred technique is to advance the plantar capsule through bone tunnels in the proximal phalanx. A small dorsal lateral incision over the MTP joint is used to aid in suture passage. Given the small working space, suture placement may be aided by suture passage devices. Distal to the sesamoids, four sutures (eight strands) are placed in the proximal tissue stump in a mattress type fashion. Four holes are drilled at the base of the proximal phalanx distal to the articular surface. The suture limbs are then shuttled through the bone tunnels and tied over a bone bridge with the toe in slight plantarflexion (16) (Figure 4). The senior author (JF Doty) routinely places the patient into a splint for the first two weeks, and then transitions the patient into a boot or hard sole shoe and allows heel weight bearing until 6 weeks postoperatively. Passive plantarflexion begins at the 2-week postoperative visit as long as the surgical incision is healed. At 6 weeks, the patient is permitted to wear a well-cushioned athletic shoe with a graphite plate or carbon fiber insert to support the hallux as ambulation is progressed. Return to sport conditioning begins at 3 months, with a goal of returning to full sport at 6 months. Some evidence suggests that athletes should be counseled that it takes up to 12 months to return to elite level athletics (12,13).
OutcomesOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Given the rarity of surgical treatment of these injuries, outcome data is limited to generally small case series (12,13,17). Waldrop reported on 15 high-level athletes that underwent surgical repair for grade III turf toe. At an average of 28 months postoperatively, the VAS pain scores at rest and during activities were less than one. The average return to play was 16.5 weeks, with all athletes participating with a custom insole and one patient required reoperation do to continued pain (18). In 2002, Anderson report on 19 high-level athletes with turf toe with 9 of 19 undergoing operative repair. Seventeen of nineteen returned to full athletic activity with 0 complications (12). Drakos presented 3 cases with 2 being treated surgically over a 4-year period. Each athlete was able to return to play high-level football at approximately 6 months (19). Clanton reported on 20 cases with an average 5-year follow-up and found that nearly half of patients had some degree of persistent pain and stiffness in the hallux (3). In summary, the rehab and return to play for significant turf toe injuries may take 6–12 months, with most athletes eventually capable of returning to high-level athletic activity. Patients should be counseled that long-term stiffness and occasional pain in the toe are not infrequent chronic problems after a significant turf toe injury.
AcknowledgmentsOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Funding: None.
FootnoteOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.05.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Introduction
- Anatomy
- Mechanism of injury
- Clinical assessment
- Grading
- Imaging
- Nonoperative treatment
- Operative treatment
- Outcomes
- Acknowledgments
- Footnote
- References
- Bowers KD Jr, Martin RB. Turf-toe: a shoe-surface related football injury. Med Sci Sports 1976;8:81-3. [PubMed]
- Coker TP, Arnold JA, Weber DL. Traumatic lesions of the metatarsophalangeal joint of the great toe in athletes. Am J Sports Med 1978;6:326-34. [Crossref] [PubMed]
- Clanton TO, Butler JE, Eggert A. Injuries to the metatarsophalangeal joints in athletes. Foot Ankle 1986;7:162-76. [Crossref] [PubMed]
- Rodeo SA, O’Brien S, Warren RF, et al. Turf-toe: an analysis of metatarsophalangeal joint sprains in professional football players. Am J Sports Med 1990;18:280-5. [Crossref] [PubMed]
- Kaplan LD, Jost PW, Honkamp N, et al. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop 2011;40:40-4. [PubMed]
- George E, Harris AH, Dragoo JL, et al. Incidence and risk factors for turf toe in- juries in intercollegiate football: data from the National Collegiate Athletic Association injury surveillance system. Foot Ankle Int 2014;35:108-15. [Crossref] [PubMed]
- Pearce CJ, Brooks J, Kemp SP, et al. The epidemiology of foot injuries in professional rugby union players. Foot Ankle Surg 2011;17:113-8. [Crossref] [PubMed]
- Stokes IA, Hutton WC, Stott JR, et al. Forces under the hallux valgus foot before and after surgery. Clin Orthop Relat Res 1979;64-72. [PubMed]
- Nigg BM. Biomechanical aspects of running. In: Nigg BM, ed. Biomechanics of Running Shoes. Champaign, IL: Human Kinetics, 1986:1-25.
- Richardson EG. Injuries to the hallucal sesamoids in the athlete. Foot Ankle 1987;7:229-44. [Crossref] [PubMed]
- Doty JF, Coughlin MJ. Turf toe repair: a technical note. Foot Ankle Spec 2013;6:452-6. [Crossref] [PubMed]
- McCormick JJ, Anderson RB. Turf toe: anatomy, diagnosis, and treatment. Sports Health 2010;2:487-94. [Crossref] [PubMed]
- McCormick JJ, Anderson RB. The great toe: failed turf toe, chronic turf toe, and complicated sesamoid injuries. Foot Ankle Clin 2009;14:135-50. [Crossref] [PubMed]
- Waldrop NE 3rd, Zirker CA, Wijdicks CA, et al. Radiographic evaluation of plantar plate injury: an in vitro biomechanical study. Foot Ankle Int 2013;34:403-8. [Crossref] [PubMed]
- Crain JM, Phancao JP, Stidham K. MR imaging of turf toe. Magn Reson Imaging Clin N Am 2008;16:93-103. vi. [Crossref] [PubMed]
- Johnston RB 3rd, Smith J, Daniels T. The plantar plate of the lesser toes: anatomical study in human cadavers. Foot Ankle Int 1994;15:276-82. [Crossref] [PubMed]
- Kadakia AR, Molloy A. Current concepts review: traumatic disorders of the first metatarsophalangeal joint and sesamoid complex. Foot Ankle Int 2011;32:834-9. [Crossref] [PubMed]
- Smith K, Waldrop N. Operative Outcomes of Grade 3 Turf Toe Injuries in Competitive Football Players. Foot Ankle Int 2018;39:1076-81. [Crossref] [PubMed]
- Drakos MC, Fiore R, Murphy C, et al. Plantar-plate disruptions: "the severe turf-toe injury." three cases in contact athletes. J Athl Train 2015;50:553-60. [Crossref] [PubMed]
Cite this article as: Fraser TW, Doty JF. Turf toe: review of the literature and surgical technique. Ann Joint 2019;4:28.



