
A technique for anchor plug salvage in the setting of a cold welded taper adapter following compress implant failure
Introduction
The Compress implant (Zimmer Biomet, Warsaw, IN) is designed to generate compliant fixation at the endoprosthesis-bone interface in a limb salvage situation. Use of this device is well described in the literature, and reported implant failure rates have been relatively low compared to some previous implant designs (1-3). Typically, failures are aseptic in nature, and occur at the implant-bone interface relatively early after the index surgery (1,2).
“Cold welding” is a term typically applied in the total hip arthroplasty literature (4,5), and refers to a situation in which a modular interface cannot be disengaged during revision surgery. This has been most commonly reported at titanium-titanium head-neck junctions in hip arthroplasty, and may result in the removal of an otherwise well-functioning femoral stem (4).
The following report describes the case of a young patient treated with a Compress implant in conjunction with a distal femoral replacement that functioned well for seven years, but ultimately failed at a modular junction away from the implant-bone interface. Additionally, we present a technique for salvage of an existing anchor plug in the setting of a cold-welded taper adapter, causing initial inability to access the compression nut to remove the spindle.
Case presentation
The patient was a 22 years old man with a history of osteosarcoma of the left distal femur who was treated with wide resection and endoprosthetic reconstruction using a Compress implant (Zimmer Biomet, Warsaw, IN) seven years previously. He had done very well over the years, and was quite active athletically. The day prior to his presentation, he noted instability of the leg and a discontinuity of the thigh. Radiographs demonstrated mechanical failure of the implant near the junction of the Compress device and the diaphyseal segment (Figure 1). Revision surgery was offered to the patient in order to restore function and provide a stable limb.
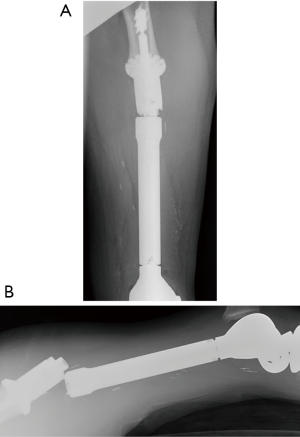
After scrutinizing the films, it was clear that the mechanism of failure was fracture of the male portion of the taper adapter adjacent to where it entered the diaphyseal segment (Figure 1B). The simplest possible surgery, therefore, would involve disengaging the taper adapter from the Compress spindle, replacing it with a new adapter, and replacing the diaphyseal segment. This strategy would retain the existing Compress, which was felt to be important in order to maintain the length of the short segment of native bone proximally.
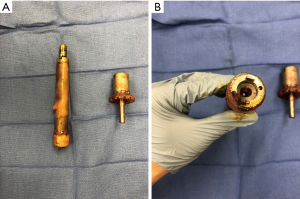
The surgery was done with general anesthesia and the patient in the supine position. His previous longitudinal medial thigh incision was used, and a deep interval just posterior to the vastus medialis proximally that extended to a medial parapatellar approach to the knee was utilized to expose the implant and proximal femur. The fracture was identified, and confirmed to be at the male portion of the taper adapter (Figure 2). We attempted to disengage the taper adapter from the spindle, but deformed two pitch-fork removal devices in the process and failed to remove it using a bone tamp. It became clear at this point that the two implants were cold-welded together. There were two reasonable options: (I) the entire Compress device could be removed, which would require identifying and removing the anchor pins, disrupting the implant-bone interface, and re-cutting the proximal femur or (II) we could attempt to remove only the spindle and centering sleeve, leaving the existing anchor plug in place. The second option was favorable as it would minimize shortening of the existing proximal femur and eliminate the need to strip periosteum proximally to identify the anchor pin sites. However, the cold-welded taper adapter was blocking access to the Compress nut, which holds the spindle onto the anchor plug traction bar.
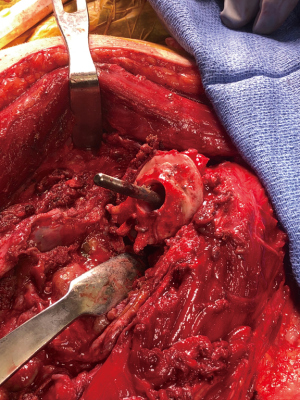
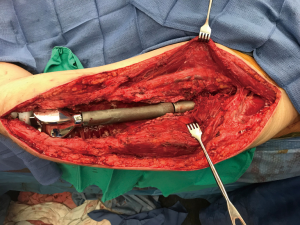
To gain access to the nut, the distal aspect of the taper adapter was resected using a metal-cutting wheel. This was done while taking extreme care to protect the soft tissues, using copious irrigation, and switching out cutting wheels when they became dull. Once the taper adapter was cut, the distal portion was removed and the Compress nut was accessed and removed (Figure 3). The anti-rotation pins were removed, and the spindle-bone interface was disrupted using a combination of flexible osteotomes and microsagittal and Gigli saws. Only a few millimeters of proximal bone were removed (Figure 4). This stage was done very carefully, as removing too much bone could have resulted in an altered position of the spindle on the traction bar, potentially eliminating the ability to apply compression, which would have resulted in the need for a more proximal anchor plug (6). We then freshened the bone surface, placed a new spindle, taper adapter, and diaphyseal segment, and completed the revision reconstruction (Figure 5). The wound was closed in layers over two deep drains, and the patient was kept protected weight-bearing with enoxaparin for thromboprophylaxis.

Discussion
In the case above, we report on mechanical failure of a Compress implant at the taper adapter as it enters the proximal diaphyseal segment. Additionally, the taper adapter was cold welded to the spindle, preventing access to the compression nut.
In one previous case series following patients treated with the Compress implant, Calvert et al. report a 30% rate of implant removal among 50 patients (1). In that study, the most common reason for revision was aseptic failure (seven of 15 revisions). Most of these occurred early, with a mean time to failure of eight months, and none of the implants failed aseptically after 17 months (1). A second study reported 85% survival at five years among a cohort of 28 patients. In that cohort, failures were either fixation failure, bone failure, or a combination of these (2). In the current study, we report on a late (seven years) failure at the taper adapter-diaphyseal junction not involving the bone-implant interface, which is not described in the previous studies. This may be due to the high activity level of our patient, ultimately causing fatigue failure of the implant.
In conclusion, failure at the modular junction of a Compress device is possible, as is cold welding of the taper adapter onto the spindle. The use of a metal cutting wheel to remove the distal aspect of the taper adapter to access the compression nut was effective and safe, although multiple wheels were required. In this situation, the anchor plug can be salvaged and proximal bone preserved.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Kurt R. Weiss and Stella Lee) for the series “Osteosarcoma” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.08.01). The series “Osteosarcoma” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Calvert GT, Cummings JE, Bowles AJ, et al. A Dual-center Review of Compressive Osseointegration for Fixation of Massive Endoprosthetics: 2- to 9-year Follow up. Clin Orthop Relat Res 2014;472:822-9. [Crossref] [PubMed]
- Healey JH, Morris CD, Athanasian EA, et al. Compress® Knee Arthroplasty Has 80% 10-year Survivorship and Novel Forms of Bone Failure. Clin Orthop Relat Res 2013;471:774-83. [Crossref] [PubMed]
- Schwartz AJ, Kabo JM, Eilber FC, et al. Cemented Distal Femoral Endoprostheses for Musculoskeletal Tumor: Improved Survival of Modular versus Custom Implants. Clin Orthop Relat Res 2010;468:2198-210. [Crossref] [PubMed]
- Whittaker RK, Zaghloul AM, Hothi HS, et al. Clinical Cold Welding of the Modular Total Hip Arthroplasty Prosthesis. J Arthroplasty 2017;32:610-5. [Crossref] [PubMed]
- Kop AM, Keogh C, Swarts E. Proximal Component Modularity in THA—At What Cost?: An Implant Retrieval Study. Clin Orthop Relat Res 2012;470:1885-94. [Crossref] [PubMed]
- Abrams GD, Gajendran VK, Mohler DG, et al. Surgical Technique: Methods for Removing a Compress® Compliant Prestress Implant. Clin Orthop Relat Res 2012;470:1204-12. [Crossref] [PubMed]
Cite this article as: Campbell ST, Roe AK, Avedian RS. A technique for anchor plug salvage in the setting of a cold welded taper adapter following compress implant failure. Ann Joint 2019;4:33.


