Posterolateral structure reconstruction for the chronic multiple ligament injuries of the knee
Introduction
Combined anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) injuries results in severe functional disability of the knee (1,2). The posterolateral structure (PLS) injuries are commonly associated with PCL and/or ACL injuries (3) by traffic accident or high energy trauma. The PCL is the primary restraint structure to posterior tibial translation of the knee. The PLS injury promote the functional disability of the PCL insufficiency (4). The PLS deficiency provides high forces to the PCL, which may cause an elongation of a PCL graft (5). The PLS resists varus stress of the knee, external rotation and posterior translation of the tibia. Previous studies reported that lateral collateral ligament (LCL), popliteus tendon (POP), and popliteofibular ligament (PFL) are the important PLSs of the knee (6-9). However, the treatment strategy for combined ligamentous injuries of the knee with PLS insufficiency remains controversial.
The authors have been performed PLS reconstruction using an autogenous biceps femoris tendon (BFT) for the chronic posterolateral (PL) instability of the knee (10,11). In addition, recently, the authors have developed double-bundle PCL reconstruction procedure using autogenous hamstring tendon ‘hybrid’ grafts which are connected meshed polyester tapes (12). In this article, the surgical technique, and clinical outcomes of PLS reconstruction for the chronic PLS insufficiency with ACL and/or PCL ruptures.
Surgical procedure
Graft preparation
The patient is placed supine position on the operating table under general anesthesia. Pneumatic tourniquet is applied to the proximal thigh of the bilateral lower limbs. C-arm fluoroscopy comes in from the operative side of the table. The surgeon confirms to keep the femur horizontal, hanging the lower limb at 90° of knee flexion, and change the 4 figure position on the operation table. The patient undergoes draping with the bilateral lower limbs placed in a stockinet to a position distal to the tibial tubercle under aseptic condition. Lactate Ringer solution is used for inflow with gravity.
Autogenous tendon grafts for all ligament reconstructions are used. The graft choice is critical for the postoperative knee function and graft site morbidity. The authors select an appropriate autogenous tendon graft from the semitendinosus tendon (Semi-T) and gracilis tendon (Gr), the bone-patellar tendon-bone (BTB), the quadriceps tendon-bone, or the BFT for each injured ligament.
For PLS reconstruction, the anterior half of a BFT is used. The Semi-T and Gr are harvested from the opposite side of the knee for PCL reconstruction to avoid the reduction of the hamstring muscle strength of the injured side. The Semi-T, the quadriceps tendon-bone, or the BTB from the same side of the knee is used for ACL reconstruction. The ACL and PCL grafts are prepared.
For ACL reconstruction, a Semi-T is cut in half. Each Semi-T is doubled and the two free ends are sutured with a 2-0 polyester thread using the circumferential ligation suture technique (13). Then, a 10-mm polyester mesh tape (Neoligament; Leeds-Keio Artificial Ligament, Leeds, England) is attached to the tibial side of the ACL grafts (14,15). After measurement of the femoral tunnel length, an Endobutton-CL-BTB (Smith & Nephew Endoscopy, Andover, MA, USA) is attached to the tendon loop of the femoral side. A distal portion of the Semi-T (diameter: 6–7 mm, length >650 mm) is used for anteromedial (AM) bundle graft of ACL reconstruction, and a proximal portion of the Semi-T (diameter: 5.5–6 mm, length >500 mm) is used for PL bundle graft.
For PCL reconstruction, the other Semi-T is cut in half. The harvested Gr length matches the length of the half Semi-T. One of the half Semi-T and Gr are doubled (diameter: 8–9 mm, length >700 mm), and a polyester tape is connected at each end in the same manner as the ACL graft. This graft is used for the anterolateral (AL) bundle graft of PCL reconstruction. The remaining half Semi-T is also doubled (diameter: 6–7 mm, length >800 mm), and a polyester tape is connected at each end in the same manner. This graft is used for the posteromedial (PM) bundle graft.
ACL reconstruction
A longitudinal medial and lateral parapatellar portals are created in arthroscopy. After the ACL remnant tissue is removed using the knife, the tibial and femoral attachment of the ACL are identified. Then, the centres of the femoral and tibial footprints are marked using the radiofrequency device. The trans-tibial tunnel technique is used for ACL reconstruction (13). First, a guidewire is inserted to the centre of the tibial attachment using a hole-in-one guide (Wire-Navigator, Smith and Nephew KK, Tokyo, Japan). Then, the surgeon should confirm whether the guidewire position is appropriate using a fluoroscopy. The authors recommended that the tibial tunnel angles averaged approximately 45° measured as the angle subtended by the axis of the tibial tunnel and the long axis of the tibia in the anteroposterior view. The tibial tunnel is created with a cannulated drill. The diameter of the tibial tunnel is same as the ACL graft diameter. The femoral tunnel is created at the point of the 2 o’clock position (Left knee) using a 5-mm off-set guide (Arthrex, Naples, FL, USA) (15). After a guidewire is inserted, the femoral tunnel is created using a 4.5-mm cannulated drill. The femoral tunnel length is measured using the probe. Then, the femoral socket is created step by step using a half-cannulated drill (Smith and Nephew Endoscopy, Andover, MA, USA).
PCL reconstruction
Second, tunnels for PCL reconstruction are created. The femoral attachment of the PCL remnant tissue is resected from the femoral medial condyle. After creating the PM portal from the PM aspect of the knee, the tibial attachment of the PCL is resected on the posterior tibia using a shaver system. A tibial drill guide (The ACUFEX Director PCL Tibial Aimer, Smith and Nephew Endoscopy) is inserted from the AM portal. The intraarticular tip of the guide is fixed at the centre of the PM bundle attachment (the medial-distal portion within the PCL attachment) on the posterior cortex of the tibia. The proximal end of the guidewire sleeve is fixed on the AM aspect of the proximal tibia. A guidewire is inserted into the tibia. The tip of the guidewire is confirmed under C-arm. Then, anterolateral longitudinal incision is created on the proximal tibia. After the retinaculum of the tibialis anterior is cut longitudinally, the tibialis anterior is released laterally. The tibial drill guide (Smith and Nephew Endoscopy) is inserted from the AL portal. The intraarticular tip of the guide is fixed to the centre of the AL bundle attachment on the posterior tibia (the lateral-proximal portion within the PCL attachment). The proximal end of the guide wire sleeve is fixed on the anterolateral aspect of the proximal tibia, because of decreasing the killer turn angle of the AL tibial tunnel. The AL graft passage is also easier in the AL tibial tunnel than in the AM tibial tunnel. A guidewire is inserted in the same manner. The guidewire positions are identified at the tibial posterior cortex using C-arm. If the inserted guidewire is located inappropriate position, the guidewire is changed using a parallel dill guide. The PM and AL tibial tunnels are created using a cannulated drill. During this procedure, the drill tip is identified to avoid popliteal nerve and vascular injuries using the PM portal.
Then, two femoral tunnels are created using the outside-in technique. A longitudinal incision is made on the medial femoral condyle. After cutting the fascia, the vastus medialis obliquus is retracted anteriorly to identify the medial femoral condyle. Surgeon should confirm the medial patellofemoral ligament for avoiding injury. The femoral PCL attachment is identified from an AM parapatellar portal. Then, the centres of the AL and PM bundle are marked using the radiofrequency device. Two guidewires are inserted using an outside-in guide (The ACUFEX Director PCL Femoral Aimer, Smith and Nephew Endoscopy). The AL and PM femoral tunnels are created from the femoral lateral condyle using a cannulated drill.
PLS reconstruction
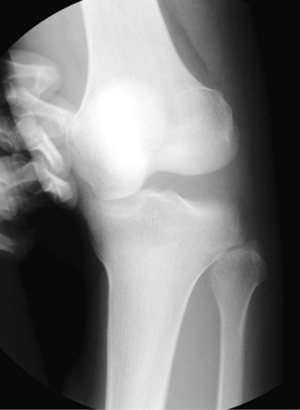
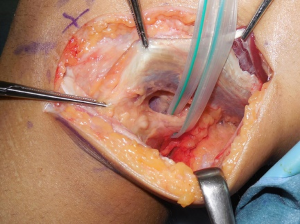
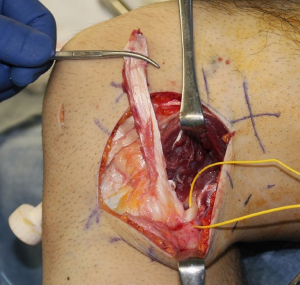
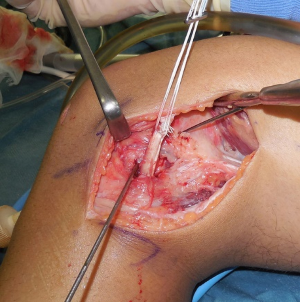
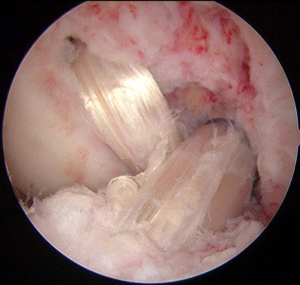
The authors have been used the BFT for PLS reconstruction as the modified Clancy method (10,11). An AL incision is made on the posterolateral aspect of the knee. After the subcutaneous tissue is undermined, the iliotibial band (ITB) and the BFT are identified. After the ITB is retracted anteriorly, the injured LCL is identified. The peroneal nerve is located on the PL aspect of the proximal fibula. The peroneal nerve is carefully released from the proximal fibula and the posterior of the BFT (Figure 1). The tendon portion of the biceps is released from the muscle portion. Then, the anterior portion of the BFT is released from the proximal portion (Figure 2). The BFT graft is created according to the previous studies (10,11). The fibular insertion of the BFT is preserved. The proximal end of the BFT is divided into the two portions longitudinally. An adjustable cortical fixation system (The ACL TightRope RT, Arthrex, Naples, FL, USA) is rigidly connected to the proximal portion of the BFT graft (Figure 3) using the 2-0 polyester thread. Then, the lateral epicondyle of the femur is identified. The LCL attachment on the femur is located at slightly proximal and posterior to the femoral lateral epicondyle. A guidewire is inserted from this point. Surgeon must avoid the tunnel convergence to the femoral ACL tunnel. The femoral tunnel of the PLS reconstruction is created with a 4.5-mm cannulated drill. After a measurement of femoral tunnel length, the femoral socket is created to the graft diameter using a cannulated drill (Figure 4).
Pearls and pitfalls are shown in Table 1. The BFT is a useful graft in PLS reconstruction for the posterolateral instability of the knee. The authors have been used an adjustable cortical fixation system for the femoral side fixation of the PLS graft, because graft tension can be easily applied during surgery. It is a technically simple procedure. The surgeon should confirm multiple ligament injuries of the knee including several manual tests under anesthesia and intraarticular conditions using MRI and arthroscopy. The surgeon should avoid tunnel convergence in ACL and PLS reconstructions. The peroneal nerve should be carefully released from the proximal fibula and the posterior of the BFT. The surgeon should confirm the BFT, because the BFT is sometimes injured in multiple ligament injuries of the knee particularly knee dislocation. The preoperative rehabilitation including the range of knee motion in the acute stage after injury are of importance for the following surgery. The long surgical time is the risk of intra-articular infection. Advantages and limitations are shown in Table 2. The PLS reconstruction using the BFT provides knee stability against the varus stress on knee extension position. The BFT is thicker than the LCL of the knee. Previous biomechanical studies reported that the rotational knee laxity in response to both external rotation and posterior translation load were significantly better after the anatomical multiple-strand PLS reconstruction than after the modified LCL reconstruction.

Full table

Full table
Graft fixation
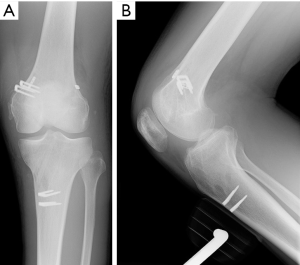
First, the PM graft for PCL reconstruction is introduced from the tibial PM tunnel to femoral PM tunnels. Then, the AL graft for PCL reconstruction is passed through the tibial and femoral AL tunnels. The femoral side of the two PCL grafts are fixed to the medial femoral condyle with two staples. Then, the ACL graft is introduced from the tibial tunnel to femoral tunnel using a passing pin. The Endobutton of the ACL graft is flipped, and fixed on the lateral femoral condyle (Figure 5). Then, the BFT graft is introduced to the PLS tunnel. The Endobutton of the PLS graft is fixed to the medial femoral condyle (Figure 6). Next, the two PCL graft are tensioned manually at 90° of knee flexion by applying an anterior drawer force to the tibia to obtain an anatomic position. Surgeon should conform a reduction of tibial sagging. Finally, the knee is positioned at 10° of knee flexion. The 60-N force is applied to the ACL graft using the tension meter. The ACL and PCL grafts are fixed to the medial aspect of the proximal tibia using two staples. The graft for the PLS reconstruction is also tensioned for the final graft fixation avoiding the varus position.

Clinical outcome
Ten patients (10 knees) who sustained chronic PLS injury with ACL and/or PCL injury were enrolled in this study. There were 10 men with a mean age of 30 (range, 17–51) years at the time of surgery. All the patients were treated in the chronic phase. Seven cases required both ACL and PCL reconstructions using the Semi-T and Gr hybrid autografts. Three cases required ACL reconstruction using the Semi-T hybrid autografts. PLS reconstruction was performed using the BFT hybrid autograft. The patients were examined at 2 years after surgery. At the last follow-up, 3 patients who had the common peroneal nerve palsy showed functional recovery. No patients showed a loss of extension of the knee more than 5°, while 1 patient revealed a loss of flexion more than 15°. The side-to-side difference in the anterior-posterior translation of the knee measured at 20° and 70° averaged 2.2 (SD, 1.9) and 3.7 (1.8) mm, respectively. Varus and valgus, anterior-posterior stress radiographs showed no significant differences in comparison with that of the uninjured knee. The Lysholm score averaged 90.3 (6.6) points. In the International Knee Documentation Committee (IKDC) evaluation, 4, 3, and 3 patients were graded as A, B, and C, respectively.
Case report
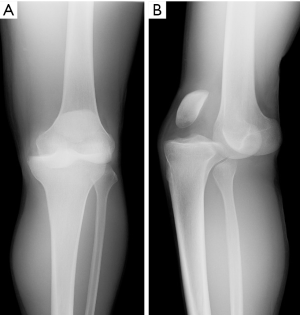
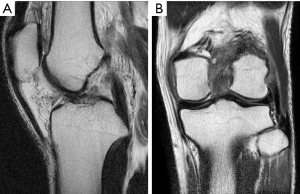
A 21-year-old man presented with spontaneously relocated left knee dislocation after a high-energy bike accident. Radiographs showed a complete anterior dislocation of the tibia to the femur (a posterior dislocation of the femur to the tibia) (Figure 7). There were no signs of vascular impairment based on the contrast-enhanced computed tomography (CT) (Figure 8). After reduction of the knee dislocation, left knee showed hyper varus instability (Figure 9), with suspected ruptures of the ACL, PCL, and PLS. He had a peroneal nerve palsy. Radiographs showed no abnormalities. Left knee was immobilised with an extension knee brace. Magnetic resonance imaging (MRI) of the left knee showed ruptures of the ACL, PCL and LCL (Figure 10). After recovering a peroneal nerve palsy, the authors performed single-bundle ACL, double-bundle PCL, and PLS reconstruction (Figure 11). At 2 years after surgery, he had a full range of knee motion. The side to side difference of anterior-posterior knee laxity averaged 2 mm. Lysholm knee score was 90 points.
Discussion
The present study demonstrated that one stage PLS, ACL and/or PCL, reconstruction for chronic combined knee instabilities can be safely performed using autografts. Clinical scores were favorable, and the postoperative knee stability was good without loss of knee extension. However according to the IKDC evaluation, three patients were abnormal (Grade C). One important factor contributing to the unfavorable IKDC rating in some patients was knee contracture that had already existed before surgery. This result indicated that the initial treatment and rehabilitation in the acute stage after injury are of importance for the following surgery.
Acute PLS injury is often found with ACL and/or PCL injuries. However, a true diagnosis of PLS injury is difficult in acute phase. Therefore, surgeon need to take PLS injury into account in multiple injury of the knee using various manual test; external rotation recurvatum test, posterolateral drawer test, reverse pivot shift test, and dial test, etc. In the acute PLS injury can be treated with conservative treatment, primary repair, or augmentation depending on various instability grades (16). However, it is considered that grade II PLS injury with multiple knee ligament injury, grade III PLS injury, and an avulsion fracture of PLS injury are surgical indication.
Recently, chronic PLS deficiency has been treated by reconstructions with various levels of combined injury of the knee to restore the functions of the damaged structures. The Larson reconstruction (17) is commonly performed, the graft strands approximate the LCL (18,19). Clancy et al. (11) reported that a part of the BFT, left pedicled on the head of fibula, was harvested. The BFT was passed behind the remaining third of the bicipital tendon and attached in the popliteal fossa of the femur, in a blind tunnel, using an interference screw or a tendon anchor. Kim et al. (20) reported clinical outcome of BFT rerouting technique for PLS instability of the knee. Results showed that 93% of cases had negative reverse pivot shift test after surgery. Fanelli et al. (21) also described that PLS reconstruction was performed using BFT tenodesis. They reported that PLS stability was obtained to normal in 97% of cases with varus stress test at 30° of knee flexion. The side-to-side difference in posterior laxity measured with KT-1000 averaged 2.1 mm. Postoperative mean Lysholm knee score was 91.7 points. They concluded that PLS reconstruction with BFT tenodesis and posterolateral capsular shift was effective treatment for PLS insufficiency. The authors (10) modified to secure the BFT graft for PLS reconstruction in the bony tunnel. LaPrade et al. (22) introduced a 3-strand PLS reconstruction, with grafts replacing the LCL, a ‘‘popliteus bypass’’ from the femoral POP attachment to the PL tibia, and a PFL that passed across the posterior tibiofibular joint to the PL tibia. Recently, Jakobsen et al. (23) reported a new 4-strand PLS reconstruction has been developed. Miyatake et al. (24) reported that that the rotational knee laxity in response to both external rotation and posterior translation load were significantly better after the 4-strand PLS reconstruction than after the modified Larson reconstruction. However, significant differences were not found between the 2 procedures concerning the varus laxity. Although biomechanical stabilities were significantly better in the 3 or 4 strand PLS reconstruction than in Larsen procedure, 3 or 4 strand PLS reconstruction technique have complex procedures, such as invasive tunnel creation, necessities of autogenous long Semi-T graft or allograft. Therefore, the authors selected the simple technique of the modified Clancy methods for PLS reconstruction in chronic multiple knee ligament injuries. However, the long-term follow-up examination is needed for PLS reconstruction, particularly concerning external rotation instability. In addition, the lower limb alignment is very important factor in the multiple ligament insufficiency. Therefore, surgeon should take notice of varus knee in chronic PLS insufficiency. The authors consider that high tibial osteotomy is one of the treatments for chronic PLS instability with varus knee alignment (25).
Tunnel convergence is greater in combined ACL and PLS reconstruction. Shuler et al. noted that to minimize the potential risk for tunnel collision, the surgeon should maintain a neutral alignment in the coronal plane, limit lateral tunnel depth to >25 mm, and direct the lateral tunnel anteriorly in the axial plane to a maximum of 40° (26). It has been suggested that POP tunnels should be drilled at 30° axial/30° coronal angulations, and LCL tunnels should be drilled at 30° axial/0° coronal angulations (27). Gali et al. reported that drilling POP and LCL femoral tunnels at 20° axial/20° coronal angulation is a safe positioning for simultaneous ACL and PLS reconstructions (28). In PLS reconstruction, first, a guidewire was inserted to the femoral tunnel of ACL reconstruction. Then, a guidewire of the BFT tunnel was passed though the anterolateral side of the knee. Therefore, it is possibility that the surgeon can avoid the tunnel convergence in PLS reconstruction.
Acknowledgments
Funding: This work was financially supported in part by a Grant-in-Aid for Scientific Research (16H03158) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Takeshi Muneta) for the series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.08.04). The series “Anatomic Reconstruction of Anterior Cruciate Ligament - Concept, Indication, and Its Efficacy” was commissioned by the editorial office without any funding or sponsorship. EK reports Grant/Research funding from Olympus Terumo Biomaterials, Japan, Smith and Nephew, Japan, Yufu Itonaga Co., Ltd., Japan, Mochida Pharmaceutical Co., Ltd., Japan, other from Centre for Sports Medicine, Hokkaido University Hospital. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations. A meta-analysis. Am J Knee Surg 2001;14:33-8. [PubMed]
- Richter M, Bosch U, Wippermann B, et al. Comparison of surgical repair or reconstruction of the cruciate ligaments versus nonsurgical treatment in patients with traumatic knee dislocation. Am J Sports Med 2002;30:718-27. [Crossref] [PubMed]
- Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy 1996;12:521-30. [Crossref] [PubMed]
- Race A, Amis AA. Loading of the two bundles of the posterior cruciate ligament: an analysis of bundle function in A-P drawer. J Biomech 1996;29:873-9. [Crossref] [PubMed]
- Harner CD, Vogrin TM, Höher J, et al. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med 2000;28:32-9. [Crossref] [PubMed]
- Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee: a biomechanical study. J Bone Joint Surg Am 1987;69:233-42. [Crossref] [PubMed]
- Grood ES, Stowers SF, Noyes FR. Limits of movement in the human knee: effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am 1988;70:88-97. [Crossref] [PubMed]
- Pasque C, Noyes FR, Gibbons M, et al. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br 2003;85:292-8. [Crossref] [PubMed]
- Veltri DM, Deng XH, Torzilli PA, et al. The role of the popliteofibular ligament in stability of the human knee: a biomechanical study. Am J Sports Med 1996;24:19-27. [Crossref] [PubMed]
- Hayashi R, Kitamura N, Kondo E, et al. Simultaneous anterior and posterior cruciate ligament reconstruction in chronic knee instabilities: surgical concepts and clinical outcome. Knee Surg Sports Traumatol Arthrosc 2008;16:763-9. [Crossref] [PubMed]
- Clancy WG Jr. Combined posterior cruciate ligament injuries. Clin Sports Med 1994;13:629-47. [PubMed]
- Yasuda K, Kitamura N, Kondo E, et al. One-stage anatomic double-bundle anterior and posterior cruciate ligament reconstruction using the autogenous hamstring tendons. Knee Surg Sports Traumatol Arthrosc 2009;17:800-5. [Crossref] [PubMed]
- Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 2004;20:1015-25. [Crossref] [PubMed]
- Kondo E, Yasuda K, Azuma H, et al. Prospective clinical comparisons of anatomic double-bundle versus single-bundle anterior cruciate ligament reconstruction procedures in 328 consecutive patients. Am J Sports Med 2008;36:1675-87. [Crossref] [PubMed]
- Kondo E, Yasuda K, Miyatake S, et al. Clinical comparison of two suspensory fixation devices for anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2012;20:1261-7. [Crossref] [PubMed]
- Spitzer E, Doyle JB, Marx RG. Outcomes of surgical treatment of posterolateral instability of the knee. J Knee Surg 2015;28:471-4. [Crossref] [PubMed]
- Larson RV. Isometry of the lateral collateral and popliteofibular ligaments and techniques for reconstruction using a free semitendinosus tendon graft. Oper Tech Sports Med 2001;9:84-90. [Crossref]
- Davies H, Unwin A, Aichroth P. The posterolateral corner of the knee: anatomy, biomechanics and management of injuries. Injury 2004;35:68-75. [Crossref] [PubMed]
- Khanduja V, Somayaji HS, Harnett P, et al. Combined reconstruction of chronic posterior cruciate ligament and posterolateral corner deficiency: a two- to nine-year follow-up study. J Bone Joint Surg Br 2006;88:1169-72. [Crossref] [PubMed]
- Spitzer E, Doyle JB, Marx RG. Outcomes of surgical treatment of posterolateral instability of the knee. J Knee Surg 2015;28:471-4. [Crossref] [PubMed]
- Fanelli GC, Edson CJ. Combined posterior cruciate ligament-posterolateral reconstructions with Achilles tendon allograft and biceps femoris tendon tenodesis. 2- to 10-year follow-up. Arthroscopy 2004;20:339-45. [Crossref] [PubMed]
- LaPrade RF, Johansen S, Wentorf FA, et al. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 2004;32:1405-14. [Crossref] [PubMed]
- Jakobsen BW, Lund B, Christiansen SE, et al. Anatomic reconstruction of the posterolateral corner of the knee: a case series with isolated reconstructions in 27 patients. Arthroscopy 2010;26:918-25. [Crossref] [PubMed]
- Miyatake S, Kondo E, Tsai TY, et al. Biomechanical comparisons between 4-strand and modified Larson 2-strand procedures for reconstruction of the posterolateral corner of the knee. Am J Sports Med 2011;39:1462-9. [Crossref] [PubMed]
- Savarese E, Bisicchia S, Romeo R, et al. Role of high tibial osteotomy in chronic injuries of posterior cruciate ligament and posterolateral corner. J Orthop Traumatol 2011;12:1-17. [Crossref] [PubMed]
- Shuler MS, Jasper LE, Rauh PB, et al. Tunnel convergence in combined anterior cruciate ligament and posterolateral corner reconstruction. Arthroscopy 2006;22:193-8. [Crossref] [PubMed]
- Gelber PE, Erquicia JI, Sosa G, et al. Femoral tunnel drilling angles for the posterolateral corner in multiligamentary knee reconstructions: computed tomography evaluation in a cadaveric model. Arthroscopy 2013;29:257-65. [Crossref] [PubMed]
- Gali JC, Bernardes Ade P, dos Santos LC, et al. Tunnel collision during simultaneous anterior cruciate ligament and posterolateral corner reconstruction. Knee Surg Sports Traumatol Arthrosc 2016;24:195-200. [Crossref] [PubMed]
Cite this article as: Kondo E, Joutoku Z, Matsubara S, Iwasaki K, Onodera T, Yasuda K, Yagi T, Iwasaki N. Posterolateral structure reconstruction for the chronic multiple ligament injuries of the knee. Ann Joint 2019;4:43.