Scintigraphic abnormalities of tibialis posterior tendonitis and their importance
Introduction
Tibialis Posterior Tendonitis (TPT) is a common injury of the foot and ankle, of arguable aetiology. Numerous hypotheses are tendered regarding the cause ranging from overuse of the Tibialis Posterior muscle to degeneration associated with a watershed area of the tendon. It was first described by Johnson and Strom (1) in 1989.
Less controversial than the aetiology is the clinical course where the inflammation of the tendon initially presents with severe pain and swelling in the posteromedial aspect of the ankle that worsens with activity (Figure 1). It is more uncomfortable during walking, prolonged standing and when using stairs, especially downstairs.
Due to the high incidence of this condition (particularly in the middle-aged and obese population), it is a frequent diagnosis that Orthopaedic Surgeons need to make.
However, these symptoms are not unique to TPT and an important differential diagnosis of pain in this region is a stress fracture of the postero-medial tibia, sprains of the ankle, arthritis in the ankle or subtalar joint, even unsuspected tarsal coalitions.
Differentiating between these conditions is extremely important, as if TPT is left untreated, it can result in attenuation and stretching of the tendon. This can be problematic, as lengthening of the tendon results in weakness of the muscle, and leads to the condition progressing in a late stage of the disease, to a chronic, debilitating condition that is the most common cause of adult acquired flat-foot deformity—termed Tibialis Posterior Tendon Dysfunction (Figure 2). Often, progression to this stage will require the patient to undergo surgical correction.

So, it is most beneficial to intervene early and prevent the progression of the disease which can be treated with the use of a specific orthotic known as a UCBL, which can prevent the progression from Tendonitis to Dysfunction. The incidence of successful outcomes of conservative treatment in the literature is not clear, as many different devices and criteria for outcome are used, but the patients in this cohort universally settled with the use of a UCBL orthotic.
Investigations
All of the possible diagnoses listed above can be imaged by a magnetic resonance imaging (MRI), and this would be a common investigation used to diagnose the condition.
We acknowledge that this is the most appropriate investigation to undertake when possible. However, MRI is costly and has limited availability in some places, which can lead to significant delays in obtaining these images.
In contrast, a Bone Scan is a convenient, cheap and more readily available imaging method, which may have already been done as part of the standard investigation for a stress fracture.
Bone scans are an imaging technique that involves an injection of technetium-99, which is bound to a carrier molecule, usually a Methyl Diphosphate (2,3). The technetium-99 undergoes radioactive decay, and the emissions of the Te99 is detectable with a gamma camera and can be printed on film.
Technetium has no affinity for bone, and it is the carrier is the molecule that provides the specificity of the test as these binds to bone. After injection, the radionuclide travels through the blood and interacts with the bone. In the bone, the tracer binds to hydroxyapatite crystals in proportion to the blood flow and osteoblast activity in the area.
The technetium-99 is then visible with specialised cameras. This final binding results in the bone phase of imaging. The bone phase is suitable for assessment of the biological activity of the bone, as it shows evidence of bone growth, mechanical stress and pathology within the bone.
However, during a bone scan, there are two other phases of imaging that have utility and are routinely performed during bone scans. The first is a blood-flow phase image, which is attained during the injection of the technetium-tracer hybrid compound and is used to assess regional blood flow. The second is the blood-pool phase, which is obtained during the first 1–2 minutes after the injection has been made, to assess whether increased tissue vascularity and capillary leakage cause the blood and radionuclide to pool in the area. Given that tissue vascularity and capillary leakage are key hallmarks of inflammation, this imaging technique can be used to identify the inflammatory regions of joints and tendons (3-14) when examined carefully.
Since localised inflammation is evident in the early stages of the pathogenesis of TPT, report will document cases where a bone scan confirmed the diagnosis of Tibialis Posterior Tendontis. By examining the blood-pool phase of individuals it will be possible to appreciate the utility of the bone scan as a diagnostic tool.
Case presentation
In this paper we describe a series of patients in whom bone scans were performed, but the diagnosis of Tibialis Posterior Tendonitis was not recognised by the consultant radiologists, and some of these patients went on to have a MRI, and others the diagnosis was made by the senior author who then reviewed the images and could identify abnormalities that would have led to the diagnosis had the clinical situation been known.
Case 1
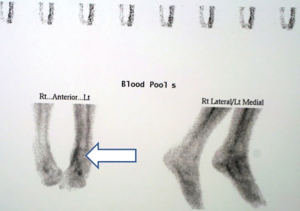
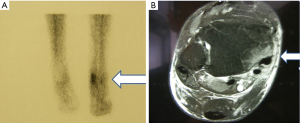
Figure 3 shows the bone scan and MRI of patient BM, a 65-year-old female who complained of a “sprained ankle” on the medial side. After treatment from a physiotherapist failed to alleviate the pain, she was consulted her GP and was assessed.
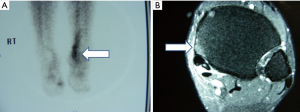
Figure 3A shows a region of high-density bone tracer on the medial aspect of the right ankle, suggestive of localised inflammation in the region. As a key hallmark of TPT and not a stress fracture, it was now possible to make a diagnosis based on the clinical findings and the imaging test.
BM then received a MRI of the ankle to verify the initial diagnosis, looking for the peritendinous fluid in the posterior tibialis tendon that is visible in Figure 3B. Not only did this scan reveal the inflamed tendon, it also showed an area of increased signal in the cortical and subcortical region of the tibia adjacent to the tendon, signifying that the bone is reacting to the inflammation of the tendon. It is this reactivity that is visible on the bone scan and provides utility for it as a diagnostic tool when a MRI is unavailable. Once the diagnosis of TPT was confirmed, BM was treated with a UCBL orthotic for 6 months, until the issue resolved.
Case 2
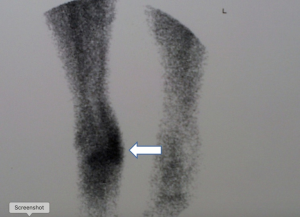
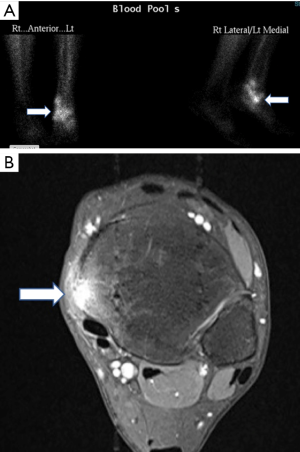
The Figure 4 contains the radiography from patient CL, a 65-year-old male with a 3-month history of pain in the posteromedial region of the right ankle. Again, Figure 4A shows a similar pattern of tracer density over the medial portion of the right ankle. To confirm this diagnosis, MRI of CL’s ankle was taken and was found to demonstrate evidence of fluid build-up in the peritendinous region of the Tibialis Posterior tendon and increased bone activity in the portion of tibia bordering it. Again, in this investigation, the results of the MRI reflected the diagnosis that was originally made by examination of the bone scan. Once this diagnosis had been made, CL required the use of a UCBL for 8 months before resolution of his symptoms and was then able to walk afterwards, orthotic free.
Case 3
The images taken from patient KP tell a similar story. KP was a 59-year-old female who presented with a 6-month history of pain and swelling in her ankle. Originally this was diagnosed as gout, however through examination of her bone scan (visible in Figure 5A) it was evident that there was a large degree of capillary leakage in the posteromedial aspect of the leg, suggestive of TPT. Through the MRI investigation in Figure 5B, it was evident that the original diagnosis, made because of the bone scan, was incorrect and that KP was suffering from TPT. Because of the early detection of this disorder, a UCBL orthotic could be used for 8 months before the symptoms settled. Then the orthotic could be abandoned as normal function had been restored.
Case 4
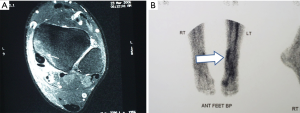
MB was a 57-year-old lady with 4 months on symptoms in the ankle after a vague “stumble”. Not settled with Physio (Figure 6). Treated with NSAID’s and UCBL for 8 months with resolution of her tendonitis
Case 5
LG was a 75-year-old lady with pain swelling and rolling over of ankle on the medial side. Pain with stairs. Not relieved with Podiatry Orthotics. Treated with UCBL with resolution of symptoms and signs over 6 months (Figure 7).
Case 6
JD was a 72-year old lady with pain in ankle not settled with Physio and Podiatry othotics. Provided with UCBL and resolution of pain and symptoms over 8 months. Images of her bone scan Figure 8A and MRI Figure 8B.
Discussion
We have reviewed the literature and found two articles which describes bone scan findings in Tibialis Posterior Tendonitis, however one (6), had a mixture of inflammatory arthritidies within the cohort, so did not specifically deal with primary Tibialis Posterior Tendonitis, and did not have the ability to correlate their findings with MRI (as these were unavailable at the time). This study also included individuals in the stage of dysfunction, not solely the inflammatory phase of the disease.
The second study (7) was a case report of a single patient who exhibited increased uptake in the blood pool and bony phase, and the histological findings suggested an inflammatory arthritis again, and thus may not be representative of degenerative Tibialis Posterior Tendonitis.
It is important to note that during the investigation of our cases was performed by the patients’ primary care physicians and the bone scan was taken as part of the workup for a suspected stress fracture or joint arthritis.
The Radiologist reports consisted of a negative result for these problems based on the Bone Phase of the bone scan.
Unfortunately, there was no comment made on the blood-pool phase of the bone scan which all showed increase uptake in the path of the Tibialis Posterior Tendon.
However, in those cases where an MRI had been taken, these patients were correctly diagnosed with Tibialis Posterior Tendonitis. Furthermore, each of these MRI’s show high signal intensity in the region of the posteromedial aspect of the tibia, beside the inflamed tibialis posterior tendon.
Thus, these MRI’s show evidence of some bone activity and this is visible on a bone scan. With this information in mind, the importance of the blood-pool phase of a Bone Scan in diagnosing TPT becomes apparent. As a routine investigation of posteromedial pain, it can be a method of detection of Tibialis Posterior tendonitis that would be highly useful in regions where an MRI is not accessible or too expensive or contra—indicated such as patients with pacemakers or spinal cord stimulators.
The images taken from our patients have shown that the Bone scan can be used to correctly identify Tibialis Posterior Tendonitis, if the correct phase of imaging is viewed.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vinod K. Panchbhavi and Maninder Shah Singh) for the series “Foot & Ankle Surgery” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.09.06). The series “Foot & Ankle Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Verbal informed consent was obtained from the patients for use of accompanying images, and permission granted for the use of them for medical education and publications. Assurances were given that the images would be deidentified.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johnson KA, Strom DE. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res 1989;196-206. [PubMed]
- Barber L, Bourke J, Gill G, et al. Three-phase bone scintigraphy in suppurative tenosynovitis. Clin Nucl Med 1995;20:928-9. [Crossref] [PubMed]
- Yang DC, Ratani RS, Mittal PK, et al. Radionuclide three-phase whole-body bone imaging. Clin Nucl Med 2002;27:419-26. [Crossref] [PubMed]
- Green JS, Morgan B, Lauder I, et al. The correlation of bone scintigraphy and histological findings in patellar tendinitis. Nucl Med Commun 1996;17:231-4. [Crossref] [PubMed]
- Van Damme K, De Coster L, Mermuys K, et al. Bone scan findings in calcific tendinitis at the gluteus maximus insertion: some illustrative cases. Radiol Case Rep 2017;12:168-74. [Crossref] [PubMed]
- Groshar D, Liberson A, Alperson M, et al. Scintigraphy of posterior tibial tendinitis. J Nucl Med 1997;38:247-9. [PubMed]
- Kannangara S, Bruce W, Hutabarat SR, et al. Scintigraphy in severe tenosynovitis of the tibialis posterior tendon. Clin Nucl Med 1999;24:694-5. [Crossref] [PubMed]
- Sopov W, Rozenbaum M, Rosner I, et al. Scintigraphy of de Quervain's tenosynovitis. Nucl Med Commun 1999;20:175-7. [Crossref] [PubMed]
- Kahn D, Wilson MA. Bone scintigraphic findings in patellar tendonitis. J Nucl Med 1987;28:1768-70. [PubMed]
- Shih WJ, Pulmano C. Demonstration of Achilles tendon rupture by three phase bone scintigraphy and MRI. Ann Nucl Med 2000;14:53-5. [Crossref] [PubMed]
- Sinha P, Kim A, Umans H, et al. Scintigraphic findings in peroneal tendonitis: a case report. Clin Nucl Med 2000;25:17-9. [Crossref] [PubMed]
- Gilula LA, Oloff L, Caputi R, et al. Ankle tenography: a key to unexplained symptomatology. Part II: Diagnosis of chronic tendon disabilities. Radiology 1984;151:581-7. [Crossref] [PubMed]
- Hodgson RJ, O'Connor PJ, Grainger AJ. Tendon and ligament imaging. Br J Radiol 2012;85:1157-72. [Crossref] [PubMed]
- McDougall IR. Skeletal scintigraphy. West J Med 1979;130:503-14. [PubMed]
Cite this article as: Peereboom J, Peereboom J. Scintigraphic abnormalities of tibialis posterior tendonitis and their importance. Ann Joint 2020;5:2.