
Contemporary surgical approaches for hip resurfacing
Introduction
Hip resurfacing arthroplasty can be performed through a variety of surgical approaches with the ideal candidate for hip resurfacing being a young, active patient with hip pain, limiting function and quality of life, with the diagnosis of hip osteoarthritis. It is clear that not all patients are candidates for hip resurfacing due to underlying pre-existing hip anatomy as well as quality of the bone (1). In general hip resurfacing should be avoided in patients with large femoral head/neck cysts (more than 1 cm in diameter), poor bone quality, significant dysplasia; in addition impaired kidney function, female gender and known metal sensitivity are contra-indications with metal on metal hip resurfacings (1). Because hip resurfacing has unique mechanisms of failure such as femoral neck fracture, surgical techniques to decrease the risk of vascular insult, component malposition, i.e., acetabular, femoral neck notching are critical. More importantly, short term failures with hip resurfacing due to limited surgeon experience can be further compounded by poor patient selection (2), inappropriate surgical exposure leading to poor implant positioning (3). In addition, hip resurfacing requires specific attention in regards to femoral component sizing, positioning as well as preparation where pathologies such as: osteophytes, cysts, retro-tilting of the femoral head will affect femoral component survivorship (4). The incidence of femoral neck fracture ranges from 0–4% (5-7) with osteonecrosis (ON) of the femoral head being the leading cause (8). Campbell et al. (8) found thermal necrosis at the cement bone interface in cases of both neck fracture and femoral component loosening, emphasizing the importance of performing an optimal cement technique while avoiding excessive cement penetration. Another key finding in that paper was edge wear on the acetabular component due to component acetabular component mal-positioning (i.e., >55° of abduction). In another retrieval study, Costa et al found a significantly higher percentage of empty lacunae (i.e., dead cells) in femoral heads where the posterior approach was used highlighting the importance of maintaining femoral head viability during surgical exposure (9).
The principles of choosing a surgical approach for either total hip replacement or hip resurfacing should be the same i.e. permit proper patient position; provide access to involved area for desired intervention; avoid damage to functionally important structures, i.e., inter-muscular and inter-nervous; approach should be extensile, should not be associated with greater complication rate and should be cosmetically acceptable. In addition, the approach has to be carefully chosen keeping in mind surgeon’s expertise, patient’s body habitus and previous surgical incisions around the hip. More importantly over the last 10 years, choice of surgical approach in total hip arthroplasty has been of significant interest in regards to optimize patient recovery, i.e., outpatient joint replacement, minimizing risk of dislocation and maximizing patient function (10) (Table 1). With the first generation of hip resurfacing of metal on polyethylene (11-13), a variety of surgical approaches were used: trans-trochanteric, anterior, posterior and Hardinge which were also used for total hip replacement with the caveat that hip resurfacing usually requires a longer incision for optimal exposure of the femoral head. With the current generation of metal on metal hip resurfacing, the posterior surgical approach is the most commonly used with modifications allowing for some preservation of the vascular supply to the femoral head which are at greater risk with this approach (14,15). The anterior, lateral approach and the trochanteric slide osteotomy preserve the ascending branch of the medial femoral circumflex artery as well as the insertion of the short external rotators as the hip is dislocated anteriorly. However, with the lateral- and trochanteric slide patients can suffer from abductor weakness and Trendelenburg gait. Whilst, the Hueter-anterior hip approach for hip resurfacing is not as common and requires specialty training, it does preserves the femoral vascularity without disruption of the abductors (16).
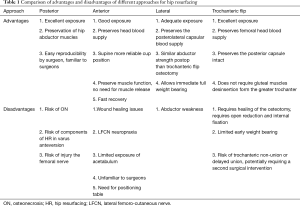
Full table
The goal of this review article is to present the three most common surgical approaches for hip resurfacing providing advantages and disadvantages.
Hueter-anterior approach
The anterior approach has been used increasingly in the last few years not only for THA but also for hip resurfacing (16,17). This approach was originally described in 1948 by Jean and Judet (18). The anterior approach for hip resurfacing is an approach with advantages and limitations. In expert hands it is optimal for minimal soft tissue damage and facilitating recovery.
Advantages
Preserves blood supply to the femoral neck by preserving the obturator externus tendon intact and when performing a circumferential capsular release and leaving a cuff of capsule; the retinacular vessels are preserved as well (15,19). Preserves muscles insertions on the femur as it is an intermuscular approach. Good exposure of femur and acetabulum. Fast recovery as there is minimal soft tissue manipulation and no muscle release. No abductor weakness and no Trendelenburg gait that can be present with other approaches resulting in adequate function postoperatively (20). With the patient in the supine position, cup orientation is more reliable facilitating intraoperative fluoroscopy to confirm proper acetabular component positioning (17).
Disadvantages
Technically challenging, requires expertise and a learning curve, as most orthopaedic surgeons are trained with other more common approaches such as posterior approach (21-23). When choosing the anterior approach for hip resurfacing the surgeon must have a clear understanding of the anatomy and orientation of the femur and acetabulum through the anterior approach with the patient supine and with the extremity in extension, external rotation for the femur and neutral flexion/extension with knee flexion and external rotation of the leg for the acetabulum. A positioning table is highly recommended and special instrumentation to allow adequate exposure and permit insertion of components with relative ease. A Spider-arm retractor might be useful for holding retractors from the contralateral side of the patient (Figure 1).
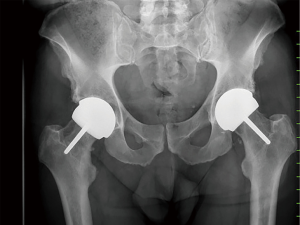
The incision of the anterior approach for hip resurfacing could require a more extensile incision for adequate manipulation and dislocation of the femoral head (24,25). In about 5–10% of cases, 1 to 1.5 cm of the tensor muscle is released at the iliac crest facilitating femoral head exposure. There is limited visualization of superolateral aspect of the femur and posterolateral aspect of the acetabulum compared with the posterior approach. Conversely, the ascending branch of MCFA as well as the retinacular vessels to the femoral head are not compromised (14). Possible complications of the procedure are femoral neck fracture, component malposition, lateral femoro-cutaneous nerve paresthesia (26), which itself is not associated with a limitation in function (17,26). Another critical component to consider is the learning curve which is comparable to more extensive surgical approaches at the first fifty procedures in a high volume arthroplasty surgeon, mainly in regards to acetabular component positions (Figure 2) (16).
Hardinge/lateral approach
Advantages
Preserves the posterolateral capsular blood supply of femoral head. Surgeons are in general familiar with the approach (6,27). It offers adequate exposure of the femoral head and acetabulum.
Disadvantages
Partial release of abductors off greater trochanter, giving postoperatively a Trendelenburg gait which can affect as much of 20% of cases (28). This can become permanent if the superior gluteal nerve is injured with most literature suggesting a safe distance of 5 cm proximal to the greater trochanter (29-33). Others have reported that with the lateral approach there is a risk of placing the femoral component into excessive valgus and retroversion (34). McBryde et al. (35) found no difference in implant survivorship or incidence of complications between posterior and lateral approach in hip resurfacing with a 97% survivorship at 8 years (35).
Posterior approach
Advantages
This is the most extensile approach to the hip (35). Most orthopaedic surgeons are trained in the posterior approach of the hip, making this a familiar approach for the general orthopaedic surgeon. It allows an excellent exposure of femur and acetabulum. It is an adequate exposure for significant deformity that might alter the normal anatomy.
Disadvantages
This approach requires release of the short external rotators being a more invasive and extensile technique (36). There is a higher risk of ON with this approach (37); exposure of the femoral neck might injure the retinacular vessels compromising the blood supply and potentially causing ON, by preserving a cuff of the posterior capsule this is decreased (15). Care must be taken when dissecting distal to the piriformis muscle as the MFCA has been described to be at the inferior aspect border of the piriformis anastomosing with the IGA. The sciatic nerve is at risk as well and should be protected throughout the procedure (14,19,29).
Preservation of gluteus maximus sling insertion is important in young active patients to preserve hip extension and hip function. The inferior gluteal nerve (IGN) and inferior gluteal artery (IGA) should be protected as well; the reported average distance between greater trochanter and the first crossing branch of IGN and IGA is 8.7 cm. At the superior border of the muscular portion of the piriformis the acetabular branch of the SGA has been identified (29,36). Positioning of the components in hip resurfacing through the posterior approach has special considerations. Kunz et al. 2010, reported risk of varus and anteversion with the posterior approach (34).
Trochanteric “flip” osteotomy
Advantages
Trochanteric flip osteotomy, proposed by Ganz et al. (38) is an alternative to posterior approach preserving vascular supply, by performing a surgical hip anterior dislocation through the lateral approach, maintaining the posterior capsule intact. This approach does not require gluteal muscles de-insertion from the greater trochanter. In the 213 hips reported by Ganz et al. 2001 with trochanteric flip osteotomy, none had avascular necrosis (38). Beaulé et al. 2004, mentioned how the anterior surgical hip dislocation is the approach to preserve the most biology with a posterolateral trans-trochanteric approach while providing optimal exposure to the acetabulum and proximal femur minimizing the soft tissue dissection (39).
Disadvantages
Early weight bearing and active abduction is limited to allow the osteotomy to heal. There is a risk of trochanteric non-union reported as 7–8% (40), potentially requiring a second surgical intervention to facilitate union or to perform hardware removal if it becomes symptomatic.
Khan et al. (41) compared anterolateral approach and trochanteric flip osteotomy and noticed no difference in the outcome of abductor strength as well as component orientation and fixation. In another series, Beaulé et al. reported a nonunion rate of 8.7% after trochanteric flip osteotomy with 18% patients requiring removal of internal fixation. Hence this approach is reserved for patients undergoing hip preservation surgery with evidence of arthritis that may require an arthroplasty or patients with a high riding trochanter (Figure 3).

Future recommendations
Research and improvement are very dynamic in orthopaedic surgery, the orthopaedic community is continuously searching for new and better equipment and techniques that allow for maximal soft tissue preservation and a fast recovery of the patient, resulting in improved outcomes and satisfaction.
We presented in this review pros and cons of surgical approaches for performing hip resurfacing, there is no one technique without possible risks and complications. However, it is clear that the choice surgical approach can have an impact on clinical outcome. The best surgical technique for hip resurfacing is dependent on patient selection and most importantly is the experience of the orthopaedic surgeon with a good understanding of the anatomy and how to optimize implant positioning to avoid complications.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Hip Resurfacing for the Young Arthritic Hip”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.12.10). The series “Hip Resurfacing for the Young Arthritic Hip” was commissioned by the editorial office without any funding or sponsorship. GG and PEB served as the unpaid Guest Editors of the series and serve as the unpaid editorial board members of Annals of Joint from May 2019 to Apr 2021. PEB reports personal fees from MicroPort, personal fees from MatOrtho, grants and personal fees from Zimmer Biomet, personal fees from Medacta, personal fees from Corin, other from DePuy Johnson & Johnson, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shimmin A, Beaule PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am 2008;90:637-54. [Crossref] [PubMed]
- Beaulé PE, Dorey FJ, Le Duff MJ, et al. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res 2004;87-93. [Crossref] [PubMed]
- Murray DW, Grammatopoulos G, Pandit H, et al. The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg Br 2012;94:1180-6. [Crossref] [PubMed]
- Beaulé PE, Poitras P. Femoral component sizing and positioning in hip resurfacing arthroplasty. Instr Course Lect 2007;56:163-9. [PubMed]
- Marker DR, Seyler TM, Jinnah RH, et al. Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty 2007;22:66-71. [Crossref] [PubMed]
- Amarasekera HW, Costa ML, Foguet P, et al. The blood flow to the femoral head/neck junction during resurfacing arthroplasty: a comparison of two approaches using Laser Doppler flowmetry. J Bone Joint Surg Br 2008;90:442-5. [Crossref] [PubMed]
- Bhargava T, Goytia RN, Jones LC, et al. Lateral femoral cutaneous nerve impairment after direct anterior approach for total hip arthroplasty. Orthopedics 2010;33:472. [PubMed]
- Campbell P, Beaule PE, Ebramzadeh E, et al. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res 2006;35-46. [Crossref] [PubMed]
- Amarasekera HW, Campbell PC, Parsons N, et al. The effect of surgical approach on the histologyof the femoral head following resurfacing of the hip: Analysis of retrieval specimens. Bone Joint Res 2013;2:200-5. [Crossref] [PubMed]
- Stambough JB, Beaule PE, Nunley RM, et al. Contemporary Strategies for Rapid Recovery Total Hip Arthroplasty. Instr Course Lect 2016;65:211-24. [PubMed]
- Steinberg ME. Symposium on Surface Replacement Arthroplasty of the Hip. Summary and conclusions. Orthop Clin North Am 1982;13:895-902. [PubMed]
- Triclot P. Metal-on-metal: history, state of the art (2010). Int Orthop 2011;35:201-6. [Crossref] [PubMed]
- Amstutz HC, Le Duff MJ. Hip resurfacing: a 40-year perspective. HSS J 2012;8:275-82. [Crossref] [PubMed]
- Beaulé PE, Campbell P, Lu Z, et al. Vascularity of the arthritic femoral head and hip resurfacing. J Bone Joint Surg Am 2006;88:85-96. [PubMed]
- Steffen RT, De Smet KA, Murray DW, et al. A modified posterior approach preserves femoral head oxgenation during hip resurfacing. J Arthroplasty 2011;26:404-8. [Crossref] [PubMed]
- Benoit B, Gofton W, Beaule PE. Hueter anterior approach for hip resurfacing: assessment of the learning curve. Orthop Clin North Am 2009;40:357-63. [Crossref] [PubMed]
- Kreuzer S, Leffers K, Kumar S. Direct anterior approach for hip resurfacing: surgical technique and complications. Clin Orthop Relat Res 2011;469:1574-81. [Crossref] [PubMed]
- Judet J, Judet R. The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg Br 1950;166-73. [Crossref] [PubMed]
- Gautier E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 2000;82:679-83. [Crossref] [PubMed]
- Taunton MJ, Mason JB, Odum SM, et al. Direct anterior total hip arthroplasty yields more rapid voluntary cessation of all walking aids: a prospective, randomized clinical trial. J Arthroplasty 2014;29:169-72. [Crossref] [PubMed]
- Zawadsky MW, Paulus MC, Murray PJ, et al. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J Arthroplasty 2014;29:1256-60. [Crossref] [PubMed]
- Yi C, Agudelo JF, Dayton MR, et al. Early complications of anterior supine intermuscular total hip arthroplasty. Orthopedics 2013;36:e276-81. [Crossref] [PubMed]
- Bhandari M, Matta JM, Dodgin D, et al. Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study. Orthop Clin North Am 2009;40:329-42. [Crossref] [PubMed]
- Lachiewicz PF. Metal-on-metal hip resurfacing: a skeptic's view. Clin Orthop Relat Res 2007;86-91. [PubMed]
- van Oldenrijk J, Hoogland PV, Tuijthof GJ, et al. Soft tissue damage after minimally invasive THA. Acta Orthop 2010;81:696-702. [Crossref] [PubMed]
- Goulding K, Beaule PE, Kim PR, et al. Incidence of lateral femoral cutaneous nerve neuropraxia after anterior approach hip arthroplasty. Clin Orthop Relat Res 2010;468:2397-404. [Crossref] [PubMed]
- Khan A, Yates P, Lovering A, et al. The effect of surgical approach on blood flow to the femoral head during resurfacing. J Bone Joint Surg Br 2007;89:21-5. [Crossref] [PubMed]
- Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res 2002;46-53. [Crossref] [PubMed]
- Nork SE, Schar M, Pfander G, et al. Anatomic considerations for the choice of surgical approach for hip resurfacing arthroplasty. Orthop Clin North Am 2005;36:163-70. viii. [Crossref] [PubMed]
- Lavigne P, Loriot de Rouvray TH. The superior gluteal nerve. Anatomical study of its extrapelvic portion and surgical resolution by trans-gluteal approach. Rev Chir Orthop Reparatrice Appar Mot 1994;80:188-95. [PubMed]
- Siebenrock KA, Rosler KM, Gonzalez E, et al. Intraoperative electromyography of the superior gluteal nerve during lateral approach to the hip for arthroplasty: a prospective study of 12 patients. J Arthroplasty 2000;15:867-70. [Crossref] [PubMed]
- Abitbol JJ, Gendron D, Laurin CA, et al. Gluteal nerve damage following total hip arthroplasty. A prospective analysis. J Arthroplasty 1990;5:319-22. [Crossref] [PubMed]
- Ramesh M, O'Byrne JM, McCarthy N, et al. Damage to the superior gluteal nerve after the Hardinge approach to the hip. J Bone Joint Surg Br 1996;78:903-6. [Crossref] [PubMed]
- Kunz M, Rudan JF, Xenoyannis GL, et al. Computer-assisted hip resurfacing using individualized drill templates. J Arthroplasty 2010;25:600-6. [Crossref] [PubMed]
- McBryde CW, Revell MP, Thomas AM, et al. The influence of surgical approach on outcome in Birmingham hip resurfacing. Clin Orthop Relat Res 2008;466:920-6. [Crossref] [PubMed]
- McMinn D, Daniel J, Ziaee H, et al. Posterior surgical approach for hip resurfacing arthroplasty. Techniques in Orthopaedics 2010;25:56-66. [Crossref]
- Costa ML, Achten J, Parsons NR, et al. Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: single centre, parallel group, assessor blinded, randomised controlled trial. BMJ 2012;344:e2147 [Crossref] [PubMed]
- Ganz R, Gill TJ, Gautier E, et al. Surgical dislocation of the adult hip: A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 2001;1119-24. [Crossref] [PubMed]
- Beaule P. A soft tissue-sparing approach to surface arthroplasty of the hip. Oper Tech Ortho 2004;14:75-84. [Crossref]
- Beaulé PE, Shim P, Banga K. Clinical experience of Ganz surgical dislocation approach for metal-on-metal hip resurfacing. J Arthroplasty 2009;24:127-31. [Crossref] [PubMed]
- Khan RM, Cooper G, Hull JB. Hip resurfacing through a modified anterolateral approach, as compared with the Ganz trochanteric flip osteotomy: a two year follow-up study. Hip Int 2009;19:338-42. [Crossref] [PubMed]
Cite this article as: Gomez AM, Grammatopoulos G, Beaulé PE. Contemporary surgical approaches for hip resurfacing. Ann Joint 2020;5:9.



