
Evaluation and treatment of the painful hip resurfacing
The mechanisms of pain and failure of a hip resurfacing arthroplasty (HRA) can be unique when compared to a traditional total hip replacement (THR) because of the different shape and geometry of the implants, as well as the fixation method and retention of proximal femoral bone. The preservation of the proximal femoral head and neck creates an interaction between bone and implant not seen with THR. Additionally, since the femoral bone has been maintained with HRA, this bone can undergo osteonecrosis or deterioration, which would lead to collapse of the femoral implant support. Furthermore, the metal-on-metal (MOM) articulation of HRA can lead to additional problems when compared to the metal-on-polyethylene bearing (MOP) of a THR. Besides the typical infectious or mechanical reasons for a painful arthroplasty, a biological reaction to the metal debris must be considered.
Because of these unique factors, the diagnosis of a painful hip resurfacing and its subsequent management requires considerations that are not typical to other types of revision THA. For example, the measurement of metal ion levels and the use of special imaging techniques to evaluate the periprosthetic soft tissues are helpful. An algorithm to help incorporate these diagnostic modalities is discussed. Revision surgery may be more complicated due to the need to address soft tissue masses or deficiencies that occur because of biologic reactions to the MOM bearing, the so-called adverse local tissue reaction (ALTR). Finally, in the process of revising a MOM HRA, the selection of a bearing articulation that eliminates the chance of future soft tissue reaction is necessary.
Evaluation of the painful MOM HRA
It should be emphasized that with a painful HRA, the reason for failure should not be immediately attributed to the MOM bearing. Specifically, the frequent causes of THR problems must still be analyzed, or the problem will not be resolved. For example, if an infection or loose acetabular component are the source of a painful arthroplasty, then a partial femoral revision to change the bearing surface will fail to correct the problem.
As with any painful arthroplasty, an evaluation for a septic cause should be performed, beginning with inflammatory blood markers. Besides measuring erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), cobalt and chromium blood levels should be obtained. The quantification of metal levels in the blood can help identify failures from accelerated wear (cobalt and chromium levels >7 ppb) as opposed to problems due to metal hypersensitivity (cobalt and chromium levels <7 ppb). Furthermore pre-revision surgery metal levels will be useful as baseline values upon which subsequent measurements can be compared.
A preoperative hip joint fluid aspiration is also advisable in all cases of failed MOM HRA, as this is the best way to rule out infection with cell count and microbiological culture. Intraoperative findings and appearance of a failed MOM articulation may suggest infection due to the creamy and purulent consistency of joint fluid, so it is reassuring to know that the probability of prosthetic joint infection is low prior to revision surgery. Della Valle et al. have highlighted the need to manually segment the different cell population of the joint fluid aspirate, as automated differentials may be falsely elevated due to metal particles and cell clumping (1).
Radiographic evaluation of hip resurfacing implants
Good quality biplanar radiographs are useful for evaluating the position of the implants within the bone, their stability over time, and the presence of bone changes that may indicate an intra-articular process such as impingement or osteolysis. Besides the standard AP X-ray, assessing acetabular component anteversion should be performed with either a cross-table lateral radiograph or cross-sectional images. If it is appropriately positioned, then a surgeon may elect to not revise a well-fixed shell, avoiding bone loss and providing the patient with an easier recovery.
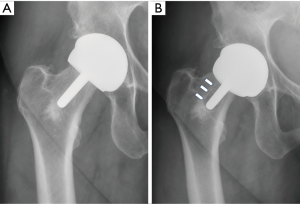
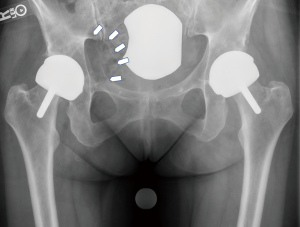
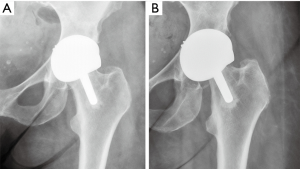
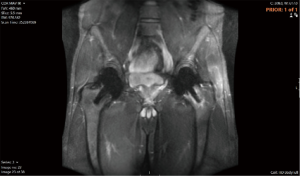
Implant stability can be assessed with the use of serial radiographs and the evaluation of the implant position relative to the bone. The stem of the femoral implant, if not cemented during the original implantation, can act as an “antenna”, providing an early warning sign for femoral migration. Migration is most commonly seen into a more varus position, leading to an asymmetric radiolucency on the lateral aspect (Figure 1A,B). Neck impingement of the native femoral bone upon the implanted acetabular component can be seen superolaterally, particularly in patients with high flexibility in flexion and external rotation (Figure 2). Radiolucencies behind the acetabular component represent osteolysis, which is due to a host reaction to wear debris (Figure 3). Finally, thinning of the femoral neck over time (Figure 4) may also represent a reaction to metal debris because of compression of the bone by hypertrophic synovium.
Soft-tissue imaging
Since the soft tissues around a MOM HRA can be affected by metal debris, an assessment of the integrity of the capsule and abductor muscles is helpful before undertaking revision surgery. Evaluating the soft tissues with advanced imaging can reveal pathology in a problematic MOM HRA that doesn’t have positive radiographic findings. For example, cross-sectional imaging can assess for the presence of cystic or solid masses around the joint, evaluate for osteolytic lesions, or look for bone edema. Magnetic resonance imaging (MRI) should use advanced techniques that incorporate a metal artifact reduction sequence (MARS) so that the soft tissues can be seen with a MOM articulation. At our institution, multiacquisition variable resonance image combination (MAVRIC) MRI is utilized, which uses distinct frequency offsets to acquire multiple overlapping volumes. This leads to less image distortion because of a an improved signal to noise ratio. MAVRIC MRI can more clearly visualize the synovium and periprosthetic bone around MOM articulations, when compared to conventional MRI (2).
As MRI capabilities to visualize MOM THR may not be widely available and can be of variable quality, ultrasound can be useful. An experienced ultrasonographer can detect reactions to metal debris around the hip that manifest as fluid collections or soft-tissue masses. Because of its accessibility, ultrasonography of the hip can be a good screening tool for problems. Garbuz et al. (3) found that ultrasound was 100% sensitive in detecting pseudotumors around MOM THR at their institution.
Metal ion interpretation
Cobalt and chromium metals are the majority elements that comprise the MOM HRA implants, so with articulation at the hip joint, metal particles are created. Thus, the levels of cobalt and chromium in the blood gives insight into the amount of intra-articular material wear. This is especially useful because wear of the articulating surfaces is not measurable on X-ray. Research has shown blood cobalt and chromium levels to highly correlate to their levels in the synovial fluid, and thus they are a surrogate for a direct measurement from the joint (4).
Although it has been questioned whether or not metal ion measurements should be done routinely, it is generally agreed that they provide valuable information in the evaluation of a painful MOM THR (5). While revision surgery is not mandated by a set threshold of cobalt or chromium, a well-functioning MOM HRA typically has metal ion levels in the 1.5–3 parts per billion (ppb) range (6,7).
Unlike cases of taper corrosion in THR where the ratio of cobalt and chromium is elevated above 1 (8), the metal levels in HRA are usually 1:1, since there are no taper junctions.
Non-infectious causes of pain
The non-infectious causes of a painful HRA can be categorized as mechanical or biological.
Mechanical causes
Iliopsoas tendon impingement
As in a traditional THR, impingement of the iliopsoas tendon upon the anterior aspect of the acetabular component can cause groin pain. In particular with the HRA patient population, more strenuous activities may elicit this pain; therefore this younger active population may be predisposed to experiencing groin pain. Bin Nasser et al. found an 18% incidence of groin pain in a cohort of HRA patients and postulated that this may be greater than in conventional THR (9).
To evaluate for the cause of groin pain, a cross-table lateral X-ray is helpful in assessing the position of the acetabular component relative to the anterior acetabular bone (Figure 5). If the X-ray is unrevealing, an MRI may be helpful to look for fluid or tendon inflammation.
A diagnostic injection with lidocaine can also be helpful in confirming the diagnosis. If there is no or minimal protrusion of the acetabular component beyond the anterior acetabular bone, then non-surgical measures such as rest, stretching, active release therapy techniques, anti-inflammatory medication, and cortisone injection have a reasonable chance of success. If there is significant protrusion of the component beyond the native bone, there is a greater potential need for surgery. Chalmers et al. found in a THR population, protrusion <8 mm had success with tenotomy of the iliopsoas tendon, whereas protrusion >8 mm had better success with acetabular revision surgery (10).
Component loosening
Groin pain in HRA can also be caused by a loose acetabular component. Because of the cobalt chrome composition of the implant and the inability to supplement fixation with screws, there is likely a greater possibility of failure of osseointegration of a HRA acetabular component as compared to a THR. As such, patients may experience groin pain, usually in the triphasic pain pattern characteristic of a loose implant. Technetium-99 three phase bone scan is helpful to confirm this diagnosis, demonstrating circumferential tracer uptake in the supra-acetabular region.
A loose femoral component in HRA can also be a cause of weight bearing pain, again in a characteristic triphasic pattern. Because the method of fixation and geometry of the implant is different than a THR, surgeons may not be as familiar in detecting this failure mechanism. Typically this will occur in midterm follow-up, likely from collapse of the supporting bone of the femoral head, and a shift into varus alignment of the femoral implant can be seen on sequential X-rays. Asymmetric radiolucent lines around the femoral stem can suggest a change in position of the implant.
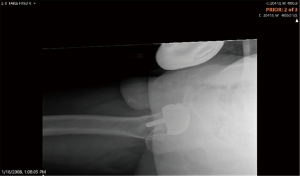
Stress fracture femoral neck
Because of the preservation of the femoral neck in HRA, it exists as a potential area of failure. A femoral neck fracture may be obvious (Figure 6), or occult. In the occult situation, it may only be seen on MRI as bone edema in the femoral neck (Figure 7). Typically this pain would manifest itself in the groin and proximal thigh region with weight bearing activity.
A displaced femoral neck fracture clearly needs surgery, generally to a stemmed femoral implant. An occult femoral neck fracture, similar to a stress fracture, can be treated with a period of non-weightbearing.
Impingement
With the retention of the femoral neck, there can be bone on acetabular implant impingement (Figure 2). This femoral neck to cup impingement may cause some discomfort in certain positions, but did not correlate with elevation in metal ion levels or a higher failure rate (11). In general, although this may be potential cause of pain in HRA, it is rare that revision surgery would be necessary to treat it.
Biologic causes (soft tissue reactions to wear debris)
Accelerated wear
Excessive metallic wear debris from a MOM HRA can lead to painful joint inflammation characterized by synovitis and effusion. Accelerated wear failures are caused by edge-loading at the articulation that may occur because of component malposition, a poorly designed implant articulation, suboptimal metallurgy, patient anatomy, or patient activity. The end result is the excess production of metal debris particles which then cause a macrophage mediated response. The resultant soft tissue abnormality is typically a “thin-walled” pseudotumor which is cystic and fluid filled. The synovium is hyperemic and hypertrophic, and the fluid and soft tissues are often stained with a gray color.
Hypersensitivity
In 2005, Willert et al. described the finding of a host immune reaction to metal debris particles in failed MOM THR (12). When looking at the histology of the tissues, the investigators noted vascular proliferation with a surrounding collection of lymphocytes. There was a significant difference in the histological findings in failed MOM THR vs. those that were well functioning. Willert hypothesized that this histologic response represented a type IV hypersensitivity reaction to the metal debris, termed aseptic lymphocytic vasculitis associated lesion (ALVAL) (13).
In the evaluation of a failed MOM HRA, ALVAL can also lead to pseudotumor formation, more often characterized as a solid mass with tissue necrosis, and osteolytic lesions.
Pseudotumor
Pseudotumor is a term that should be discussed in the context of a failed MOM HRA. It was first introduced by investigators at Oxford University to describe a failure mechanism around MOM hip resurfacings (14). Glyn-Jones et al. found that female patients had a greater incidence of painful swelling around the hip characterized by fluid collections, cystic masses, and solid, soft tissue masses (15). Although the researchers couldn’t determine what caused these “pseudotumors”, looking back these masses were likely a result of both accelerated wear and hypersensitivity reactions. The patients in the series were found to have a large number of acetabular components outside of the safe zone that would have subjected the articulation to edge-loading, though it was not realized at the time. Other patients had acetabular components that were within the generally accepted safe zone of position and still developed pseudotumors, suggesting an immunologic response to metal debris. As metal levels were not measured, the pseudotumor that occurred in this series probably encompassed both accelerated wear and hypersensitivity reactions.
Since at the time of the study, the investigators were not aware of this failure mechanism, the soft tissue growths were allowed to progress to the point where they had compressive effects on neurovascular structures. Because of this, the pseudotumor excisions were extensive and had a high incidence of serious complications; the prognosis was poor in several of these patients (16).
With awareness of this potential problem, more frequent monitoring for soft tissue and bone damage is now performed, leading to improved results with revisions for pseudotumors (17).
Diagnostic algorithm
We use an algorithm (Figure 8) that encompasses the thought processes and evaluation modalities discussed in this paper. Evaluation for infection, component loosening, and iliopsoas tendon impingement in a symptomatic MOM HRA are performed as would be expected and are not mentioned in this algorithm. The diagnostic arms where the patient is has no symptoms and imaging tests are normal (no revision necessary), or where the patient has significant symptoms and there are abnormal radiographic findings (revision necessary), are quite clear as to the management. Scenarios where patients there are abnormal imaging or metal levels but patients are asymptomatic; or where patients are symptomatic and have negative diagnostic findings, are more difficult to manage. In these cases, further diagnostic and more frequent testing are often necessary.
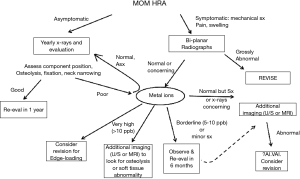
Asymptomatic joint
If the patient has no symptoms and the radiographs show implants with acceptable position, no signs of implant loosening or migration, and maintenance of periprosthetic bone quality, the joint may be evaluated in another year. If the X-rays show bone loss around the femoral neck, or osteolytic lesions, then metal ion measurements and cross-sectional imaging are obtained. If blood metal levels are clearly elevated or imaging reveals soft-tissue reactions, then the patient should enter into a more frequent interval of monitoring, such as every 6 months. This imparts to the patient the gravity of the issue and alerts them to the possibility of a revision operation despite the lack of symptoms. Upon follow-up testing, if there is progressive soft tissue damage on MRI, greater swelling or mass on ultrasound, or further elevation of metal ions, then revision surgery is indicated.
Symptomatic joint
With a symptomatic joint and abnormal X-rays, revision surgery is necessary. If the patient has symptoms but the radiographs are normal, then metal ions are measured. If the blood cobalt or chromium are markedly elevated, then revision is indicated for accelerated wear/edge-loading. If metal ions are normal or only slightly elevated, then cross-sectional imaging is the next step. If advanced imaging shows a soft tissue reaction such as a solid mass, then the likely diagnosis is ALVAL and the joint should be revised. If imaging is normal, then the patient can enter into the 6-month cycle of monitoring; or if he/she insists upon surgery due to symptoms, then this would constitute the “unexplained pain” category of revision etiology. In these situations, the patient should be counseled that the surgery is exploratory in nature and may not correct his/her symptoms.
Reconstructive options
As with any revision surgery, the goal is to correct the problem at hand and to avoid it occurring again in the future. As such, a ceramic on polyethylene (PE) or ceramic on ceramic bearing should be used in order to eliminate the MOM bearing. To reduce the possibility of corrosion at the head/neck taper when revising a failed MOM joint, most surgeons will avoid the use of a cobalt chrome femoral head. Retained metallic debris in the joint leading to third body wear with PE has not been clinically demonstrated. This is likely because metallic debris is smaller and finer than fractured ceramic particles. Nevertheless, because of this theoretical concern, some surgeons choose to revise all failed MOM articulations to ceramic-on-ceramic to avoid runaway PE wear.
With a monoblock HRA acetabular component, there are dual-mobility PE head options that can eliminate the articular production of metal debris. As with any liner exchange, a well-fixed and well-positioned socket is a requirement for its retention. In the specific situation of a loose HRA femoral implant, this can be corrected by using a stemmed femoral implant with a dual-mobility head that matches the size of the existing socket. Though this can be a less invasive solution to a both component revision, the dual-mobility head can lead to other problems such as intra-prosthetic dislocation or even excessive wear. Blevins et al. demonstrated in a series of 71 patients that a both component revision had a higher number of complications than the femoral only revision group; however, the femoral only revision group had two intraprosthetic dislocations with extensive polyethylene wear of the dual mobility head (18).
Debridement of the soft tissues around a failed MOM joint is important. Metallic staining of the synovial tissues and trochanteric bursa is frequently seen in cases of accelerated wear. A complete excision of the involved synovial tissue should be performed in order to rid the joint of metal particles, thus reducing the foreign material inciting a host response. Furthermore, removing this metal laden tissue reduces the particle load from the host, helping the elevated metal levels to return to normal more rapidly.
In hypersensitivity cases, the joint fluid may look purulent because of its cloudy and creamy appearance. Hence, this is one of the reasons we recommend a preoperative joint aspiration for all failed MOM joints; as long as the preop aspiration has ruled out infection, we will proceed with the revision as planned. Hypersensitivity reactions can also result in solid masses with caseous material throughout the joint (Figure 9). Excision of this tissue is critical in order to prevent recurrence of the masses from ongoing reactions.

Histological evaluation of the removed tissue is critically important to evaluate for the likelihood of a hypersensitivity reaction. We routinely use the Campbell ALVAL score at our institution, which examines the tissue for the synovial lining integrity, inflammatory cell infiltrates, and tissue organization; this provides a semi-quantitative measure of the intensity of an immunologic reaction (19).
Results
Revision outcomes after failed MOM HRA have been lacking, with certain series describing a high incidence of complications, subpar clinical scores, and a need for repeat revision surgery (16,20). In our experience, the results following failure of a MOM HRA depend upon the reason for revision, with mechanical failures achieving excellent postoperative clinical scores (21). HRA that failed due to accelerated wear also did well at minimum 2-year follow-up, but patients whose hips failed because of unexplained pain or hypersensitivity reactions had the poorest outcomes.
Revisions of MOM THR using titanium fiber-metal shells have been shown by Munro to have a higher failure rate of acetabular bone ingrowth (4 of 17; 24%) than would be expected. This leads to the possibility that the ingrowth potential of acetabular bone is affected by the metal debris; thus highly-porous acetabular components are recommended for revision operations of failed MOM HRA (20). Grammatopoulos demonstrated a 50% rate of major complications in his series of revision with a 9.4% incidence of re-revision for recurrent soft-tissue masses; as mentioned previously, this may be due to the advanced nature of these lesions prior to treatment (16).
De Smet has shown that results could improve with earlier revision surgery (17). With more frequent monitoring of MOM THA with modalities such as metal levels, clinical examination, and advanced imaging, the author felt that he was able to revise patients earlier and with less soft tissue and bone damage.
Future surveillance
We believe that blood cobalt and chromium should be followed on a yearly basis until they normalize. In addition to interval postoperative radiographs to assess for implant position and stability, cross-sectional imaging is not routinely obtained unless the patient is symptomatic; in these cases, it is helpful for the evaluation of ongoing or persistent soft tissue reactions.
Conclusions
Revision surgery of a failed MOM HRA presents issues that are unique to the metal on metal articulation. Only after evaluation of the painful HRA for reasons common to traditional THR should the MOM bearing be examined as the potential cause. To address problems caused by the wear debris of a MOM HRA, a complete excision of the synovium and soft tissues containing metal particles must be performed. To avoid the future production of metal debris, a ceramic-on-ceramic or ceramic-on-PE bearing should be used. In severe cases, the amount of soft tissue damage and subsequent debridement may lead to instability of the joint; to avoid dislocation of the revision joint, constrained liners, dual mobility implants, or muscle transfers for abductor mechanism deficiency may be necessary. More extensive soft tissue damage around the hip can compromise the results of revision, so earlier intervention for problem MOM HRA is recommended.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (George Grammatopoulos and Paul E. Beaulé) for the series “Hip Resurfacing for the Young Arthritic Hip” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.12.12). The series “Hip Resurfacing for the Young Arthritic Hip” was commissioned by the editorial office without any funding or sponsorship. EPS reports personal fees from Smith and Nephew, personal fees from United Orthopedics, personal fees from Orthalign, personal fees from Kyocera, outside the submitted work. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yi PH, Cross MB, Moric M, et al. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res 2015;473:498-505. [Crossref] [PubMed]
- Hayter CL, Koff MF, Shah P, et al. MRI after arthroplasty: comparison of MAVRIC and conventional fast spin-echo techniques. AJR Am J Roentgenol 2011;197:W405-11 [Crossref] [PubMed]
- Garbuz DS, Hargreaves BA, Duncan CP, et al. The John Charnley Award: Diagnostic accuracy of MRI versus ultrasound for detecting pseudotumors in asymptomatic metal-on-metal THA. Clin Orthop Relat Res 2014;472:417-23. [Crossref] [PubMed]
- De Smet K, De Haan R, Calistri A, et al. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am 2008;90:202-8. [Crossref] [PubMed]
- Kwon YM, Lombardi AV, Jacobs JJ, et al. Risk stratification algorithm for management of patients with metal-on-metal hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons, and the Hip Society. J Bone Joint Surg Am 2014;96:e4 [Crossref] [PubMed]
- Su EP, Housman LR, Masonis JL, et al. Five year results of the first US FDA-approved hip resurfacing device. J Arthroplasty 2014;29:1571-5. [Crossref] [PubMed]
- Daniel J, Ziaee H, Pradhan C, et al. Blood and urine metal ion levels in young and active patients after Birmingham hip resurfacing arthroplasty: four-year results of a prospective longitudinal study. J Bone Joint Surg Br 2007;89:169-73. [Crossref] [PubMed]
- Hothi HS, Berber R, Whittaker RK, et al. The Relationship Between Cobalt/Chromium Ratios and the High Prevalence of Head-Stem Junction Corrosion in Metal-on-Metal Total Hip Arthroplasty. J Arthroplasty 2016;31:1123-7. [Crossref] [PubMed]
- Bin Nasser A, Beaule PE, O'Neill M, et al. Incidence of groin pain after metal-on-metal hip resurfacing. Clin Orthop Relat Res 2010;468:392-9. [Crossref] [PubMed]
- Chalmers BP, Sculco PK, Sierra RJ, et al. Iliopsoas Impingement After Primary Total Hip Arthroplasty: Operative and Nonoperative Treatment Outcomes. J Bone Joint Surg Am 2017;99:557-64. [Crossref] [PubMed]
- Le Duff MJ, Johnson AJ, Wassef AJ, et al. Does femoral neck to cup impingement affect metal ion levels in hip resurfacing? Clin Orthop Relat Res 2014;472:489-96. [Crossref] [PubMed]
- Davies AP, Willert HG, Campbell PA, et al. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am 2005;87:18-27. [Crossref] [PubMed]
- Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am 2005;87:28-36. [Crossref] [PubMed]
- Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008;90:847-51. [Crossref] [PubMed]
- Glyn-Jones S, Pandit H, Kwon YM, et al. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br 2009;91:1566-74. [Crossref] [PubMed]
- Grammatopoulos G, Pandit H, Kwon YM, et al. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br 2009;91:1019-24. [Crossref] [PubMed]
- De Smet KA, Van Der Straeten C, Van Orsouw M, et al. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin North Am 2011;42:259-69. ix. [Crossref] [PubMed]
- Blevins JL, Shen TS, Morgenstern R, et al. Conversion of Hip Resurfacing With Retention of Monoblock Acetabular Shell Using Dual-Mobility Components. J Arthroplasty 2019;34:2037-44. [Crossref] [PubMed]
- Campbell P, Ebramzadeh E, Nelson S, et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010;468:2321-7. [Crossref] [PubMed]
- Munro JT, Masri BA, Duncan CP, et al. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res 2014;472:523-8. [Crossref] [PubMed]
- Su EP, Su SL. Surface replacement conversion: results depend upon reason for revision. Bone Joint J 2013;95-B:88-91. [Crossref] [PubMed]
Cite this article as: Su EP. Evaluation and treatment of the painful hip resurfacing. Ann Joint 2020;5:16.




