
Polyethylene for hip resurfacing—worth a second look
Introduction
Evolution of polyethylene for hip resurfacing
It is easy to equate the concerns with metal-on-metal arthroplasty and the concept of hip resurfacing. Hip resurfacing and metal-on-metal are not synonymous. The polymers polyethylene, polyurethane, polytetrafluoroethylene, polyester, and polyoxymethylene have all been used for implant arthroplasty of the hip. Polyethylene has been used most commonly, because the other polymers did not have the necessary resistance to wear in their early preparations. The large diameter of the articulation necessary for hip resurfacing is an inherently difficult design challenge. It has taken many years to produce thin wear-resistant polyethylene. Loosening, wear, and impingement were all significant failure issues in early cases. The results of hip resurfacing in the 1970s and 1980s were generally poor and hip resurfacing was largely abandoned by the mid-1980s (1-6). The legacy of the early failures was a distrust of the hip resurfacing concept. This was similar to the skepticism about metal-on-metal resurfacing today (7-10).
The failure of early polyethylene resurfacing procedures was a consequence of poor materials, poor implant design, inadequate instrumentation, and imprecise surgical technique. Failure is not inherent with the hip resurfacing procedure itself. The concept of hip resurfacing is sound, as it preserves a more normal transmission of forces across the joint. The retention of bone and avoidance of an intramedullary implant are attractive features. Admittedly, hip resurfacing is much more difficult to perform. Hip resurfacing has not been embraced by most orthopedic surgeons. Hip resurfacing patients are younger and more demanding (11,12).
Preserving the large femoral head makes surgical exposure of the acetabulum difficult. There is a significant exposure advantage in favor of total hip replacement. Typically, there is more deformity present in resurfacing candidates, as they are much more likely to have femoral acetabular impingement and underlying dysplasia because their advanced arthritis occurred at a younger age. The bone preparation during resurfacing is demanding and unforgiving with respect to the fit of the prosthesis to bone. Typically, there is just one implant size appropriate for each patient. The size of the femoral head determines the acetabular implant to be used.
Conventional polyethylene was vulnerable to wear (1,13,14). It was uncertain if efforts to improve polyethylene would be successful, so attention was turned to improving the wear resistance of the femoral component. Cobalt chromium replaced stainless steel. Ceramics either as a fully ceramic femoral component or ceramic-coated titanium came next and were improvements (15). Fully ceramic resurfacing ensembles have been used several times but squeaking and an occasional fracture have been limiting factors. Delta ceramics have been suggested as a solution, but stress shielding has been an issue (16,17). Metal-on-metal has been used widely but adverse reactions to metal wear debris have been the concern (3,18,19).
Improvement of the acetabular bearing was challenging. Initial trials using polyurethane were promising (18,20). The widespread acceptance of polyethylene, however, made it the most attractive candidate material. Five well-accepted assumptions had to be overcome and solved to use polyethylene for hip resurfacing: (I) conventional teaching suggested the minimal polyethylene thickness must be 6 mm (21). Most implants have used much thicker dimensions. Manufacturers, the Food and Drug Administration, and surgeons required relatively thick polyethylene (22); (II) it was assumed that the large capacity of the polyethylene would have unacceptable volumetric wear leading to early failure (23); (III) deformation of the thin polyethylene wear would lead to failure; (IV) impingement would result in pain and ultimate failure given the necessarily larger femoral neck compared to total hip replacement; (V) polyethylene acetabular components must be thicker or larger and, therefore, possibly less bone conserving.
The cross-linking of polyethylene has been a significant advance for all implant arthroplasty procedures. With cross-linked polyethylene, acetabular implants with a capacity of up to 44 mm and greater have been shown to provide the necessary resistance to wear and are available commonly for total hip replacement. Also, cross-linked polyethylene with a thickness of 3.6–4.0 mm has been shown to be safe and implants with this dimension have been in clinical use for many years for both total hip replacement and resurfacing (18,24-26). With cross-linked polyethylene, thicknesses between 4.0 and 5.0 mm are now routine offerings for total hip replacement. However, impingement can be an issue causing failure with highly cross-linked polyethylene. The polyethylene must be fully supported by the metal backing and not extend beyond the rim as it might in some implants (26,27). The necessarily thin polyethylene with its thin metal backing deforms with surgical implantation and this must be managed carefully. Bone preservation is of paramount importance during hip resurfacing surgery.
The first use of highly cross-linked polyethylene for hip resurfacing surgery immediately followed its introduction for total hip replacement in 1998. Custom implants, total hip polyethylene implants repurposed for hip resurfacing, and specific polyethylene resurfacing implants have been used successfully (2,15,27).
Specific design rationale
There are many valleys of death for good ideas. Conventional wisdom required an incremental approach to innovating the acetabular component for hip resurfacing. Metal-on-metal and ceramic-on-ceramic implants are 6 mm thick. The critical dimension is the last reaming of the acetabulum compared to the last reaming of the femoral head; this should be not more than 10 mm (28). An acetabular component using polyethylene of this dimension is possible. There are circumstances in which there is abundant bone available but it is important to preserve at least 5 mm of medial and anterior walls for most patients. Acetabular preparation is of paramount importance in hip resurfacing.
It is possible to safely make acetabular implants with 4 mm of polyethylene, 2 mm of metal backing, and 1 mm of porous coating (29,30) (Figure 1). This ensemble still can have an effective polyethylene liner locking mechanism. If the construct were any thinner it would need to be one piece, as it could not accept a locking mechanism for the polyethylene liner. A two-piece implant allows the use of a central threaded impactor which affords better visualization during insertion. Impactors for one-piece implants can impede visualization and or require a more complex inserter (27). Also, a two-piece implant allows for independent polyethylene exchange and for supplemental screw fixation if necessary.

An important advance has been the understanding of the importance of managing the deformation of thin components. Acetabular component deformation has been a significant reason for component failure when using two-piece acetabular constructs with unforgiving metal or ceramic inserts and, possibly, with thin polyethylene. The metal shell deforms against the acetabular bone prepared by the under-reaming necessary to secure a firm press fit (31). Imperfect fit of the metal or ceramic liner can lead to wear debris generation and failure. Thin polyethylene inserts and thin titanium shells also deform during insertion. Stable liner capture by the locking mechanism is critical to the long-term success of the prosthesis. Also, there have been independent concerns about the potential adverse effect of component osseointegration from strain with shell deformation during insertion. These concerns have been proven to be insignificant and osseointegration occurs reliably with under reaming (31).
With correct insertion tools, shell insertion and intraoperative liner engagement have been proven safe. Long-term studies including retrieval data have shown that thin components are successful (22,24). It is possible to under-ream the acetabular component by 3 mm and still be able to insert and assemble the two-piece prosthesis intraoperatively. With under-reaming, critical acetabular bone is preserved. Because under-reaming is possible, most patients can be treated with the same size polyethylene acetabular component or just a 2-mm incremental increase compared to total hip replacement (26,32) (Figure 2).

Polyethylene wear with liner sizes up to 52.5 mm has been shown to be minimal both in clinical application and in wear simulator studies up to 30 million cycles (18). The wear experienced with hip resurfacing parallels the favorable wear seen with total hip replacement. However, edge loading from impingement is still a concern. The solution has been to use polyethylene fully supported by the acetabular shell (Figure 1). There are two acetabular polyethylene designs that have been used for resurfacing in which the polyethylene liner covers the edge of the metal backing leaving a vulnerability to impingement of the femoral neck against the polyethylene (26,27). The wear of highly cross-linked polyethylene has been studied using wear simulation, clinical retrievals, and by imaging using computed tomographic (CT) scans. All three methods suggest low wear equating to a lifetime of use.
There have been few femoral component failures. Such failures are related to the fundamental health of the femoral head. Femoral components can be cemented yet, more recently, cementless fixation is performed and is an attractive option. The femoral component can be anatomic or flat topped (Figure 3). The author has had good success with a cementless anatomic femoral component. Ceramic-coated implants are attractive from a wear standpoint and they are appealing to patients who have concerns about reactions to implanted metals (33).

Methods
Beginning in 1998, the author has implanted 2,154 highly cross-linked hip resurfacing prostheses in 1,931 patients. Thirty-two patients died and 35 were lost to follow-up. The same inclusion and exclusion criteria were used in this study of polyethylene hip resurfacing as have been used in other studies for metal-on-metal hip resurfacing. It was necessary to have geometry that would allow placement of the acetabular prosthesis with a least 5 mm of medial wall preservation and bone quality that was within the normal range (34,35). The femoral prostheses were cemented in 840 (39%) and uncemented in 1,314 (61%) patients (Figure 3). Follow-up examinations were performed at 8 weeks, 6 months, and annually, and outcomes were assessed using the Modified Harris Hip Score, WOMAC instrument, and UCLA Hip Score (36-38). Follow-up evaluation also included a digital anteroposterior (AP) view radiograph of the pelvis centered over the symphysis (Figure 4), an AP view of the hip centered over the femoral head, and a shoot-through lateral radiograph. High-resolution CT scans with metal-artifact reduction software were performed to look for polyethylene wear in 102 participants when they presented 6–11 years postoperatively (18) (Figure 5).


Wear simulator testing
The author compared the wear of 30 highly cross-linked polyethylene resurfacing implants to conventional polyethylene using a wear simulator for 30 million cycles (18). The highly cross-linked implant had 93% less wear than the conventional polyethylene (P<0.001), which equates to more than 30 years of clinical use by highly active patients.
The materials and methods have been described in greater detail previously (26).
Results
The follow-up period ranged from 5 to 21 years (median, 9.5 years). Patient demographics are shown in Table 1. The postoperative functional results all improved significantly (Table 2). Eighty percent of the patients achieved a postoperative UCLA score of 8 or greater. The average acetabular component inclination was 41° (range 30° to 53°) and the average anteversion was 15° (range, 0° to 25°). The average femoral anteversion was 13° (range, 0° to 20°). All femoral components were neutral or placed in a valgus orientation with respect to the native femur. Screw fixation was used in 9% of patients when the shell was ≥20% uncovered.
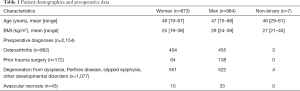
Full table
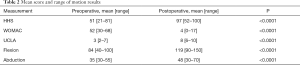
Full table
Complications
There were two dislocations that resolved nonoperatively. Eleven patients continued to report pain (five mild, four moderate, two significant). There were 21 deep infections; three were treated successfully by two-stage reimplantation and conversion to total hip replacement, 12 were treated with systemic antibiotics and implant retention with or without surgical debridement, two underwent a single-staged revision of the resurfacing implant (Figure 6), and four were treated with chronic suppression and implant retention.

Revisions
Twenty-four patients (1%) underwent successful revision of their femoral component to a stem-supported implant from 3 to 20 years following the initial surgery. The causes of failure were femoral neck fracture (12), femoral loosening or subsidence (9), and infection (3). Two patients had a revision of their femoral resurfacing component to another femoral resurfacing component. In all revisions, the metal-backed acetabular component was retained and the acetabular liner was exchanged to allow use of a smaller or the same highly cross-linked polyethylene. There were five acetabular revisions for loosening. A new shell with screw fixation resulted in a secure component and successful outcome. Using revision for any reason as the endpoint, the Kaplan-Meier survival estimate of mean survivorship was 97.5% (95% CI, 95–98.9%) at 10 years (Figure 3). There were no bearing-surface failures or pending revisions.
Retrievals
There were 32 polyethylene implants retrieved during revision surgery or postmortem. The implants were retrieved from 3 to 20 years after placement. Examination found minimal wear ranging from 0.003 to 0.07 mm/year and no visible evidence of damage to the polyethylene.
Bone retention
Figure 5 shows the bone retention and absence of acetabular wear 11 years following an entirely cementless hip resurfacing arthroplasty. The results of bone retention evaluation have been reported previously (32). Briefly, the mean acetabular wall was 10 mm thick postoperatively vs. 15 mm preoperatively, the head: neck ratio was 1.36 postoperatively compared to 1.42 preoperatively. The leg length increased a mean of 4 mm postoperatively. The acetabular component was a mean of 3.9 mm to Kohler’s line and there were no instances of compromise to the femoral neck or medial wall.
Deformation testing
Acetabular under-reaming is a bone preservation and fixation strategy in hip resurfacing. All prior reports of acetabular component deformation have been cadaveric studies (31). I assessed the deformation of the thin shells and very thin highly cross-linked polyethylene in 32 acetabular components retrieved postmortem or during revision after a mean of 9 years of patient use. They had been placed with 3 mm of under-reaming. Deformation of the shells and liners was measured during insertion, 30 minutes after implantation, after reducing the hip and testing range of motion, and at retrieval. The acetabular shells deformed a mean of 0.58 mm on insertion. At retrieval the residual deformation was 0.23 mm. The initial liner deformation was 0.29 mm decreasing to 0.15 mm on retrieval. The calculated insertional force was 367 Nm. There were no acetabular fractures, and no shell or liner failures. The thin resurfacing acetabular shells and liners deform when placed with 3 mm of under-reaming. The deformation becomes less with loading, bone relaxation, and clinical use. There were no adverse clinical consequences from under-reaming and all implants performed well. The bone preservation provided by under-reaming is beneficial during hip resurfacing surgery.
Efficiency of treatment
The author recorded the time of answering questions for patients presenting for hip resurfacing and patients presenting for total hip replacement. The interview time spent with resurfacing patients had an overall mean of 49 minutes compared with 24 minutes for total hip replacement. Themes were identified using qualitative interviews. For resurfacing patients their hip function was integral to their sense of well-being and self-efficacy. Resurfacing patients self-identified as having different needs and higher demands than other patients. Resurfacing patients used medical literature and the internet as first sources of information and physician information as their second source. Care coordinators found additional instruction and trust building was necessary with hip resurfacing patients. The operative time was also longer, with mean of 88 minutes compared with 64 minutes for total hip replacement.
Discussion
Hip resurfacing using highly cross-linked polyethylene is a successful procedure. It is a conceptually attractive solution to hip arthritis for young and active patients. There are four practical considerations that are limiting for hip resurfacing: (I) hip resurfacing is a difficult technical procedure that invites errors. Because of the more difficult exposure, demanding planning and execution, surgeons are more attracted to the more efficient total hip replacement alternative; (II) resurfacing implants are typically more expensive and less available; (III) the procedural coding and payment systems typically do not recognize the additional challenges resurfacing presents, with payment the same as total hip replacement; (IV) hip resurfacing patients are younger, more engaged, and often ask more questions and have higher expectations than older patients and consume more staff and surgeon time. By comparison, total hip replacement represents a more efficient procedure. Also, the weight of opinion and authority recommends hip replacement rather than hip resurfacing. The clinical performance and preference of resurfacing patients, however, leads to a better overall outcome. Because of the ceiling effect of outcome tools, accurately measuring and demonstrating additional value for hip resurfacing has been a challenge.
There are young patients whose needs and expectations will not be met by total hip replacement. The retention of femoral bone, smaller volume of implanted material, and ability to offer the procedure when the medullary canal is blocked are all procedural advantages of hip resurfacing. The functional advantages for resurfacing patients are enhanced stability, ability for sports and other physically demanding endeavors, and a lower incidence of mortality at 10 years compared to hip replacement (39-43). In addition, infection, when it occurs, is more easily managed without intrusion into the femoral canal.
The successful reports about hip resurfacing may seem systematically biased. It is possible to control for bias by: (I) using independent, blinded third-party examiners; (II) using well-designed qualitative questions with sufficient follow-up; (III) recognizing that randomized trials comparing hip resurfacing arthroplasty to total hip replacement in different patients have not shown any influence of patient preoperative preference on either their outcome or postoperative preference (44), and (IV) recognizing that patients do not always correctly recall which procedure they received and, therefore, are not always able to form a bias. The expectations patients have for resurfacing are higher for both function and survivorship than for total hip replacement. Comparison studies have shown a preference for hip resurfacing. Patients with a resurfaced hip on one side and a hip replacement on the other have consistently expressed a strong preference for hip resurfacing arthroplasty (45,46).
The 20-year results of using conventional polyethylene for hip resurfacing with the Indiana Conservative Hip (DePuy, Warsaw, IN), THARIES, TARA and Wagner (Zimmer Biomet, Warsaw, IN) were poor (1,4,5,47). Improved techniques and instrumentation and the use of highly cross-linked polyethylene have resulted in much better outcomes and survivorship. The issues with metal-on-metal and the potential issues of squeaking, fracture, and stress shielding with ceramic-on-ceramic can be avoided. Polyethylene is familiar and well-studied. Improvements in intraoperative technique have included intraoperative imaging, a cannulated system for placing the femoral guide pin, cementless fixation, more effective impactors for the acetabular shell and liner, and possibly computer-assisted surgery. A deeper understanding and better management of acetabular shell deformation have resulted in better fixation and better bone conservation.
Hip resurfacing is successful in conserving acetabular bone compared to total hip replacement (26,29,47,48). Preserving femoral bone is not only advantageous in case of a revision but also functionally. Revision surgery in the uncommon and unwelcome event of failure in this study was successful in producing an outcome equivalent to primary hip replacement.
Earlier concerns with conventional polyethylene relative to wear, thickness, osteolysis, and deformation have been solved with cross-linked polyethylene (26,32,49). The currently available implants are successful but even thinner one-piece implants may be possible. However, one-piece implants require the use of an effective suction, negative pressure or pegged acetabular inserter, which is complicated, and preclude supplemental dome screw fixation and independent liner exchanges. Also, managing the deformation of one-piece components is more challenging. The implants described in this study have been successful enough to continue offering polyethylene hip resurfacing with confidence. These are not custom-made components (27).
There are limitations to this work. All the procedures were performed by a single very experienced surgeon. Thus, it is possible that the results would not be reproducible in other centers. A multicenter study would have been preferred and additional centers are now being added to continue this research. Similar but not identical implants were used. Smaller studies using a consistent implant and technique have been published (26,32). The follow-up in this study was midterm but some results have extended to 21 years.
Townley, Amstutz, and Buechel came close, but did not reach success with conventional polyethylene for hip resurfacing (1,29,50). They each looked at highly cross-linked polyethylene and the present work extends and adds further evidence that highly cross-linked polyethylene is the next step in the evolution of hip resurfacing (15,30,51). Improvements that have led to success using polyethylene for hip resurfacing are: (I) improved operative technique, (II) improved instrumentation, (III) improved management and understanding of acetabular shell and liner deformation, and (IV) additional and longer implant testing and clinical follow-up. Hip resurfacing arthroplasty using highly cross-linked polyethylene is a reliable and durable procedure that meets even the highest demands of younger active patients.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (George Grammatopoulos and Paul E. Beaulé) for the series“Hip Resurfacing for the Young Arthritic Hip” published in Annals of Joint. The article has undergone external peer review.
Conflict of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2019.12.09). The series “Hip Resurfacing for the Young Arthritic Hip” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board approval (# 5190S-11) and the investigation was conducted in conformity with ethical principles of research and that informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pritchett JW. Success rates of the TARA hip. Am J Orthop 1998;27:658. [PubMed]
- Pritchett JW. Curved-stem hip resurfacing: minimum 20-year followup. Clin Orthop Relat Res 2008;466:1177-85. [Crossref] [PubMed]
- Freeman MA. Total surface replacement hip arthroplasty. Clin Orthop Relat Res 1978;2-4. [PubMed]
- Yue EJ, Cabanela ME, Duffy GP, et al. Hip resurfacing arthroplasty: risk factors for failure over 25 years. Clin Orthop Relat Res 2009;467:992-9. [Crossref] [PubMed]
- Costi K, Howie DW, Campbell DG, et al. Long-term survival and reason for revision of Wagner resurfacing hip arthroplasty. J Arthroplasty 2010;25:522-8. [Crossref] [PubMed]
- Malviya A, Lobaz S, Holland J. Mechanism of failure eleven years following a Buechel Pappas hip resurfacing. Acta Orthop Belg 2007;73:791-4. [PubMed]
- de Steiger RN, Miller LN, Prosser GH, et al. Poor outcome of revised resurfacing hip arthroplasty. Acta Orthop 2010;81:72-6. [Crossref] [PubMed]
- Dunbar MJ, Prasad V, Weerts B, et al. Metal-on-metal hip surface replacement: the routine use is not justified. Bone Joint J 2014;96-B:17-21. [Crossref] [PubMed]
- Pritchett JW. Letter to the Editor: Poor survivorship and frequent complications at a median of 10 years after metal-on-metal hip resurfacing revision. Clin Orthop Relat Res 2017;475:1747-8.
- Pritchett JW. One-component revision of failed hip resurfacing from adverse reaction to metal wear debris. J Arthroplasty 2014;29:219-24. [Crossref] [PubMed]
- de Waal Malefijt MC, Huiskes R. A clinical, radiological and biomechanical study of the TARA hip prosthesis. Arch Orthop Trauma Surg 1993;112:220-5. [Crossref] [PubMed]
- Hellman MD, Ford MC, Barrack RL. Is there evidence to support an indication for surface replacement arthroplasty?: a systematic review. Bone Joint J 2019;101-B:32-40. [Crossref] [PubMed]
- Kurtz SM, Gawel HA, Patel JD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res 2011;469:2262-77. [Crossref] [PubMed]
- Mall NA, Nunley RM, Zhu JJ, et al. The incidence of acetabular osteolysis in young patients with conventional versus highly crosslinked polyethylene. Clin Orthop Relat Res 2011;469:372-81. [Crossref] [PubMed]
- Pritchett JW. Conservative total articular replacement arthroplasty: minimum 20-year follow-up. In: McMinn DJW, editor. Modern hip resurfacing. New York: Springer, 2009:408-14.
- Blakeney WG, Beaulieu Y, Puliero B, et al. Excellent results of large-diameter ceramic-on-ceramic bearings in total hip arthroplasty: Is Squeaking Related to Head Size. Bone Joint J 2018;100-B:1434-41. [Crossref] [PubMed]
- Yoon BH, Park IK. Atraumatic fracture of the BIOLOX delta ceramic liner in well-fixed total hip implants. Orthopedics 2018;41:e880-3. [Crossref] [PubMed]
- Pritchett J. Very large diameter polymer acetabular liners show promising wear simulator results. J Long Term Eff Med Implants 2016;26:311-9. [Crossref] [PubMed]
- Cobb JP, Clarke SJ, Jeffers J, et al. Anatomic ceramic hip resurfacing arthroplasty: first in human trials. Orthop Proc 2018;100B:29.
- Pritchett J. Heat generated by hip resurfacing prostheses: in vivo pilot study. J Long Term Eff Med Implants 2011;21:55-62. [Crossref] [PubMed]
- Bartel DL, Bicknell VL, Wright TM. The effect of conformity, thickness, and material on stresses in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg Am 1986;68:1041-51. [Crossref] [PubMed]
- Shen FW, Lu Z, McKellop HA. Wear versus thickness and other features of 5-Mrad crosslinked UHMWPE acetabular liners. Clin Orthop Relat Res 2011;469:395-404. [Crossref] [PubMed]
- Lachiewicz PF, Heckman DS, Soileau ES, et al. Femoral head size and wear of highly cross-linked polyethylene at 5 to 8 years. Clin Orthop Relat Res 2009;467:3290-6. [Crossref] [PubMed]
- Kelly NH, Rajadhyaksha AD, Wright TM, et al. High stress conditions do not increase wear of thin highly crosslinked UHMWPE. Clin Orthop Relat Res 2010;468:418-23. [Crossref] [PubMed]
- Martell JM, Verner JJ, Incavo SJ. Clinical performance of a highly cross-linked polyethylene at two years in total hip arthroplasty: a randomized prospective trial. J Arthroplasty 2003;18:55-9. [Crossref] [PubMed]
- Pritchett JW. Hip resurfacing using highly cross-linked polyethylene: prospective study results at 8.5 years. J Arthroplasty 2016;31:2203-8. [Crossref] [PubMed]
- Treacy RBC, Holland JP, Daniel J, et al. Preliminary report of clinical experience with metal-on-highly- crosslinked- polyethylene hip resurfacing. Bone Joint Res 2019;8:443-50. [Crossref] [PubMed]
- Le Duff MJ, Wang CT, Wisk LE, et al. Benefits of thin-shelled acetabular components for metal-on-metal hip resurfacing arthroplasty. J Orthop Res 2010;28:1665-70. [Crossref] [PubMed]
- Buechel FF. Hip resurfacing revisited. Orthopedics 1996;19:753-6. [PubMed]
- Buechel FF Sr, Pappas MJ. A metal/ultrahigh-molecular-weight polyethylene cementless surface replacement. Semin Arthroplasty 2011;22:66-74. [Crossref]
- Markel D, Day J, Siskey R, et al. Deformation of metal-backed acetabular components and the impact of liner thickness in a cadaveric model. Int Orthop 2011;35:1131-7. [Crossref] [PubMed]
- Pritchett JW. Hip resurfacing with a highly cross-linked polyethylene acetabular liner and a titanium nitride-coated femoral component. Hip Int 2018;28:422-428. [Crossref] [PubMed]
- Pappas MJ, Makris G, Buechel FF. Titanium nitride ceramic film against polyethylene. A 48 million cycle wear test. Clin Orthop Relat Res 1995;64-70. [PubMed]
- Beaulé PE, Antoniades J. Patient selection and surgical technique for surface arthroplasty of the hip. Orthop Clin North Am 2005;36:177-85. [Crossref] [PubMed]
- Schmalzried TP, Silva M, de la Rosa MA, et al. Optimizing patient selection and outcomes with total hip resurfacing. Clin Orthop Relat Res 2005;200-4. [Crossref] [PubMed]
- Amstutz HC, Le Duff MJ, Campbell PA, et al. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am 2010;92:2663-71. [Crossref] [PubMed]
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737-55. [Crossref] [PubMed]
- Ware JE, Kosinski M, Keller SD. How to score the SF-12 physical and mental health summary scales. 3rd ed. Lincoln, RI: Quality Metric Incorporated, 1998.
- Haddad FS, Konan S, Tahmassebi J. A prospective comparative study of cementless total hip arthroplasty and hip resurfacing in patients under the age of 55 years: a ten-year follow-up. Bone Joint J 2015;97-B:617-22. [Crossref] [PubMed]
- Barrack RL, Ruh EL, Berend ME, et al. Do young, active patients perceive advantages after surface replacement compared to cementless total hip arthroplasty? Clin Orthop Relat Res 2013;471:3803-13. [Crossref] [PubMed]
- Costa ML, Achten J, Parsons NR, et al. Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: single centre, parallel group, assessor blinded, randomised controlled trial. BMJ 2012;344:e2147 [Crossref] [PubMed]
- McMinn DJ, Snell KI, Daniel J, et al. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ 2012;344:e3319 [Crossref] [PubMed]
- Kendal AR, Prieto-Alhambra D, Arden NK, et al. Mortality rates at 10 years after metal-on-metal hip resurfacing compared with total hip replacement in England: retrospective cohort analysis of hospital episode statistics. BMJ 2013;347:f6549. [Crossref] [PubMed]
- Bisseling P, Smolders JM, Hol A, et al. No clear influence of preference bias on satisfaction and early functional outcome in resurfacing hip arthroplasty. Acta Orthop 2011;82:161-5. [Crossref] [PubMed]
- Fowble VA, dela Rosa MA, Schmalzried TP. A comparison of total hip resurfacing and total hip arthroplasty–patients and outcomes. Bull NYU Hosp Jt Dis 2009;67:108-12. [PubMed]
- Ortiz-Declet VR, Iacobelli DA, Yuen LC, et al. Birmingham hip resurfacing vs total hip arthroplasty: a matched-pair comparison of clinical outcomes. J Arthroplasty 2017;32:3647-51. [Crossref] [PubMed]
- Loughead JM, Starks I, Chesney D, et al. Removal of acetabular bone in resurfacing arthroplasty of the hip: a comparison with hybrid total hip arthroplasty. J Bone Joint Surg Br 2006;88:31-4. [Crossref] [PubMed]
- Vendittoli PA, Lavigne M, Girard J, et al. A randomised study comparing resection of acetabular bone at resurfacing and total hip replacement. J Bone Joint Surg Br 2006;88:997-1002. [Crossref] [PubMed]
- Pritchett JW. Reply to Dr. Ranawat's letter to the editor. Ann Joint 2016;1:25-26. [Crossref]
- Tan TL, Ebramzadeh E, Campbell PA, et al. Long-term outcome of a metal-on-polyethylene cementless hip resurfacing. J Arthroplasty 2014;29:802-7. [Crossref] [PubMed]
- Amstutz HC, Takamura KM, Ebramzadeh E, et al. Highly cross-linked polyethylene in hip resurfacing arthroplasty: long-term follow-up. Hip Int 2015;25:39-43. [Crossref] [PubMed]
Cite this article as: Pritchett JW. Polyethylene for hip resurfacing—worth a second look. Ann Joint 2020;5:10.


