Charcot midfoot reconstruction—surgical technique based on deformity patterns
Introduction
Midfoot is the most commonly affected region in Charcot neuroarthropathy (CN) of the foot and ankle. This often results in midfoot collapse leading to rocker bottom and forefoot abduction deformity (1). The mainstay of treatment is non-operative management in most patients with offloading in a total contact cast or custom orthotics. However, some with significant midfoot deformity and/or instability, along with the loss of protective sensation, can develop chronic foot ulceration as a result of increased plantar pressures despite adequate offloading (2).
Chronic non-healing midfoot ulcers due to CN that do not respond favourably to the offloading measures or exostectomy, can develop repeat infective episodes leading to deep bone infection (3). These ulcers, especially in a diabetic patient, get inevitably colonised by bacteria that can contribute to deep tissue infection and osteomyelitis. Repeat such infective episodes increase the risk of amputation and subsequent mortality (4). Patients with marked Charcot midfoot deformity with or without instability that cannot be offloaded effectively are vulnerable to develop ulceration and infection, potentially leading to a major amputation. A major amputation in a diabetic patient carries an unacceptably high mortality rate and it is desirable to maintain the ambulatory status by offering reconstruction.
Midfoot deformity correction and reconstruction has recently gained popularity as a limb salvage procedure with more predictable and successful outcomes. Many techniques have been described including fixation with lag screws, plates, intramedullary screws and external fixators, or combinations of these (5-8). Non-union or pseudoarthrosis was considered as an acceptable outcome in such difficult pathologies in the past, but it has now become a recognized concern that non-union in a neuropathic foot can result in recurrence of the foot deformity over time. The optimal outcome following a Charcot midfoot reconstruction is an infection free, normal shaped plantigrade foot that has healthy skin coverage and no abnormal bone prominences and can fit in an appropriate shoe or brace for full weight bearing mobilisation.
Patient selection and workup
Charcot midfoot reconstruction is normally considered on patients with midfoot deformity/instability that had developed ulceration or is at risk of developing an ulcer, despite adequate offloading measures. This procedure is ideally performed during the quiescent stage (Eichenholtz stage 2 or 3) of the disease process. The patients undergoing surgical reconstruction of a deformed Charcot foot due to diabetes often present with significant multiple co-morbidities, including neuropathy, nephropathy, retinopathy, obesity, cardiac and peripheral vascular pathologies (9).
Multidisciplinary care
Perioperatively, these patients require input from a multidisciplinary team that, as a minimum, should include a podiatrist, diabetologist, vascular surgeon, orthopaedic surgeon, wound care specialist and an orthotist (10). The team will also require access to a high-quality musculoskeletal and vascular radiodiagnostic service in addition to infectious diseases and plastic surgery services.
Soft tissue assessment
The skin, tendons and other soft tissues in the foot and ankle are assessed for contractures that might require release during surgery. Contracted Achilles tendon is often encountered in this group of patients. Possible failure of primary closure of the surgical incisions must be assessed and skin coverage primarily with plastic surgery techniques or secondarily must be planned.
Pre-operative imaging
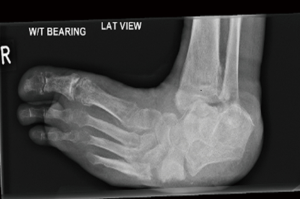
MRI imaging of the foot is valuable in the assessment of the status of soft tissues, presence of deep infection and activity levels of Charcot process. CT imaging of the foot is often needed for surgical planning of osteotomies. Weight bearing plain radiographs of the foot and ankle are extremely helpful for the assessment of mechanical alignment of the foot segments, the degree of bone damage and the deformity. The degree of midfoot deformity is measured by calculating calcaneal pitch, Meary’s angle and dorsoplantar talo-first metatarsal angle (Figure 1A,B).

Midfoot deformity patterns
CN midfoot usually presents with a rocker bottom deformity, most commonly through the tarsometatarsal and/or midtarsal joints. This is often associated with forefoot abduction and pronation. Ulcers develop over the bony prominences, often medially due to the extruded medial cuneiform or laterally the cuboid. The navicular, talar head and base of 5th metatarsal are other areas of bone prominence.
The CN midfoot deformities generally fall into one of these three patterns: (I) rocker bottom forefoot abduction (Figure 2); (II) dorsal subluxation/dislocation (Figure 3); (III) forefoot adduction (Figure 4). The rocker bottom forefoot abduction pattern is the commonest one and results in significant reduction of calcaneal pitch and increase of Meary’s angle and the talar-1st metatarsal angle in the dorso-plantar plane. The Charcot process often affects the Lisfranc, naviculo-cuneiform or talonavicular articulations and result in angulation deformity in these joints with intact bone contact at these articulations. In dorsal subluxation/dislocation pattern the forefoot dissociates from the hindfoot and subluxes or dislocates dorsally causing partial or full loss of normal bone contact at these articulations. This deformity is often due to the involvement of transverse tarsal joints in the Chacot process resulting in tilting of talus plantar wards along with calcaneus due to intact talo-calcaneal articulation, resulting in reduction of calcaneal pitch. The forefoot adduction pattern is uncommon and is usually associated with fracture of the bases of lateral metatarsals and peroneus brevis dysfunction.
Preoperative considerations
Hemoglobin A1c (HbA1c) level is a good indicator of glycaemic control and should be optimised prior to planned surgery. For non-urgent and elective deformity corrections, we aim to achieve an HbA1c level of 8 or less. However, midfoot Charcot deformities in the presence of active infection require emergent surgical procedures and these often present with an HbA1c level above 8. In such situations, we proceed with the first stage of staged correction that involves debridement of infected ulcer and osteomyelitic bone. This, along with optimal microbiological control usually results in better glycemic control so that the second stage of definitive midfoot reconstruction procedure can be performed in a timely manner. Patients with significant peripheral vascular disease should undergo a revascularisation procedure a few weeks prior to the planned reconstruction.
Presence of an ulcer over the bone prominence is not a contraindication for Charcot midfoot reconstruction. It important to diagnose the presence of infection with microbiological cultures from deep tissue or bone specimens. If osteomyelitis is suspected clinically or from cross sectional radiological studies, bone biopsies are performed for microbiological analysis (11). In the presence of active bone infection, a two-stage reconstruction should be considered. During the first stage, the infected ulcers with or without underlying osteomyelitis are surgically debrided and the resultant bone void is packed with an antibiotic loaded calcium sulphate preparation. Excision of large sections of bone often results in instability and the midfoot is temporarily stabilized using three to four 2.5 mm threaded wires or an external fixator if required. Culture-specific parenteral antibiotics are continued until there is clinical and serological evidence of infection eradication. The debridement surgery is repeated if infection eradication is not achieved. The bone biopsies are repeated after stopping the antibiotics for 2 weeks and the definitive midfoot reconstruction is performed if there is continued clinical and serological evidence of infection eradication, along with the absence of microbiological cultures on bone biopsies.
Equipment preference card
Fluoroscopy, handheld Doppler probe, curved osteotomies, oscillating saw, 4 and 6.5 mm cannulated screw system, locking plate system with minimum of 3 mm diameter screw, small and large diameter midfoot column beams.
Procedure
The patient is positioned supine on a radiolucent table with the feet at the edge of the lower end of table. A thigh tourniquet is applied and inflated if there is no contraindication from the leg vasculature point of view. The limb is prepped and draped above the knee in order to leave the patella exposed for assessment of rotational alignment. Fluoroscopy is used throughout the procedure and the machine is ideally placed opposite to the surgeon.
Before inflating the tourniquet, a Doppler probe is used to identify the patent vessels of the ankle and foot, and especially the dorsalis pedis artery and is marked on the skin, from the distal tibia to the foot, with an indelible marker. It is important to know the artery’s exact course, as in severe deformities it varies significantly and often lies very close to the dorsomedial incision.
If an ulcer is present, this is thoroughly debrided at the beginning of the procedure. Bone debridement at the ulcer base is performed to healthy bleeding bone. The instruments used are disposed of and the foot is re-draped. In the presence of a history of previous or recent ulceration or infection multiple bone and soft tissue samples are collected throughout the procedure from previously infected areas for microbiological cultures.
The calcaneal pitch is assessed dynamically under fluoroscopy and if it is not correctable a percutaneous Achilles tendon lengthening is performed by using Hoke’s triple-hemisection technique.
The principle of internal fixation is ‘a durable long-segment rigid internal fixation with optimal bone opposition’. The surgical approaches, osteotomy and fixation construct depend on the patterns of Charcot midfoot deformity.
Rocker bottom abduction pattern
In this pattern, the deformity is predominantly present in the medial column resulting in collapsed medial longitudinal arch and forefoot abduction. This can be corrected by using a plantar and medial based biplanar wedge resection leading to shortening of the medial column and restoration of the medial longitudinal arch.
A dorsomedial curvilinear incision is drawn on the foot at the level of the ankle joint just medial to the tibialis anterior tendon, extended to the distal third of the first metatarsal shaft. The tibialis anterior tendon is retracted laterally and deep dissection is continued through the bed of tibialis anterior to develop thick soft tissue flaps down to the bone. Tibialis anterior tendon is divided near its insertion, leaving a small flap of bone attachment to the base of 1st metatarsal for the tendon reattachment at the end of the procedure. The bony structures are exposed with careful sub-periosteal dissection using a Bristow periosteal elevator and sharp dissection dorsally and plantarly all the way to the lateral column.
A straight or curved biplanar wedge osteotomy, medial and plantar based, with the apex in the body of cuboid, is marked based on the pre-operative planning, and confirmed under fluoroscopy. The wedge osteotomy levels and planes are then marked under fluoroscopy with two 1.6 mm Kirschner wires (Figure 5A). The distal cut of the wedge osteotomy is done through the subchondral bone of the bases of the 1st–3rd metatarsals. Care is taken not to go further distal as this carries the risk of damaging the deep plantar arch and the arcuate artery.

The proximal cut of the wedge osteotomy goes through the cuneiform/navicularis/talar head medially depending on the degree of the deformity and the size of resection. The plantar part of the wedge often includes most of the plantar prominence. The osteotomy cuts are started using an oscillating saw to score the bone and then continued with wide sharp osteotomes. The deeper bone cuts are done using narrower osteotomes under direct vision. This makes sure that the osteotomes stay within the confines of the bone; therefore, the soft tissues are protected. The curved osteotomes are preferable as the shape of the resulting bony surfaces provides better inherent stability and a larger area of bone contact. The senior author prefers to use depth-calibrated curved osteotomes of three different widths for this purpose. The apex of the osteotomy is aimed at the mid-substance of the cuboid bone so that the lateral cortex of cuboid bone is carefully preserved. The deformity is corrected by closing the resected wedge gap through gentle manipulation (Figure 5B). This allows plastic deformation of the lateral cortex of cuboid during correction and the application of tension band plating principle for medial column fixation. Removal of any residual bone is performed in order to achieve optimal bone opposition and ensure absence of bone prominences. This shortening also allows tension free soft tissue closure.
The two 1.6-mm Kirschner wires are then removed and the corrected midfoot position is provisionally held in place with two 2-mm Kirschner wires. The subsequent fixation follows the principles of the superconstruct (12) where the fixation is extended to the next unaffected joint/s in the medial column. It is preferable to extend the fixation to the naviculo-cuneiform joints for simple deformities affecting the tarso-metatarsal articulation only. However, in majority the midtarsal articulation is involved and therefore the superconstruct fixation is extended proximally to beyond the talonavicular joint. All joints included in the superconstruct fixation are prepared with removal of articular cartilage and subchondral bone and using a sagittal saw, osteotome or gouge.
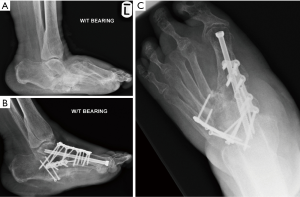
The fixation method depends on the desired stiffness of the construct. It is important to achieve a long-segment and rigid internal fixation in Charcot midfoot deformity corrections (12). Initial reduction and fixation are performed using either one to two 4.0 or 6.5mm cannulated lag screws across the osteotomy or an intramedullary midfoot fusion bolt inserted through the head of 1st metatarsal into the body of talus. The aim of these fixation techniques is to achieve compression across the osteotomy site. The stability of the fixation is then enhanced by plate fixation in neutralisation or buttress mode. A low profile strong and durable plate with a minimum of 3 mm diameter locking screws fixation system is used. The plates are carefully contoured to match the shape of the corrected midfoot. The fixation in most cases needs to extend proximally to the talus and distally to the 1st metatarsal midshaft (Figure 6).
Dorsal subluxation/dislocation pattern
In this pattern, the joint subluxation or displacement often extends to the lateral column and as a result the deformity correction requires bi-column corrective fixation. The medial column surgical approach is performed as described above. The lateral column is approached using a dorsolateral incision from the midshaft of the 4th metatarsal, extended towards the tip of the lateral malleolus by as much as needed. The soft tissue dissection follows the same principles as described above. An osteotomy is done through the fusion mass at the level of previous dislocation/subluxation.
Resection of the overlapped bone ends is done proximally and distally from one or both incisions, to make sure that the dislocation/subluxation is reduced without soft tissue tension. Generous sub-periosteal soft tissue release of the free ends of the osteotomy is normally required in order to plantar translate the distal fragment to be able to restore the medial longitudinal arch and reduce the deformity completely. Exostectomy and reshaping of the bone ends by removing excess dorsal and plantar bone is quite often necessary.
The internal stabilisation of the osteotomy is achieved by using a combination of lag screws, intramedullary midfoot fusion bolts and bi-column plate fixation. Minimum of two 4.0–6.5 mm cannulated lag screws are normally required across the osteotomy to achieve adequate stability. Alternatively, 2–3 intramedullary midfoot fusion bolts are inserted through the head of 1st, 4th and 2nd metatarsals into the tarsal bones. The stability of the fixation is then enhanced by a one locking plate fixation for each column. The medial column plate fixation principles are as described above. The lateral column plate fixation generally spans from the anterior process of calcaneus to the shaft of 4th metatarsal (Figure 7A,B,C).
Forefoot adduction pattern
In this pattern, the forefoot goes into adduction resulting in relative lengthening of the lateral column and some degree of bone loss in the medial column. As a result, this pattern often requires combined lateral and medical column surgical approaches as described above. Laterally based wedge resection followed by bi-column fixation similar to the dorsal subluxation/dislocation pattern is performed.
Careful assessment of the position and length of plates and screws is done under fluoroscopy throughout the procedure to avoid any metal work prominence. In the absence of history of previous infection in the midfoot, autologous bone graft from healthy looking resected bone, proximal tibia or iliac crest is used to fill any residual gaps and promote bone healing. If there was any history of previous bone infection, antibiotic eluting injectable bone graft substitute is used to achieve the same and reduce post-operative infection rates.
The tibialis anterior tendon is reattached in optimal tension. The deep soft tissue layer and skin are closed in a layered fashion over a suction drain if required. The column shortening usually allows for primary wound closure without soft tissue tension. Sterile dressings are used to cover the wound, and a well-padded and moulded below knee 2/3rd backslab is applied.
Post-operative care
Post-operatively the operated leg remains elevated for 48 hours. Post-operative antibiotics are administered according to the preoperative microbiological culture sensitivities when available and changed if necessary based on the intraoperative specimen sensitivity results. The wound inspection is done 2 days post-operatively and the suction drain, if used, is removed. The leg is placed in a bivalved non-weight bearing total contact cast once the foot swelling is reduced. The patient is discharged when safe mobilisation is achieved and adequate home micro-environment is ensured. A total contact cast is applied when there are no wound concerns. A non-weight bearing status is recommended until signs of bony union are confirmed radiologically, usually at three months post operatively. Partial weight bearing in a total contact cast is then initiated under regular radiological monitoring for signs of implant failure or loss of correction. When there is radiological evidence of completed bone union, the patient is allowed to mobilise full weight bearing using, custom made orthotics or normal shoes.
Tips, tricks and pitfalls
During Charcot midfoot reconstruction, the priority is given to achieve a normal looking stable plantigrade foot which often involves restoration of the normal alignment angles in the foot. It is however crucial not to jeopardise foot vascularity and soft tissue integrity in order to achieve absolutely normal radiological angles. The degree of correction that can be reached safely without compromising the vasculature is assessed intraoperatively after bone excision and soft tissue releases.
Careful pre-operative planning on CT imaging and weight bearing foot radiographs is essential to plan the surgical incisions and the wedge bone resection, minimise soft tissue tension at closure and maximise stability of the final fixation construct.
On the lateral simulated weight bearing view of the foot, the calcaneal pitch must be corrected to an extent where the normal foot tripod is restored and there are no weight bearing bony prominences between the calcaneal tuberosity proximally and the metatarsal heads distally.
When tension free skin closure is not possible, a partial wound closure aiming for metalwork coverage could be performed and a negative pressure dressing could be applied.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.02.01). VK reports personal fees from Marquardt, outside the submitted work; AV reports personal fees from Bonesupport, during the conduct of the study.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brodsky JW. Patterns of breakdown in the Charcot tarsus of diabetics and relation to treatment. Foot and Ankle 1986;5:353.
- Armstrong DG, Lavery LA. Elevated peak plantar pressures in patients who have Charcot arthropathy. J Bone Joint Surg Am 1998;80:365-9. [Crossref] [PubMed]
- Robinson AH, Pasapula C, Brodsky JW. Surgical aspects of the diabetic foot. J Bone Joint Surg Br 2009;91:1-7. [Crossref] [PubMed]
- Shaikh N, Vaughan P, Varty K, et al. Outcome of limited forefoot amputation with primary closure in patients with diabetes. Bone Joint J 2013;95-B:1083-7. [Crossref] [PubMed]
- Pinzur MS, Gil J, Belmares J. Treatment of osteomyelitis in charcot foot with single-stage resection of infection, correction of deformity, and maintenance with ring fixation. Foot Ankle Int 2012;33:1069-74. [Crossref] [PubMed]
- Sammarco VJ, Sammarco GJ, Walker EW Jr, et al. Midtarsal arthrodesis in the treatment of Charcot midfoot arthropathy. J Bone Joint Surg Am 2009;91:80-91. [Crossref] [PubMed]
- Richter M, Mittlmeier T, Rammelt S, et al. Intramedullary fixation in severe Charcot osteo-neuroarthropathy with foot deformity results in adequate correction without loss of correction - Results from a multi-centre study. Foot Ankle Surg 2015;21:269-76. [Crossref] [PubMed]
- Butt DA, Hester T, Bilal A, et al. The medial column Synthes Midfoot Fusion Bolt is associated with unacceptable rates of failure in corrective fusion for Charcot deformity: Results from a consecutive case series. Bone Joint J 2015;97-B:809-13. [Crossref] [PubMed]
- Hartig N, Krenn S, Trnka HJ. Surgical treatment of the Charcot foot: long-term results and systematic review. Orthopade 2015;44:14-24. [Crossref] [PubMed]
- Manu CA, Mustafa OG, Bates M, et al. Transformation of the multidisciplinary diabetic foot clinic into a multidisciplinary diabetic foot day unit: results from a service evaluation. Int J Low Extrem Wounds 2014;13:173-9. [Crossref] [PubMed]
- Schaper NC, Van Netten JJ, Apelqvist J, et al. Prevention and management of foot problems in diabetes: A Summary Guidance for Daily Practice 2015, based on the IWGDF guidance documents. Diabetes Res Clin Pract 2017;124:84-92. [Crossref] [PubMed]
- Sammarco VJ. Superconstructs in the treatment of charcot foot deformity: plantar plating, locked plating, and axial screw fixation. Foot Ankle Clin 2009;14:393-407. [Crossref] [PubMed]
Cite this article as: Kavarthapu V, Vris A. Charcot midfoot reconstruction—surgical technique based on deformity patterns. Ann Joint 2020;5:28.