Comparison of a novel ‘modified full length standing hip knee ankle anteroposterior radiograph’ with the standard hindfoot alignment view radiograph for assessment of hindfoot alignment
Introduction
Hindfoot alignment plays an important role in many foot and ankle pathologies (1). Hindfoot malalignment is a recognized cause of persisting foot and ankle disabilities that may result in degenerative joint diseases (2). Moreover, for surgical correction of malalignment, reliable preoperative determination of hindfoot alignment is crucial (3). Recent evidence suggests that hindfoot malalignment could be critical in knee arthroplasties as well (4). Planovalgus foot has been associated with failure of cruciate retaining total knee replacements (TKRs) (5). In addition, hindfoot valgus and varus alignments may behave differently after TKR; with studies by Hara et al. (6), and Takenaka et al. (7), demonstrating that correction of femorotibial alignment after TKR is associated with improvement in hindfoot alignment in patients who have pre-existing hindfoot valgus but not in patients who have pre-existing hindfoot varus. Cho et al. (8) have showed greater hindfoot valgus deformity to be associated with increased pre-operative varus mechanical alignment in patients undergoing TKR. They have also noticed that this hindfoot alignment improves after TKR, possibly due to restoration of normal mechanical axis of the lower limb (8). Finally, it is evident that hindfoot alignment also changes after high or low tibial osteotomies performed for preventing progression of knee or ankle arthritis (9,10). Hence it would suffice to say that, in addition to the relevance for foot and ankle surgeons, hindfoot alignment assessment is likely to become more significant even for lower limb surgeons operating proximal locations as well.
When planning a TKR or osteotomies around the knee conventional method to determine mechanical alignment angles is by obtaining a standing full-length hip-knee-ankle anteroposterior radiograph (abbreviated as ‘HKA radiograph’ from here onwards in this manuscript) (11). The mechanical axis is a line drawn from the center of femoral head to center of ankle joint. However, it can be argued that the weight (mechanical load) of the body is transmitted from the pelvis to the ground, and thus passes through the hindfoot as well. Actually, it makes sense to include the hindfoot alignment in planning a knee replacement and other procedures where mechanical axis is relevant. Hindfoot alignment has an influence on the overall limb alignment after a knee replacement (4) and may also have a bearing on the success or longevity of a knee replacement (5).
For assessing hindfoot alignment in isolation, there are many standardized hindfoot alignment radiographic views reported in literature (e.g., hindfoot alignment view, long axial view etc.) (12-14). However, it is not possible to capture the entire lower limb skeletal anatomy in these radiographic views. We decided to explore ways to modify the standard HKA radiograph and check if we were able to assess hindfoot alignment from the modified HKA radiograph. If such a radiographic view could be established, we would be able to see the entire lower limb mechanical alignment in a single radiograph including the hindfoot alignment, thus reducing the need for additional radiation related to specific hindfoot radiographic views.
Towards this goal, we designed a novel radiographic modification to the standard HKA radiograph that allows assessment of the hindfoot alignment in the same radiograph used for routine pre-operative planning in patients with knee osteoarthritis.
The aim of our study was to measure the accuracy and precision of hindfoot alignment using our modified HKA radiograph in comparison to the standard hindfoot alignment view radiograph (HAV).
Methods
After obtaining ethics committee approval, 48 consecutive eligible patients awaiting TKR at Golden Jubilee National Hospital (GJNH) were selected for this prospective study.
Following selection criteria were used:
Patient inclusion criteria—(I) patients having predominant knee osteoarthritis, (II) able to give informed consent, (III) able to return for follow-up.
Patient exclusion criteria—(I) patients having advanced osteoarthritis in other lower-limb joint(/s), (II) patients with a limb length discrepancy requiring a shoe-raise.
Radiographic views
Each patient had two radiographs preoperatively; one radiograph was the novel HKA radiograph (modified HKA) and the other was the standard HAV (14).
For obtaining the standard HAV, the method described by Cobey et al. (15) and Saltzman et al. (14) was implemented. This essentially involved directing the X-ray beam behind the ankle in a posterior to anterior direction with 20-degree downward tilt to the floor. The X-ray detector/cassette was placed in a similar 20-degree inclination so that the detection film was perpendicular to the direction of the beam.
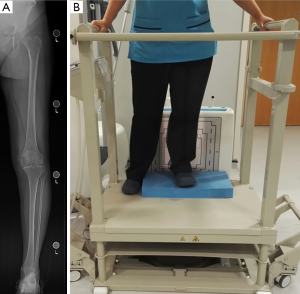
For obtaining hindfoot visualization in an HKA AP radiograph, we first analysed the conventional HKA radiograph and noticed that it usually extended distally until the talus (see Figure 1A,B).
We developed a modified HKA radiograph with the aim to include the entire hindfoot. We achieved this by elevating the platform on which the patient stands. This effectively led to the radiographic view extending further distally to include the calcaneus. In view of the elevated height, hand-bars were designed for health and safety reasons (see Figure 2A,B). For both the radiographs, lower limb and foot position was standardized to avoid excessive internal or external rotation.
Initial trial for feasibility showed that the modified HKA radiograph provided good hindfoot visualization without hindering normal visualization of the entire lower limb from the top acetabulum to the bottom distal leg. Although the extent of hindfoot visualization varied from case to case, the radiographic shadow of medial border of calcaneum was distinctly appreciable in all cases. Hence, we explored to see if we could use this medial border as a landmark to measure tibio-calcaneal angles while comparing the two radiographic views.
Radiographic measurements
Determining the axis of tibia was straightforward in both radiographic views (modified HKA and HAV). We used the method described by Saltzman et al. (14) for determining the tibial axis in both our modified HKA and the standard hindfoot axial views by identifying mid-diaphyseal axis of tibia using two mid-diaphyseal points at 10 and 15 cm above the medial tibial plafond.
Determining a reproducible landmark in the hindfoot was more challenging. This is evident from the disagreements in the various methods described in the literature. When Saltzman et al. originally described the hindfoot axial view, he cautioned that using the mid-axis line of calcaneus can lead to unreliable measurements (14). He instead used a lead strip in each radiograph to define the floor and identified the most inferior point of calcaneus (closest to the lead strip). Perpendicular distance of this point from the tibial axis highlighted the extent of hindfoot varus or valgus deformity (14). This method has been criticized by Reilingh et al. for not being able to provide a quantitative angle that might be more desirable for planning corrective treatment (13). Reilingh et al. instead used 40–60% division as described by Robinson et al. (16) to identify mid-diaphyseal axis of calcaneus. However, in addition to the Saltzman’s pre-existing criticism against using mid-axis, Reilingh et al. also discovered that the relatively short projected height of calcaneus (due to shorter inclination angle of the beam of only 20 degrees) could possibly lead to measurement errors if Robinson method was utilized (13). In fact, Reilingh et al. found measurements in HAV to be less reliable than those obtained at 45-degree inclination angle long axial view (which produces a more elongated image of calcaneus). Finally, Neri et al. have described a line through the most distal point of calcaneus to a point where tangent of talar dome intersects tibial axis to calculate hindfoot alignment in HAV (12).
Since the main goal of our study was to compare the modified HKA with HAV, and because of significant variation in literature on which method to use to calculate alignment in hindfoot, we explored to find an anatomical landmark that was easily visible and not distorted or superimposed in both the views (modified HKA and HAV). After the initial phase comparing various landmarks, we decided to use the radiographic shadow of medial calcaneal border.
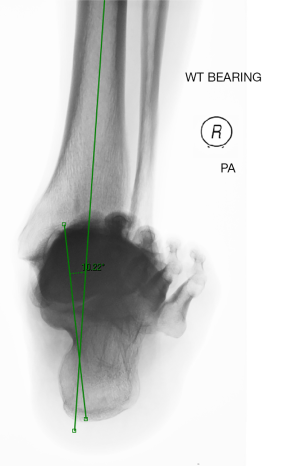
Hindfoot alignment was measured in the standard HAV by first drawing a line along the vertical axis of calcaneus, parallel to the distal medial cortex of calcaneus, and then measuring the angle between this line and the tibial mid-diaphyseal axis (see Figure 3).
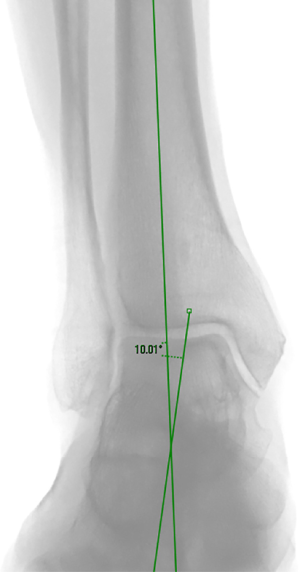
For assessing tibiocalcaneal angle in the modified HKA view, the line through the tibia was the same along the anatomical axis of distal tibial diaphysis. Then the line through calcaneus was drawn along the shadow of medial cortex of calcaneus, and the angle between these two lines was measured (see Figure 4).
Two different experienced orthopedic surgeons measured the two sets of radiographs of each case and calculated the tibiocalcaneal angle. Interobserver variability between both the observers was examined by calculating intraclass correlation coefficient.
Statistical analysis
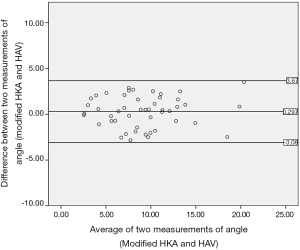
The alignment angle measured on the modified HKA radiograph was compared with the angle measured on the HAV radiograph using Bland Altman plots and limits of agreement. Based on conventional value of three degrees being used in most studies on knee arthroplasty mechanical axis alignment, it was decided that the limits of agreement were be within three degrees for the Modified HKA to provide an acceptable measure of hindfoot alignment.
Results
Tibiocalcaneal angles in modified HKA and HAV radiographs of all 48 cases were independently measured by both observers. Intraclass correlation coefficient between two observers was 0.94 for the tibiocalcaneal angle measurement in the modified HKA radiographs and 0.87 for the same angle in HAV radiographs. Scores between 0.75 to 1 is normally considered to be excellent agreement.
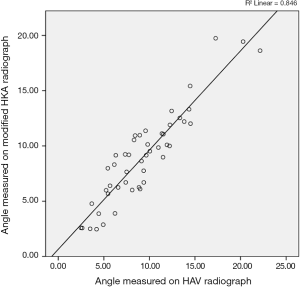
For further calculations and comparisons, average of the measurements obtained by the two observers for each angle was utilized. Then angle measurements of both views were compared using Related Sample Wilcoxon Signed Rank Test and there was no significant difference between the two measurements (P=0.207). On plotting the two values in X and Y axis, a good correlation was observed with Spearman’s Rho coefficient 0.892 (see Figure 5).
Bland Altman plot (see Figure 6) showed most values within 3-degree agreement and all values within +3.67 to −3.08 degrees, suggesting reasonable clinical agreement between the two methods. The mean difference between the angle measured between the new modified HKA and standard HAV was only 0.297 degrees with a standard deviation of 1.69 degrees.
Discussion
We started this study to explore a simple question—can we modify HKA radiograph to include a reasonable assessment of hindfoot in it? As highlighted in detail in the introduction section of this manuscript, this question was driven by multiple recent evidences of hindfoot alignment either being affected or causing problems in surgical procedures proximal to the ankle joint (5-8). In view of these evidences, we argue that there is a need for taking hindfoot alignment in to consideration while assessing hip-knee-ankle mechanical axis in view of these new developments. While foot and ankle surgeons currently have many standardized radiographic methods to assess hindfoot in isolation, there is no method to be used by hip and knee surgeons to analyze simultaneously the entire limb and the hindfoot in the same and unique pre-operative X-rays planning. Developing a method to assess hindfoot alignment from the HKA Radiographs may offer two major benefits. First, it would allow calculation and assessment of hindfoot alignment in patients undergoing TKR without the need for any special or additional radiographic views. Second, this could be potentially help in devising a mechanical alignment of lower limb as a whole in future; which would summate hindfoot alignment to the ‘conventional mechanical axis’ extending from the hip center to center of ankle mortise. There are also evidences exploring role of hindfoot alignment in the lower limb degenerative arthropathies and arthroplasty scenarios (2,6). It was therefore worthwhile to have a method in place, to accurately assess and measure hindfoot alignment in a routine HKA radiograph.
In our modified HKA radiograph view, we have showed that it was possible to obtain weight-bearing hip-knee-ankle views including hindfoot, without sacrificing any loss in hip visualization. We have also demonstrated that the angles measured by the modified HKA radiographs view were in good correlation and reasonable clinical agreement of 3 degrees with the established standard hindfoot alignment views.
However, there are few limitations in our study. First, rotations of foot and lower limb may affect measurement of angle accurately. We have tried to standardize the method by ensuring anatomical landmarks (e.g., patella facing forward) being identical for all cases. However, there is always a potential for error, although this is not unique to our method, and this remains inherent even in the standard HKA radiographs (17-19). Second, we have excluded patients with limb-length discrepancies, and with multiple joint arthritis, from our study. Therefore, we are unable to predict how the angles will behave in such patients. Finally, our method to use a line parallel to medial border of calcaneus, although justified by us in the methods section of this manuscript, is not yet standardized by other studies in the literature.
In view of these limitations listed above, we will not extrapolate our findings to currently advocate our modified HKA radiograph as a replacement to pre-existing standardized hindfoot radiographic views for complex foot and ankle pathologies until further validation from peers. Nevertheless, we are confident in recommending our modified HKA radiograph instead of the conventional HKA radiograph view for pre-operative alignment assessment in patients undergoing lower-limb arthroplasty or osteotomies around the knee. We think this will provide significant information regarding hindfoot to lower limb orthopedic surgeons with no apparent loss to their standard pre-operative planning.
There are many unanswered questions about relationship between varus/valgus in hindfoot with varus/valgus in knee, and how these alignments change before and after arthroplasty. We think this is going to be a field of active research in future and the modified HKA radiograph view described in our study may help in identifying mechanical axis and angles of lower limb as a whole including hindfoot as well.
Conclusions
The new modified HKA radiograph is a reasonable alternative to the hindfoot alignment view for assessment of tibiocalcaneal angle and hindfoot alignment. This allows us to measure hindfoot alignment without needing additional radiographs in patients who would otherwise need two separate radiographs—one for hindfoot and another for lower limb. As the entire femur and tibia is accessible in the same radiograph, there is no loss in ease of pre-operative planning for lower limb arthroplasty/alignment procedures, and a potential gain in creating a dataset for further research in to the mechanical axis of the entire lower limb including the hindfoot alignment component.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Vinod K. Panchbhavi and Maninder Shah Singh) for the series “Foot & Ankle Surgery” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj.2020.01.05). The series “Foot & Ankle Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by West of Scotland Research Ethics Committee 5. The ethics committee reference number is 15/WS/0267. Informed consent was taken from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang C, Xu X, Hu M, et al. Optimization of hindfoot alignment radiography. Acta Radiol 2017;58:719-25. [Crossref] [PubMed]
- Hayashi K, Tanaka Y, Kumai T, et al. Correlation of compensatory alignment of the subtalar joint to the progression of primary osteoarthritis of the ankle. Foot Ankle Int 2008;29:400-6. [Crossref] [PubMed]
- Takakura Y, Takaoka T, Tanaka Y, et al. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am 1998;80:213-8. [Crossref] [PubMed]
- Mullaji A, Shetty GM. Persistent hindfoot valgus causes lateral deviation of weightbearing axis after total knee arthroplasty. Clin Orthop Relat Res 2011;469:1154-60. [Crossref] [PubMed]
- Meding JB, Keating EM, Ritter MA, et al. The planovalgus foot: a harbinger of failure of posterior cruciate-retaining total knee replacement. J Bone Joint Surg Am. 2005;87:59-62. [PubMed]
- Hara Y, Ikoma K, Arai Y, et al. Alteration of hindfoot alignment after total knee arthroplasty using a novel hindfoot alignment view. J Arthroplasty 2015;30:126-9. [Crossref] [PubMed]
- Takenaka T, Ikoma K, Ohashi S, et al. Hindfoot alignment at one year after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2016;24:2442-6. [Crossref] [PubMed]
- Cho WS, Cho HS, Byun SE. Changes in hindfoot alignment after total knee arthroplasty in knee osteoarthritic patients with varus deformity. Knee Surg Sports Traumatol Arthrosc 2017;25:3596-604. [Crossref] [PubMed]
- Choi JY, Song SJ, Kim SJ, et al. Changes in Hindfoot Alignment After High or Low Tibial Osteotomy. Foot Ankle Int 2018;39:1097-105. [Crossref] [PubMed]
- Shah SM, Roberts J, Picard F. Ankle and Hindfoot Symptoms after Medial Open Wedge High Tibial Osteotomy. J Knee Surg 2019;32:269-73. [Crossref] [PubMed]
- Babazadeh S, Dowsey MM, Bingham RJ, et al. The long leg radiograph is a reliable method of assessing alignment when compared to computer-assisted navigation and computer tomography. Knee 2013;20:242-9. [Crossref] [PubMed]
- Neri T, Barthelemy R, Tourné Y. Radiologic analysis of hindfoot alignment: Comparison of Méary, long axial, and hindfoot alignment views. Orthop Traumatol Surg Res 2017;103:1211-6. [Crossref] [PubMed]
- Reilingh ML, Beimers L, Tuijthof GJ, et al. Measuring hindfoot alignment radiographically: the long axial view is more reliable than the hindfoot alignment view. Skeletal Radiol 2010;39:1103-8. [Crossref] [PubMed]
- Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int 1995;16:572-6. [Crossref] [PubMed]
- Cobey JC. Posterior roentgenogram of the foot. Clin Orthop Relat Res 1976;202-7. [PubMed]
- Robinson I, Dyson R, Halson-Brown S. Reliability of clinical and radiographic measurement or rearfoot alignment in a patient population. The Foot 2001;11:238-48. [Crossref]
- Hunt MA, Fowler PJ, Birmingham TB, et al. Foot rotational effects on radiographic measures of lower limb alignment. Can J Surg 2006;49:401-6. [PubMed]
- Kawakami H, Sugano N, Yonenobu K, et al. Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Orthop Res 2004;22:1248-53. [Crossref] [PubMed]
- Jamali AA, Meehan JP, Moroski NM, et al. Do small changes in rotation affect measurements of lower extremity limb alignment? J Orthop Surg Res 2017;12:77. [Crossref] [PubMed]
Cite this article as: Dash KK, Gilchrist J, Picard F, Shah K. Comparison of a novel ‘modified full length standing hip knee ankle anteroposterior radiograph’ with the standard hindfoot alignment view radiograph for assessment of hindfoot alignment. Ann Joint 2020;5:36.