
Rotator cuff tears in elderly patients: is repair worthwhile?
Introduction
Rotator cuff tears (RCTs) are a common cause of pain and shoulder dysfunction (1,2). With increasing age, the prevalence of RCTs also increases (3,4). In those aged 80 years and older, as many as 62% of patients have been noted to have rotator cuff (RC) abnormalities (3). This is particularly important when considering the rate of aging in the global population (5). Between 2015 and 2030, the number of people aged 60 and older is predicted to grow by 56%, from 901 million to 1.4 billion; by 2050 this number is projected to double (2.1 billion) (5). Meanwhile, adult participation in recreational activities, including sports, has increased (6). In the last decade, the understanding of RC pathology in this group of patients has improved. Advances in diagnosis, patient selection, perioperative management, and surgical techniques have led to more sophisticated treatment strategies, negating the dogma of strict nonoperative management in elderly patients with RCTs.
Epidemiology
RC injury is the most common cause of shoulder disability (1), and is associated with pain and decreased function (2). As age increases, the prevalence of RCTs also increases, and the development of RC pathology is considered a normal consequence of aging (3,4,7). Studies have shown that over half of patients (62%) aged 80 years and older may have RC abnormalities (3). Additionally, the pattern of RC injury changes noticeably with age. In older individuals RCTs are usually atraumatic, resulting from chronic degeneration (8). Furthermore, older patients possess a higher likelihood of suffering larger, irreparable RCTs (9).
RC injuries are defined anatomically and present along a spectrum, ranging in severity from tendinopathy, to partial tear, to complete tear (10). The progression of pathology is thought to occur relatively slowly and can oftentimes occur without associated symptoms. Older patients with asymptomatic partial and full thickness tears, may frequently progress to symptomatic tears without trauma; these are accompanied by muscle atrophy and fatty infiltration (7). Yamaguchi et al. reported that patients older than 66 years with a painful RCT in one shoulder have a 50% chance of having a contralateral tear even without noticeable symptoms (4). Asymptomatic tears may be expected to become painful in roughly 30–40% of patients within 2 to 5 years (11-14).
Older individuals are predisposed to a variety of risk factors that complicate RC disease, including age-related conditions such as lower bone density, decreased vascularity, and more complicated medical comorbidities such as diabetes mellitus, rheumatoid arthritis, and renal disease (15,16).
Classification
Multiple classification schemes have been proposed for RCTs. Current classification systems are generally divided into three groups: partial-thickness tears, full-thickness tears, and massive tears. Each group contains subclassifications which are pertinent to the particular tear type, generally involving size, shape, and muscular atrophy.
Partial-thickness tears
Partial-thickness rotator cuff tears (PTRCTs) are most commonly classified by the RC tendons involved, tear location, and by the thickness of the tear. In the Ellman classification system (17) the tear is first identified by location: A. articular-surface, B. bursal-surface, or C. interstitial. The tear is then graded according to its depth: (I) <3 mm (<25% thickness); (II) 3–6 mm (25–50% thickness); and (III) >6 mm (>50% thickness). This grading system assumes the RC footprint to be approximately 10–12 mm in the medial to lateral dimension. However, this classification system does not take into account several factors such as the length of the tear (anterior to posterior size of tear along the tendon footprint), tissue quality of the tendon, or the etiology of the tear (traumatic or degenerative). Compounding upon these limitations, the MOON group has demonstrated poor interobserver reliability in predicting the tear grade on MRI, and only moderate interobserver reliability in predicting the location of the tear (articular or bursal-sided) (18). Regardless of these shortcomings, the Ellman classification system continues to be the most universally utilized system for PTRCTs. Treatment recommendations are based upon the understanding of the histopathology of the tendon, and the depth of the tear. As the depth of the tear increases, there is increased strain on the remaining tendon (19), which may propagate development of a full-thickness tear. Also, the articular side of the tendon has only half of the strength of the bursal side, and accordingly, bursal sided tears are treated more aggressively. Articular sided tears over 6 mm are recommended to be repaired (20), while the threshold to repair bursal sided tears is >3 mm (21).
Full-thickness tears
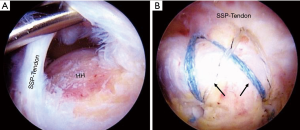
Classification schemes have been developed to describe full-thickness rotator cuff tears (FTRCTs), which have attempted to include tendons involved, tear size, tear shape, chronicity, and muscle atrophy (Figure 1). Perhaps the most recognized system was described by DeOrio and Cofield (22). This system classifies FTRCTs according to tear size: less than 1 cm is small, 1–3 cm is medium, 3 to 5 cm is large, and >5 cm is defined as a massive tear. However, as this is one-dimensional, the system may not properly predict a repairable vs. non-repairable tear (23,24).
The classification system by Harryman et al. (25) incorporated the number of tendons torn: stage 0 is an intact RC, stage IA is a PTRCT of supraspinatus, stage IB is a FTRCT of supraspinatus only, stage II is a FTRCT of supraspinatus involving infraspinatus, stage III involves supraspinatus, infraspinatus, and subscapularis, and stage IV is RCT arthropathy.
Similarly, the Collin et al. classification scheme (26) defines five types of massive RCTs according to tendon involvement: type A are tears of the supraspinatus and superior subscapularis; type B are tears of the supraspinatus and entire subscapularis; type C are tears of the supraspinatus, superior subscapularis, and infraspinatus; type D are tears of the supraspinatus and infraspinatus; and type E are tears of the supraspinatus, infraspinatus, and teres minor. This subclassification of massive tears offers a prediction of pseudoparalysis, or loss of function including forward elevation, external and internal rotation.
Davidson and Burkhart (23) proposed a geometric system of classification which links tear pattern on MRI to treatment and prognosis (24). Type 1 Crescent tears have a medial to lateral depth that is less than or equal to the anterior-posterior width of the tear, or a length under two centimeters, and can usually be repaired with good to excellent results by fixing the tendon directly to bone. Type 2 Longitudinal (L or U) shaped tears have a greater medial to lateral depth than anterior to posterior width, and a tear width under 2 cm; these tears typically are repairable with side-to-side (margin convergence) stitches followed by repair of tendon to bone, resulting in good to excellent outcomes. Type 3 Massive tears are defined by tear length and width greater than 2 cm each; in the majority of these cases interval slides and partial repairs are necessary, with only fair to good results. Finally, Type 4 Cuff tear arthropathy is defined by arthrosis of the glenohumeral joint and decrease of the acromiohumeral distance; these tears are irreparable, and the treatment of choice is arthroplasty.
Massive tears
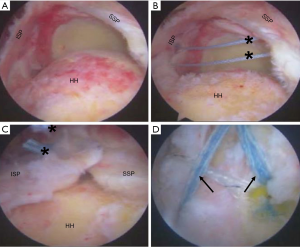
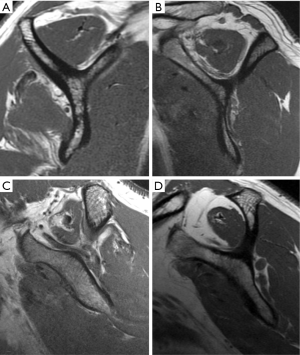
Chronic massive RCTs are associated with tendon contraction and muscle belly atrophy, which increase the difficulty of reconstruction and are associated with poorer outcomes after repair (27) (Figure 2). Goutallier et al. (28) first described the pattern of fatty infiltration on CT scans. In this system, Stage 0 defines normal muscle without fatty streaking, stage 1 demonstrates some fatty streaks, stage 2 demonstrates significant fatty infiltration (but still more muscle than fat), stage 3 represents equal fat and muscle, and in stage 4 a greater amount of fat is present than muscle (Figure 3). Stage 3 and 4 are regarded by some to be indicators of an irreparable tear, although Burkhart et al. demonstrated significant functional improvement in repair of massive RCTs with grade 3 atrophy or higher (27).
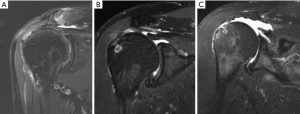
Patte developed a system of tear classification (29), which incorporates tear size, coronal and sagittal plane tear imaging, tendon quality, and biceps tendon involvement; the amount of tendon retraction is the most commonly utilized portion of this scheme to evaluate massive tears (Figure 4). In the Patte classification of tendon retraction, a stage 1 tear remains close to the bony insertion, a stage 2 tear is retracted to the level of the humeral head, and a stage 3 tear is retracted to the level of the glenoid. However, this does not provide a treatment or prognosis for tendon repair, unlike the Davidson and Burkhart scheme (23).
Nonoperative treatment
Nonoperative treatment has been shown to be effective in RCTs of the elderly (30). Treatment may consist of complimentary conservative therapies, including ice and anti-inflammatory drugs, physical therapy (PT), and/or corticosteroid and orthobiologic injections. The goals of treating RCTs in the elderly patient are to decrease pain, improve shoulder function, and improve shoulder biomechanics.
In a recent meta-analysis of randomized controlled trials comparing surgical repair to conservative treatment or subacromial decompression (SAD) for degenerative tears of the RC, Schemitsch et al. (31) concluded that at one year, surgical repair resulted in significantly higher Constant-Murley scores, versus conservative treatment alone or SAD in elderly patients. However, the authors offer a caveat that this difference may be small, and that due to the high success rate of conservative treatment in elderly patients, surgeons may be judicious in recommending surgery or conservative management.
In a prospective study of 68 patients, Agout et al. (32) reported significant functional gains in patients treated conservatively with massive RCTs. Gains plateaued at six months, after which time the authors recommended consideration of surgical treatment.
PT
Moosmayer et al. (33) performed a randomized controlled trial comparing PT to surgical repair for small- to medium-sized tears. Treatment benefits were shown to be greater in the surgical group; however, over 80% in the PT group were satisfied with conservative management at one-year follow-up, and the remaining patients who crossed over to surgical management were effectively treated with delayed surgical repair. The MOON group demonstrated that approximately 75% of patients treated with PT had effective symptom alleviation at two-year follow-up (34).
Corticosteroid injections
Corticosteroid injections provide symptom relief by inhibiting the inflammatory cascade in the injured tendons, relieving pain and stiffness associated with RCTs (35). However, results have been mixed and concerns exist regarding steroid effects on tear propagation, tendon strength and degeneration, resultant infection, and poorer outcomes with subsequent need for revision after ultimate surgical intervention (36).
In a 2003 Cochrane review, Buchbinder et al. (37) reported only small benefit for corticosteroid treatment over placebo in the treatment of RC disease, questioning the efficacy of corticosteroid treatment. Similarly, a recent meta-analysis performed by Mohamadi et al. (38), comparing corticosteroid to placebo treatment for RC tendinosis, found only a minimal and transient decrease in pain in those treated with corticosteroids. Accordingly, the authors did not recommend this treatment due to potential deleterious side effects of corticosteroids on the RC.
Orthobiologics
Platelet-rich plasma (PRP) injections have proven to be an effective modality in treatment of RC tendinosis and PTRCTs (39-41). However, these studies comprise mostly younger patients below the age of 65 years. In regard to more severe RCTs, a meta-analysis of level I and II evidence investigated the use of PRP in patients undergoing arthroscopic repair of FTRCTs and demonstrated no overall benefit on clinical outcomes and re-tear rates (42). However, the authors did not elaborate on the age of included patients. A randomized controlled trial performed by Zumstein et al. (43) reported on a cohort of 35 elderly patients with a mean age of 65.3 years (range, 54–74 years) who underwent arthroscopic repair of FCRCTs. The authors found no beneficial effect of platelet- and leucozyte-rich fibrin on clinical outcome, healing rate, postoperative defect size and tendon quality at 12 months follow-up (43). Nevertheless, there remains a paucity of literature specifically investigating the use of PRP in older patients.
Operative treatment
Operative treatment is generally performed for symptomatic RCTs in younger patients, as tear progression can be expected in over 80% of patients with symptomatic full-thickness tears and over 25% of patients with symptomatic partial-thickness tears (44,45).
In patients aged 65 years or older, the benefit of operative treatment has been historically debated. Comorbidities correlated with age such as diabetes, osteoporosis and cardiovascular disease can influence the fixation strength of RCR; these factors and the inherent compromised healing capability of the tendon has influenced surgeons towards nonoperative treatment (15,16,46). Additionally, high re-tear rates over 50% have been observed following fixation of RCTs in patients older than 70 years (47-49). With the advent of reverse total shoulder arthroplasty (RTSA), surgeons have debated whether joint replacement is superior to other reconstructive approaches in this group of patients (2). However, in recent years, the paradigm has shifted towards a more liberal approach to rotator cuff repair (RCR) in the elderly, as the literature shows promising results when these patients are properly indicated (2,49,50). Furthermore, Dornan et al. (51) compared three treatment strategies [(I) arthroscopic RCR with the option to arthroscopically revise once; (II) arthroscopic RCR with conversion to RTSA on potential failure; (III) primary RTSA] for patients with massive RCTs with pseudoparalysis and without osteoarthritis using a Markov decision model. The authors found that initial arthroscopic RCR for massive RCTs and conversion to RTSA on potential failure was the most cost-effective strategy for treatment in patients with pseudoparalysis and without osteoarthritis. These findings were independent of patient age.
SAD
Some authors have suggested performing a simple SAD for the treatment of RCTs in low-demand elderly patients, arguing that this procedure is less invasive (52). However, when comparing the results of simple SAD to arthroscopic RCR in patients older than 60 years, the repair group achieved better functional outcomes, and eccentric humeral head position and cuff tear arthropathy were avoided in the medium term (53). This is in concordance with the prospective, randomized study performed by Flurin et al. (54). Both the SAD group and the arthroscopic RCR group demonstrated improvements in ASES and Constant scores; however, the RCR group scored significantly better than decompression alone. Palliative SAD is a feasible minimally invasive technique leading to postoperative improvements. Nonetheless, in the authors’ opinion, this should be reserved for older, low-demand patients (54), those who have massive RCTs with high-grade fatty infiltration that seem unlikely to heal following fixation (54), those who do not desire RTSA, and patients who should not undergo a longer procedure due to medical conditions.
Repair
Historically, when repair was chosen for treatment, RCTs were managed with an open approach. With this technique, treatment of massive RCTs in patients older than 70 years of age yielded satisfactory outcomes according to the UCLA score (mean: 30.9 points) in 78.2% of patients in a study published in 1999 (55). Over the last 20 years however, understanding of RC pathology, as well as surgical techniques, has evolved greatly.
In 2005, Rebuzzi et al. (56) were among the first to demonstrate satisfactory results of arthroscopic RCR (mean UCLA score: 30.5 points) in patients older than 60 years of age, regardless of tear size, patient’s age, and type of suture repair. Interestingly, no differences in outcomes were observed when adjusting for preoperative tear size. These early results of arthroscopic repair were similar to those of open repair.
Djahangiri et al. (57) reported on five-year outcomes in patients older than 65 years after mini-open or arthroscopic operations. The authors found that a single tendon RCR resulted in high patient satisfaction and significant improvements of the Constant score. Furthermore, complete healing as determined by ultrasonography was documented in 70% of cases, and those who did heal had significantly better scores. The authors concluded, that mini-open and arthroscopic RCR had similar outcomes in patients older than 65 years when compared with their younger counterparts.
Verma et al. (58) arthroscopically treated 44 patients aged 70 years or older with FTRCTs (Figure 1) and showed significant improvement in pain and function at a mean follow-up of 36.1 months, with an ASES score of 87.5 points. None of the patients required revision surgery. The majority (94.3%) of their patients were satisfied with the results, and 94.1% would commit to doing the procedure again.
Interestingly, Fehringer et al. (59) demonstrated that similar outcome scores were achieved in surgically treated patients aged 65 and older with FTRCTs, compared to untreated patients with intact RCs, if the repairs healed. Additionally, patients with RCRs that healed had better function compared to patients with untreated tears. The healing rate as determined by ultrasonography was 78.5%, which is in line with the findings of other authors for this age group (48,49,57).
Bhatia et al. (60) conducted a study investigating the outcomes of 49 shoulders in 44 recreational athletes who were older than 70 years (mean age 73; range, 70–82 years). At a minimum follow-up of two years, the authors reported good outcomes following arthroscopic RCR in this active patient group of older individuals. Significant improvements in all outcome scores from pre- to postoperatively were demonstrated and no RCRs were revised. Furthermore, median patient satisfaction was 10 out of 10 and 77% of the patients were able to return to their sport at a similar level.
In a systematic review evaluating the treatment options for older individuals with RCTs tears published in 2012, the authors found insufficient evidence to suggest efficacy of operative over nonoperative treatment (61). However, their results showed possible favorable outcomes for repairs.
Most recently, a systematic review by Altintas et al. (2) demonstrated that RCR in patients 70 years or older resulted in high clinical success with good outcomes and pain relief. The authors emphasized that although the re-tear rate in this collective is high (27.1%), RCR offers a joint-preserving method with significant improvements in outcomes if patients are indicated for treatment appropriately, taking into account tear-specific (tear size, tear retraction, fatty atrophy of the RC muscles) and patient-specific characteristics (comorbidities, activity level, osteoarthritis, osteoporosis).
Patch augmentation
Various biologic and non-biologic augmentations exist, aiming to provide stability and improve healing capabilities of large and massive RCTs. In a recent systematic review and meta-analysis, graft augmentation provided significantly lower re-tear rates and higher ASES scores when compared to RCR alone (62). However, this may not be generalizable to the elderly, as the mean age of patients included in this study ranged from 48 to 67.3 years.
Flury et al. (63) investigated tendon integrity and shoulder function in patients aged 60 years and older following RCR of supraspinatus tears, with and without the use of a porcine dermis patch augmentation. No differences in outcome scores and re-tears were seen between the groups. Although results in younger patients have been promising, there is a paucity of literature specifically investigating the use of patch augmentation in the elderly.
Predictors of success
It is commonly believed that inferior outcomes following RCR are correlated with advanced age. However, current investigations have shown that chronological age alone might not be as important as previously thought.
Rhee et al. (47) reported that the re-tear rate following RCR increased significantly with preoperative tear size, but not with increasing age. In their study, no difference in re-tear rates was seen between patients younger and older than 70 years. Charousset et al. (64) reported that age alone was not correlated with poor results; however, the size of the lesion was. They postulated that successful repairs can be achieved, particularly when the tear is limited to the supraspinatus tendon. In a more recent study, Gwark et al. (49) again corroborated that the most significant factor for re-tears was preoperative tear size rather than age.
One factor that might have led to the belief that age is an independent risk factor for failure is the circumstance that older patients possess a higher chance of having larger, irreparable RCTs (9). Additionally, age-dependent comorbidities such as osteoporosis have been identified as independent risk factors compromising RC healing (15). Although Ryu et al. (65) did not find a relationship between vitamin D levels and repair integrity or functional outcomes following RCR, an increased risk for postoperative surgical complications following arthroscopic RCR was observed by Harada et al. (66) Treatment of osteoporosis and vitamin D repletion prior to RCR is an emerging topic of interest; however, literature is scarce (66). Intraoperatively, osteoporotic bone may be managed with the use of larger anchors, broader sutures, medialization of the footprint to reduce tension, and increased points of fixation (16).
Postoperative rehabilitation
Postoperative rehabilitation is essential to successful outcomes after RCR. The goals of the postoperative period are to minimize pain, restore range of motion (ROM), and regain previous levels of functionality.
Superior tendon-to-bone healing has been associated with early immobilization during the immediate postoperative period (67). However, this comes with trade-offs; functional recovery may be delayed by suspending early motion, due to increased stiffness and muscle atrophy (68).
Houck et al. (69) performed a systematic review of seven meta-analyses comparing early passive motion, motion beginning within one week postoperatively, and delayed motion after immobilization for a minimum of 4–6 weeks. No clear conclusion was established in regard to superiority; however, many of the studies supported an increase in ROM and higher re-tear rates with early motion, as well as better healing with delayed motion. Additionally, many studies concluded that tear size played an important factor in protocol determination and success. Thomson et al. (70) conducted a systematic review that investigated the effects of early postoperative ROM exercise compared with delayed rehabilitation protocols. Two of the six studies included in the study reported that patients treated with early motion regained ROM more quickly; however, no statistically significant differences were noted between groups at one year postoperatively. The remaining four studies reported no statistically significant difference between rehab groups, suggesting that early rehabilitation following RCR surgery may not be detrimental.
Strong scientific evidence supporting a definitive postoperative rehabilitation protocol has yet to be established; therefore, the authors recommend a comprehensive approach that considers patient goals, surgical findings, tissue quality, tear size, and post-surgery risks, including stiffness and re-tear rate. Care must be taken to avoid over-stressing the repair during the post-operative window; thus, the authors prefer to immobilize the shoulder in a sling for 6 weeks, beginning with early pendulum and passive ROM exercises immediately postoperatively. At 4 to 6 weeks, active-assisted motion is begun with progression to full active motion as pain permits. Strengthening usually commences between 8 to 10 weeks, with a return to full activity without restrictions between 3 and 4 months.
Conclusions
In summary, healthy elderly patients without significant comorbidities who have the desire to return to an active lifestyle benefit equally from RCR as their younger counterparts. Chronological age does not seem to be an independent risk factor for failure; however, comorbidities associated with age may be. Therefore, patient selection is a crucial component dictating successful outcomes following RCR in the elderly.
Acknowledgments
Research performed at the Steadman Philippon Research Institute, Vail, CO, USA.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adnan Saithna) for the series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (http://dx.doi.org/10.21037/aoj-20-41). The series “Current and Emerging Concepts in the Management of Rotator Cuff Tears” was commissioned by the editorial office without any funding or sponsorship. PCN reports personal fees from Arthrex, outside the submitted work. The position of PCN at the Steadman Philippon Research Institute is supported by Arthrex. PJM reports grants, personal fees and other from Arthrex, Inc., other from Smith & Nephew, other from Siemens, other from Össur, personal fees from Medibridge, personal fees from Springer Publishing, other from VuMedi, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Moosmayer S, Smith HJ, Tariq R, et al. Prevalence and characteristics of asymptomatic tears of the rotator cuff: an ultrasonographic and clinical study. J Bone Joint Surg Br 2009;91:196-200. [Crossref] [PubMed]
- Altintas B, Anderson NL, Pitta R, et al. Repair of Rotator Cuff Tears in the Elderly: Does It Make Sense? A Systematic Review. Am J Sports Med 2020;48:744-53. [Crossref] [PubMed]
- Teunis T, Lubberts B, Reilly BT, et al. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 2014;23:1913-21. [Crossref] [PubMed]
- Yamaguchi K, Ditsios K, Middleton WD, et al. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am 2006;88:1699-704. [Crossref] [PubMed]
- Division UNDoEaSAP. World Population Ageing 2015 2015.
- Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247-57. [Crossref] [PubMed]
- Lazarides AL, Alentorn-Geli E, Choi JH, et al. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg 2015;24:1834-43. [Crossref] [PubMed]
- Yamaguchi K, Tetro AM, Blam O, et al. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg 2001;10:199-203. [Crossref] [PubMed]
- Shim SB, Jeong JY, Kim JS, et al. Evaluation of risk factors for irreparable rotator cuff tear in patients older than age 70 including evaluation of radiologic factors of the shoulder. J Shoulder Elbow Surg 2018;27:1932-8. [Crossref] [PubMed]
- Kuhn JE. Current concepts: rotator cuff pathology in athletes--a source of pain or adaptive pathology? Curr Sports Med Rep 2013;12:311-5. [Crossref] [PubMed]
- Moosmayer S, Tariq R, Stiris M, et al. The natural history of asymptomatic rotator cuff tears: a three-year follow-up of fifty cases. J Bone Joint Surg Am 2013;95:1249-55. [Crossref] [PubMed]
- Maman E, Harris C, White L, et al. Outcome of nonoperative treatment of symptomatic rotator cuff tears monitored by magnetic resonance imaging. J Bone Joint Surg Am 2009;91:1898-906. [Crossref] [PubMed]
- Safran O, Schroeder J, Bloom R, et al. Natural history of nonoperatively treated symptomatic rotator cuff tears in patients 60 years old or younger. Am J Sports Med 2011;39:710-4. [Crossref] [PubMed]
- Keener JD, Galatz LM, Teefey SA, et al. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am 2015;97:89-98. [Crossref] [PubMed]
- Chung SW, Oh JH, Gong HS, et al. Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 2011;39:2099-107. [Crossref] [PubMed]
- Entezari V, Lazarus M. Surgical Considerations in Managing Osteoporosis, Osteopenia, and Vitamin D Deficiency During Arthroscopic Rotator Cuff Repair. Orthop Clin North Am 2019;50:233-43. [Crossref] [PubMed]
- Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res 1990;64-74. [Crossref] [PubMed]
- Spencer EE Jr, Dunn WR, Wright RW, et al. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med 2008;36:99-103. [Crossref] [PubMed]
- Mazzocca AD, Rincon LM, O'Connor RW, et al. Intra-articular partial-thickness rotator cuff tears: analysis of injured and repaired strain behavior. Am J Sports Med 2008;36:110-6. [Crossref] [PubMed]
- Weber SC. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy 1999;15:126-31. [Crossref] [PubMed]
- Cordasco FA, Backer M, Craig EV, et al. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am J Sports Med 2002;30:257-60. [Crossref] [PubMed]
- DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am 1984;66:563-7. [Crossref] [PubMed]
- Davidson J, Burkhart SS. The geometric classification of rotator cuff tears: a system linking tear pattern to treatment and prognosis. Arthroscopy 2010;26:417-24. [Crossref] [PubMed]
- Millett PJ, Warth RJ. Posterosuperior rotator cuff tears: classification, pattern recognition, and treatment. J Am Acad Orthop Surg 2014;22:521-34. [Crossref] [PubMed]
- Harryman DT 2nd, Mack LA, Wang KY, et al. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 1991;73:982-9. [Crossref] [PubMed]
- Collin P, Matsumura N, Ladermann A, et al. Relationship between massive chronic rotator cuff tear pattern and loss of active shoulder range of motion. J Shoulder Elbow Surg 2014;23:1195-202. [Crossref] [PubMed]
- Burkhart SS, Barth JR, Richards DP, et al. Arthroscopic repair of massive rotator cuff tears with stage 3 and 4 fatty degeneration. Arthroscopy 2007;23:347-54. [Crossref] [PubMed]
- Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994;78-83. [PubMed]
- Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990;81-6. [PubMed]
- Lin JC, Weintraub N, Aragaki DR. Nonsurgical treatment for rotator cuff injury in the elderly. J Am Med Dir Assoc 2008;9:626-32. [Crossref] [PubMed]
- Schemitsch C, Chahal J, Vicente M, et al. Surgical repair versus conservative treatment and subacromial decompression for the treatment of rotator cuff tears: a meta-analysis of randomized trials. Bone Joint J 2019;101-B:1100-6. [Crossref] [PubMed]
- Agout C, Berhouet J, Spiry C, et al. Functional outcomes after non-operative treatment of irreparable massive rotator cuff tears: Prospective multicenter study in 68 patients. Orthop Traumatol Surg Res 2018;104:S189-92. [Crossref] [PubMed]
- Moosmayer S, Lund G, Seljom U, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: A randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br 2010;92:83-91. [Crossref] [PubMed]
- Kuhn JE, Dunn WR, Sanders R, et al. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg 2013;22:1371-9. [Crossref] [PubMed]
- Gialanella B, Bertolinelli M. Corticosteroids injection in rotator cuff tears in elderly patient: pain outcome prediction. Geriatr Gerontol Int 2013;13:993-1001. [Crossref] [PubMed]
- Lubowitz JH, Brand JC, Rossi MJ. Preoperative Shoulder Corticosteroid Injection Is Associated With Revision After Primary Rotator Cuff Repair. Arthroscopy 2019;35:693-4. [Crossref] [PubMed]
- Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003;CD004016 [PubMed]
- Mohamadi A, Chan JJ, Claessen FM, et al. Corticosteroid Injections Give Small and Transient Pain Relief in Rotator Cuff Tendinosis: A Meta-analysis. Clin Orthop Relat Res 2017;475:232-43. [Crossref] [PubMed]
- Scarpone M, Rabago D, Snell E, et al. Effectiveness of Platelet-rich Plasma Injection for Rotator Cuff Tendinopathy: A Prospective Open-label Study. Glob Adv Health Med 2013;2:26-31. [Crossref] [PubMed]
- Shams A, El-Sayed M, Gamal O, et al. Subacromial injection of autologous platelet-rich plasma versus corticosteroid for the treatment of symptomatic partial rotator cuff tears. Eur J Orthop Surg Traumatol 2016;26:837-42. [Crossref] [PubMed]
- von Wehren L, Blanke F, Todorov A, et al. The effect of subacromial injections of autologous conditioned plasma versus cortisone for the treatment of symptomatic partial rotator cuff tears. Knee Surg Sports Traumatol Arthrosc 2016;24:3787-92. [Crossref] [PubMed]
- Zhang Q, Ge H, Zhou J, et al. Are platelet-rich products necessary during the arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. PLoS One 2013;8:e69731 [Crossref] [PubMed]
- Zumstein MA, Rumian A, Thelu CE, et al. SECEC Research Grant 2008 II: Use of platelet- and leucocyte-rich fibrin (L-PRF) does not affect late rotator cuff tendon healing: a prospective randomized controlled study. J Shoulder Elbow Surg 2016;25:2-11. [Crossref] [PubMed]
- Yamamoto N, Mineta M, Kawakami J, et al. Risk Factors for Tear Progression in Symptomatic Rotator Cuff Tears: A Prospective Study of 174 Shoulders. Am J Sports Med 2017;45:2524-31. [Crossref] [PubMed]
- Kim YS, Kim SE, Bae SH, et al. Tear progression of symptomatic full-thickness and partial-thickness rotator cuff tears as measured by repeated MRI. Knee Surg Sports Traumatol Arthrosc 2017;25:2073-80. [Crossref] [PubMed]
- Brewer BJ. Aging of the rotator cuff. Am J Sports Med 1979;7:102-10. [Crossref] [PubMed]
- Rhee YG, Cho NS, Yoo JH. Clinical outcome and repair integrity after rotator cuff repair in patients older than 70 years versus patients younger than 70 years. Arthroscopy 2014;30:546-54. [Crossref] [PubMed]
- Robinson PM, Wilson J, Dalal S, et al. Rotator cuff repair in patients over 70 years of age: early outcomes and risk factors associated with re-tear. Bone Joint J 2013;95-B:199-205. [Crossref] [PubMed]
- Gwark JY, Sung CM, Na JB, et al. Outcomes of Arthroscopic Rotator Cuff Repair in Patients Who Are 70 Years of Age or Older Versus Under 70 Years of Age: A Sex- and Tear Size-Matched Case-Control Study. Arthroscopy 2018;34:2045-53. [Crossref] [PubMed]
- Witney-Lagen C, Mazis G, Bruguera J, et al. Do elderly patients gain as much benefit from arthroscopic rotator cuff repair as their younger peers? J Shoulder Elbow Surg 2019;28:1056-65. [Crossref] [PubMed]
- Dornan GJ, Katthagen JC, Tahal DS, et al. Cost-Effectiveness of Arthroscopic Rotator Cuff Repair Versus Reverse Total Shoulder Arthroplasty for the Treatment of Massive Rotator Cuff Tears in Patients With Pseudoparalysis and Nonarthritic Shoulders. Arthroscopy 2017;33:716-25. [Crossref] [PubMed]
- Kempf JF, Gleyze P, Bonnomet F, et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy 1999;15:56-66. [Crossref] [PubMed]
- Jacquot A, Dezaly C, Goetzmann T, et al. Is rotator cuff repair appropriate in patients older than 60 years of age? prospective, randomised trial in 103 patients with a mean four-year follow-up. Orthop Traumatol Surg Res 2014;100:S333-8. [Crossref] [PubMed]
- Flurin PH, Hardy P, Abadie P, et al. Rotator cuff tears after 70 years of age: a prospective, randomized, comparative study between decompression and arthroscopic repair in 154 patients. Orthop Traumatol Surg Res 2013;99:S371-8. [Crossref] [PubMed]
- Worland RL, Arredondo J, Angles F, et al. Repair of massive rotator cuff tears in patients older than 70 years. J Shoulder Elbow Surg 1999;8:26-30. [Crossref] [PubMed]
- Rebuzzi E, Coletti N, Schiavetti S, et al. Arthroscopic rotator cuff repair in patients older than 60 years. Arthroscopy 2005;21:48-54. [Crossref] [PubMed]
- Djahangiri A, Cozzolino A, Zanetti M, et al. Outcome of single-tendon rotator cuff repair in patients aged older than 65 years. J Shoulder Elbow Surg 2013;22:45-51. [Crossref] [PubMed]
- Verma NN, Bhatia S, Baker CL 3rd, et al. Outcomes of arthroscopic rotator cuff repair in patients aged 70 years or older. Arthroscopy 2010;26:1273-80. [Crossref] [PubMed]
- Fehringer EV, Sun J, Cotton J, et al. Healed cuff repairs impart normal shoulder scores in those 65 years of age and older. Clin Orthop Relat Res 2010;468:1521-5. [Crossref] [PubMed]
- Bhatia S, Greenspoon JA, Horan MP, et al. Two-Year Outcomes After Arthroscopic Rotator Cuff Repair in Recreational Athletes Older Than 70 Years. Am J Sports Med 2015;43:1737-42. [Crossref] [PubMed]
- Downie BK, Miller BS. Treatment of rotator cuff tears in older individuals: a systematic review. J Shoulder Elbow Surg 2012;21:1255-61. [Crossref] [PubMed]
- Bailey JR, Kim C, Alentorn-Geli E, et al. Rotator Cuff Matrix Augmentation and Interposition: A Systematic Review and Meta-analysis. Am J Sports Med 2019;47:1496-506. [Crossref] [PubMed]
- Flury M, Rickenbacher D, Jung C, et al. Porcine Dermis Patch Augmentation of Supraspinatus Tendon Repairs: A Pilot Study Assessing Tendon Integrity and Shoulder Function 2 Years After Arthroscopic Repair in Patients Aged 60 Years or Older. Arthroscopy 2018;34:24-37. [Crossref] [PubMed]
- Charousset C, Bellaiche L, Kalra K, et al. Arthroscopic repair of full-thickness rotator cuff tears: is there tendon healing in patients aged 65 years or older? Arthroscopy 2010;26:302-9. [Crossref] [PubMed]
- Ryu KJ, Kim BH, Lee Y, et al. Low Serum Vitamin D Is Not Correlated With the Severity of a Rotator Cuff Tear or Retear After Arthroscopic Repair. Am J Sports Med 2015;43:1743-50. [Crossref] [PubMed]
- Harada GK, Arshi A, Fretes N, et al. Preoperative Vitamin D Deficiency Is Associated With Higher Postoperative Complications in Arthroscopic Rotator Cuff Repair. J Am Acad Orthop Surg Glob Res Rev 2019;3:e075 [Crossref] [PubMed]
- Zhang S, Li H, Tao H, et al. Delayed early passive motion is harmless to shoulder rotator cuff healing in a rabbit model. Am J Sports Med 2013;41:1885-92. [Crossref] [PubMed]
- Keener JD. Revision rotator cuff repair. Clin Sports Med 2012;31:713-25. [Crossref] [PubMed]
- Houck DA, Kraeutler MJ, Schuette HB, et al. Early Versus Delayed Motion After Rotator Cuff Repair: A Systematic Review of Overlapping Meta-analyses. Am J Sports Med 2017;45:2911-5. [Crossref] [PubMed]
- Thomson S, Jukes C, Lewis J. Rehabilitation following surgical repair of the rotator cuff: a systematic review. Physiotherapy 2016;102:20-8. [Crossref] [PubMed]
Cite this article as: Nolte PC, Seiter M, Elrick BP, Millett PJ. Rotator cuff tears in elderly patients: is repair worthwhile? Ann Joint 2021;6:20.


