
Concept of neutral rotation sling for non-operative treatment of proximal humerus fractures
Introduction
Proximal humerus fractures (PHFs) are a common source of morbidity in patients, especially in the elderly population. It is the third most common fracture diagnosed in elderly patients after hip and distal forearm fractures (1). PHFs most commonly occur from a low energy mechanism such as a fall from standing height. These fractures are more common in females (84%) and elderly patients with an average age of 71 years (2). While extremely common, up to 84% of PHFs are treated conservatively without surgery (3). The proportion of PHF being treated conservatively has remained relatively unchanged in the past decade. In that same timeframe, open reduction and internal fixation (ORIF) was the most common type of surgery for PHFs. Shoulder replacement procedures are another surgical option, with recent emphasis on reverse shoulder arthroplasty (RSA), which has largely replaced hemiarthroplasty (HA) (4).
Surgery has traditionally been reserved for displaced two, three, and four-part PHFs based on the classic Neer criteria (5). Although the rate at which PHFs are being treated with surgery has not changed, there has been recent literature supporting non-operative treatment in displaced PHFs. The Proximal Fracture of the Humerus Evaluation by Randomization (PROFHER) study was a multi-center randomized study conducted in the United Kingdom comparing surgical and non-surgical treatment in 250 patients with displaced surgical neck fractures of the proximal humerus. The study found no difference in function outcomes, quality of life scores, complication rates, or mortality at two and five years post-injury (6,7). Furthermore, two recent Cochrane systematic review showed no evidence of improved functional or quality of life scores in operatively treated displaced PHFs (8,9).
A uniform protocol for suggested non-operative treatment of PHFs does not currently exist. A wide range of timeframes for immobilization exist. The duration, frequency, and type of physical therapy also varies significantly in the literature. When assessing the type of immobilization used, most commonly it is a routine sling with the arm resting in an internally rotated position. The potential exists for malreduction of the PHF from remaining in this position. In this article, we introduce the concept of immobilization of PHFs in neutral rotation. Furthermore, we offer a comprehensive review of non-operative protocols used in the literature, and propose a standardized protocol for non-operative treatment of these injuries.
Neutral rotation immobilization
The method of shoulder immobilization in PHFs may influence fracture healing and ultimately shoulder function. Few studies have compared different types of shoulder immobilizers. Rommens et al. compared the Gilchrist arm sling to a Desault bandage, finding better patient satisfaction with the Gilchrist arm sling but no difference in functional results (10). Both forms of immobilization hold the arm in internal rotation and neither is widely used in practice today. The standard of care in many medical centers is immobilization in a commercially available simple sling. While this is a cost-effective option for shoulder immobilization, standard slings typically hold the arm in an internally rotated position.
No studies to date have directly compared outcomes in PHF treated nonoperatively in a neutral rotation sling versus a standard internal rotation sling. However, a recent randomized controlled trial found that neutral rotation slings provided improved external rotation, adduction, and pain after anatomic total shoulder arthroplasty (11). Similarly, improved motion and pain has been shown in patients with rotator cuff repairs treated with neutral rotation braces (11). While it is unrealistic to extrapolate these results to nonoperatively treated PHFs, literature has shown that immobilization of a post-insult shoulder in neutral rotation many times leads to earlier improved motion and pain.
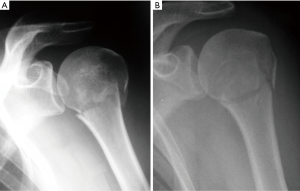
An intact rotator cuff balances the humeral head in a neutral position with the supraspinatus, infraspinatus, and teres minor muscles directing an external rotation force and the subscapularis muscle countering with an internal rotation force. Collectively, this maintains the humeral head centered on the glenoid in a neutral rotation. The pectoralis major and latissimus dorsi muscles produce an internal rotation and adduction force on the proximal humeral shaft, while the deltoid produces a superior directed force. In the setting of a surgical neck fracture of the proximal humerus, the humeral head and its rotator cuff attachments are effectively separated from the humeral shaft. In this scenario, the humeral head is held in a neutral position regardless of the position of the humeral shaft. Therefore, if the arm is in a standard sling, the humeral shaft will be relatively internally rotated with respect to the humeral head resulting in fracture malreduction. This phenomenon has been illustrated radiographically in Figure 1.
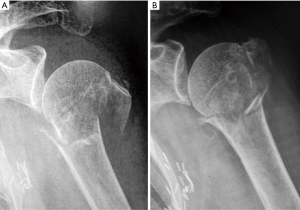
PHFs that involve an isolated greater tuberosity fracture or a three-part fracture with greater tuberosity involvement, have similar malreduction forces that may lead to malreduction of the fracture. The posterior rotator cuff muscles create a force vector that pulls the tuberosity fragment medially and posteriorly. If the arm is held in an internally rotated position, the remaining humeral head and shaft displace from the greater tuberosity fragment. If the humeral shaft is held in a neutral position, this force is decreased, improving the alignment of the fracture (Figure 2).
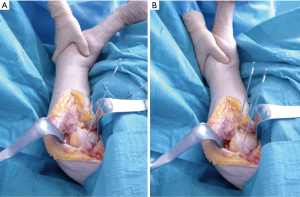
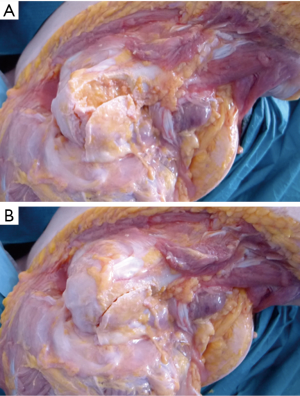
The theory that maintaining the arm a neutral rotation would better align PHFs was examined with a cadaveric model (Figure 3). The cadaveric specimens were dissected down to the intact rotator cuff. In the first specimen, one pin was driven into the humeral head and one in the humeral shaft. A surgical neck osteotomy was then performed to simulate a surgical neck fracture. As seen in Figure 3A, when the arm is held in internal rotation, the fracture displaces due to the rotator cuff maintaining the humeral head in a neutral orientation. When the arm is held in neutral rotation the fracture is well reduced. A greater tuberosity osteotomy was performed on another specimen, simulating an isolated greater tuberosity fracture. With the arm internally rotated, the fracture displaces posteriorly and with the arm in neutral the fracture is well reduced (Figure 3B). Fracture displacement also occurs with an isolated greater tuberosity osteotomy on a cadaveric model as shown in Figure 4. While a cadaveric specimen cannot account for the dynamic forces experienced in the shoulder, PHFs appear to maintain a more anatomic fracture alignment when the arm is held in a neutral rotation as opposed to internal rotation.
Length of immobilization
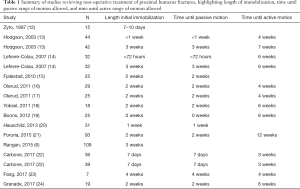
The length of time for shoulder immobilization varies significantly between providers. A search of rehabilitation protocols for non-operatively treated PHFs in the past twenty years demonstrates a range of time for shoulder immobilization. The protocols range from zero to four weeks of strict immobilization time, with two weeks being the most common length of time (Table 1).
Full table
With a shorter immobilization period, patients will theoretically have a faster recovery time but risk fracture displacement. With prolonged immobilization periods, patients theoretically have a lower risk of fracture displacement but are at risk of shoulder stiffness and slower return to function. Hodgson et al. compared immediate mobilization with physical therapy to delayed mobilization for three weeks in a randomized controlled trial. The authors found that patients with earlier mobilization had better pain and functional scores at 16 weeks post-injury but no statistical difference at one year (13). Lefevre-Colau et al. also compared early mobilization to delayed mobilization in a randomized controlled trial. The early mobilization group started physical therapy within 72 hours of the injury with passive range of motion and pendulum exercises with the other group delaying any mobilization for three weeks. The study found improved function and pain at six weeks and three months in the early mobilization group but no significant difference at six months post-injury (14). These randomized controlled trials suggest that early mobilization after a PHF will improve function and pain in patients in the early rehabilitation period but may affect the long-term outcome.
Physical therapy and home exercise protocols
The literature demonstrates variability in rehabilitation protocols for non-operatively treated PHFs. Most protocols entail a period of immobilization followed sequentially by passive range of motion exercises, active range of motion exercises, and finally strengthening exercises. Home exercise programs have been shown to be as effective as formal physical therapy when performed correctly (25). Most providers agree that a structured early rehabilitation program produces better results as has been shown in the literature (8).
Table 1 also highlights the timeframe that patients with a PHF were allowed to begin passive and active range of motion exercises in select protocols for conservatively treated PHFs. The median time until passive range of motion was allowed was two weeks and for active motion was six weeks. Carbone et al. recently compared early intensive mobilization to early conventional mobilization. Both groups started physiotherapy seven days after the injury with the intensive mobilization group starting pendulum exercises and assisted passive motion exercises five times a week for two weeks, followed by active motion three weeks post-injury. The conventional group did physical therapy sessions twice a week. This study found no advantage to early intensive mobilization (22).
Conclusions
A consensus on treatment protocol for non-operatively treated PHFs does not exist. The routine placement of PHFs in a standard sling keeps the humeral shaft internally rotated relative to the humeral head, causing potential displacement and malunion of the fracture. We propose that PHFs treated without surgery be placed in a neutral rotation shoulder immobilizer at the time of injury. We also encourage a standard rehabilitation protocol that includes pendulum and gentle range of motion exercises for the first two weeks after the injury. This is followed by two weeks of passive range of motion exercises, then two weeks of active range of motion exercises, and progression to full activity without restrictions at six weeks. A randomized controlled trial comparing results in patients with a standard sling and patients in a neutral shoulder immobilizer is necessary to further evaluate this proposal.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “Management of Fractures Around the Shoulder”. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-19-189). The series “Management of Fractures Around the Shoulder” was commissioned by the editorial office without any funding or sponsorship. AS served as the unpaid Guest Editor of the issue. AS reports personal fees from Medacta, outside the submitted work. PB reports personal fees from CONMED Linvatec, personal fees from Smith & Nephew, personal fees from Wright Medical Technology, Inc., outside the submitted work; and he serves on the editorial and governing board for Orthopedics. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barrett JA, Baron JA, Karagas MR, et al. Fracture risk in the U.S. Medicare population. J Clin Epidemiol 1999;52:243-9. [Crossref] [PubMed]
- Xie L, Ding F, Zhao Z, et al. Operative versus non-operative treatment in complex proximal humeral fractures: a meta-analysis of randomized controlled trials. Springerplus 2015;4:728. [Crossref] [PubMed]
- Bell J-E, Leung BC, Spratt KF, et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. J Bone Joint Surg Am 2011;93:121-31. [Crossref] [PubMed]
- Han RJ, Sing DC, Feeley BT, et al. Proximal humerus fragility fractures: recent trends in nonoperative and operative treatment in the Medicare population. J Shoulder Elbow Surg 2016;25:256-61. [Crossref] [PubMed]
- Neer CS. Displaced proximal humeral fractures. Part I. Classification and evaluation. By Charles S. Neer, I, 1970. Clin Orthop Relat Res 1987;3-10. [PubMed]
- Rangan A, Handoll H, Brealey S, et al. Surgical vs Nonsurgical Treatment of Adults With Displaced Fractures of the Proximal Humerus. JAMA 2015;313:1037. [Crossref] [PubMed]
- Handoll HH, Keding A, Corbacho B, et al. Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J 2017;99-B:383-92. [Crossref] [PubMed]
- Handoll HHG, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2012;12:CD000434 [Crossref] [PubMed]
- Beks RB, Ochen Y, Frima H, et al. Operative versus nonoperative treatment of proximal humeral fractures: a systematic review, meta-analysis, and comparison of observational studies and randomized controlled trials. J Shoulder Elbow Surg 2018;27:1526-34. [Crossref] [PubMed]
- Rommens PM, Heyvaert G. Conservative treatment of subcapital humerus fractures. A comparative study of the classical Desault bandage and the new Gilchrist bandage. Unfallchirurgie 1993;19:114-8. [Crossref] [PubMed]
- Conti M, Garofalo R, Castagna A. Does a brace influence clinical outcomes after arthroscopic rotator cuff repair? Musculoskelet Surg 2015;99:S31-5. [Crossref] [PubMed]
- Zyto K, Ahrengart L, Sperber A, et al. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br 1997;79:412-7. [Crossref] [PubMed]
- Hodgson SA, Mawson SJ, Stanley D. Rehabilitation after two-part fractures of the neck of the humerus. J Bone Joint Surg Br 2003;85:419-22. [Crossref] [PubMed]
- Lefevre-Colau MM, Babinet A, Fayad F, et al. Immediate Mobilization Compared with Conventional Immobilization for the Impacted Nonoperatively Treated Proximal Humeral Fracture. J Bone Joint Surg Am 2007;89:2582-90. [Crossref] [PubMed]
- Fjalestad T, Hole MØ, Jørgensen JJ, et al. Health and cost consequences of surgical versus conservative treatment for a comminuted proximal humeral fracture in elderly patients. Injury 2010;41:599-605. [Crossref] [PubMed]
- Olerud P, Ahrengart L, Ponzer S, et al. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011;20:747-55. [Crossref] [PubMed]
- Olerud P, Ahrengart L, Ponzer S, et al. Hemiarthroplasty versus nonoperative treatment of displaced 4-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011;20:1025-33. [Crossref] [PubMed]
- Yüksel HY, Yimaz S, Akşahin E, et al. The Results of Nonoperative Treatment for Three- and Four-Part Fractures of the Proximal Humerus in Low-Demand Patients. J Orthop Trauma 2011;25:588-95. [Crossref] [PubMed]
- Boons HW, Goosen JH, van Grinsven S, et al. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. Clin Orthop Relat Res 2012;470:3483-91. [Crossref] [PubMed]
- Hauschild O, Konrad G, Audige L, et al. Operative versus non-operative treatment for two-part surgical neck fractures of the proximal humerus. Arch Orthop Trauma Surg 2013;133:1385-93. [Crossref] [PubMed]
- Foruria AM, Martí M, Sanchez-Sotelo J. Proximal Humeral Fractures Treated Conservatively Settle During Fracture Healing. J Orthop Trauma 2015;29:e24-30. [Crossref] [PubMed]
- Carbone S, Razzano C, Albino P, et al. Immediate intensive mobilization compared with immediate conventional mobilization for the impacted osteoporotic conservatively treated proximal humeral fracture: a randomized controlled trial. Musculoskelet Surg 2017;101:137-43. [Crossref] [PubMed]
- Fang C, Kwek EBK. Self-reducing proximal humerus fractures. J Orthop Surg (Hong Kong) 2017;25:2309499017717180 [Crossref] [PubMed]
- Roberson TA, Granade CM, Hunt Q, et al. Nonoperative management versus reverse shoulder arthroplasty for treatment of 3- and 4-part proximal humeral fractures in older adults. J Shoulder Elbow Surg 2017;26:1017-22. [Crossref] [PubMed]
- Bertoft ES, Lundh I, Ringqvist I. Physiotherapy after fracture of the proximal end of the humerus. Comparison between two methods. Scand J Rehabil Med 1984;16:11-6. [PubMed]
Cite this article as: Joyce CD, Seidl A, Boileau P. Concept of neutral rotation sling for non-operative treatment of proximal humerus fractures. Ann Joint 2021;6:17.


