Complications after ORIF of proximal humerus fractures—how to deal with them
Introduction
The advent of proximal humeral locking plates led to increased enthusiasm and utilization in the setting of open reduction and internal fixation (ORIF) of displaced proximal humerus fractures (PHFs). However, complications associated with use of this technology became rapidly apparent. This was especially true in the setting of elderly fractures, particularly three- and four-part fractures. In this setting, the rate can be as high as 30–40% (1-5).
Failures of proximal humeral locking plates can be mechanical, biological, or infectious. The first priority in management of complications is avoidance. This may be enabled with careful patient selection, a principle-based surgical technique, and close postoperative management.
The goals of this review include a discussion of mechanisms of avoidance of complications after ORIF of PHFs, as well as a description of mechanisms of treatment to salvage this difficult situation.
Avoidance of failure
While postoperative management of the failed ORIF of a PHF can lead to improved outcomes, it is undoubtedly better to avoid this complication primarily. It is our opinion that with careful patient selection, a principal based surgical technique, and close postoperative management, complications and re-operations in the setting can be minimized.
As described, complications can be mechanical, biological, or infectious. While avoidance of infection cannot always be obtained, biological and mechanical complications, in our opinion, can be mitigated. At our institution, we recently reviewed the failure rate of ORIF in a series of elderly patients. While mechanical failures were rare, biological failures were common, particularly in three- and four-part fractures in the elderly. For this reason, the first critical decision is whether a patient is a candidate for ORIF. In our practice, we avoid ORIF for patients with the following characteristics:
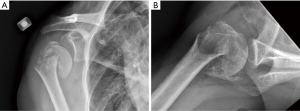
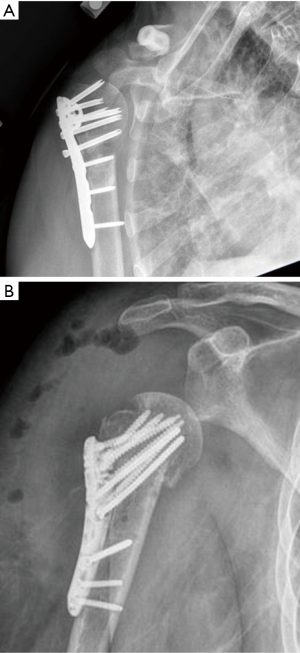
- Elderly patients, with three- and four-part fractures (Figure 1A,B);
- Middle-age (40–60 YO) patients with three- and four-part fractures and associated head dislocations (Figure 2A,B);
- Middle-age (40–60 YO) patients with complex medical comorbidities that would lead to a high rate of failure and avascular necrosis (dialysis, transplant, severe diabetes, etc.).
Avoiding ORIF in this patient group will lead to a substantial decrease in biological failures. Most biological failures in our series were related to avascular necrosis, which is related to perfusion of the head segment (1). Increasing comminution and displacement of the tuberosity segments, head dislocation, and a short calcar segment have been reliably and reproducibly correlated with avascular necrosis. These are factors that we consider prior to undertaking ORIF.
In addition to biological considerations with ORIF, it is critically important that mechanical/surgical failures are avoided. Studies have demonstrated a high rate of varus collapse, intra-articular screw penetration (many of which are immediately after surgery) and hardware failure after ORIF. It is our opinion that with careful surgical technique, many of these risks can be mitigated.
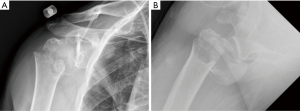
We utilize a principle-based technique that relies on stable, even if non-anatomic reduction of the PHF, with the proximal humeral locking plate applied as a neutralization plate. This principle-based technique has been well described elsewhere (6). In brief, through a deltopectoral approach, we aim for a valgus reduction of the proximal humerus. We insist upon a stable reduction obtained between the shaft and the head segment. If there is substantial posteromedial comminution, a short segment of allograft fibula is added for support (Figure 3). The fracture is pinned in place, and a plate is applied as a neutralization plate (rather than as a tool for reduction as has been previously described). Screws are left short in order to avoid intra-articular screw penetration (particularly posterior-superior screws). Sutures are liberally used to neutralize the pull of the rotator cuff on the tuberosity fragments.
At our institution, we have demonstrated a low rate of mechanical failure when this principle-based approach is utilized and the following criteria are met:
- The head segment is in valgus (greater than 130 degrees);
- There is medial head support (with the humeral shaft or fibular allograft). In the majority of cases this involves calcar screws as well (screws in the infero-medial aspect of the humeral head);
- The greater tuberosity is below the humeral head;
- The top of the plate is applied below the greater tuberosity;
- Screws are extra-articular (confirmed with dynamic fluoroscopy);
- Sutures are used liberally between the rotator cuff and the plate.
While early range of motion exercises have been advocated to avoid postoperative stiffness, it is our practice that early and aggressive range of motion is not necessary. We have seen very limited post-surgical stiffness after ORIF, particularly in the elderly. In cases of postsurgical stiffness, corticosteroid injections and physical therapy have been effective to regain mobilization. Bony union of the proximal humerus is substantially more important (and more difficult to salvage if it is not achieved) than early range motion.
Evaluation of the failed ORIF PHF
In spite of careful patient selection, meticulous surgical techniques, and close postoperative surveillance, there remains a significant rate of failure of ORIF for PHF. The shoulder specialist is charged with improving shoulder function, as well as decreasing pain for patients in this setting. These patients are frequently frustrated, in many cases have complex social and medical backgrounds, and have problems that may be difficult to salvage.
We begin the evaluation of the failed PHF with a careful history and physical exam. Critical factors to ascertain include:
- Pre-fracture shoulder pain and management (injections, surgery, etc.);
- Pre-surgical timelines (Time from fracture to surgery);
- Postoperative wound healing and drainage;
- Neurovascular status pre- and post-surgery;
- Patient goals, expectations, and functional status;
- Previous operative notes and findings at outside facilities.
In addition to a careful history and physical exam, preoperative imaging studies including radiographs [grashey (internal rotation), grashey (external rotation), scapular y, and axillary view] are necessary. In most cases of failed ORIF, we use computed tomography (CT) scans with metal suppression and three-dimensional reconstructions.
We pay particular attention to a few critical issues that will affect our management:
Axillary nerve function
Axillary nerve dysfunction is common after PHF, even in the setting of nonsurgical management. While “pre-surgical” axillary nerve dysfunction, related to the injury, is likely to resolve, this may be complicated in the setting of surgical management, in which case the axillary nerve could have been surgically injured or traumatized. We have a low threshold for EMG evaluations and referral to a brachial plexus specialist in the setting of axillary nerve dysfunction or deltoid weakness. This will be critical to understand prior to consideration of surgical reconstruction.
Infection
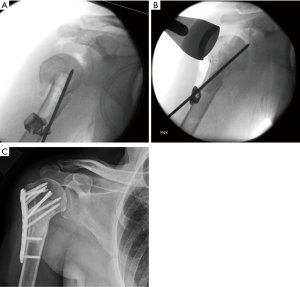
Patients should be carefully questioned for a history of postoperative wound drainage, surgical irrigation and debridements, and prolonged postoperative antibiotics. These can provide an indication of an underlying infection. In some cases, treating surgeons may have minimized infectious complications to the patient. Therefore, it is critical to ask each of these questions individually (Figure 4). In addition to a careful history and physical exam, in almost all cases of failed ORIF for PHF, an ultrasound or fluoroscopically guided aspiration of the joint is completed. We send aspirations for cell count as well as holding the cultures for two weeks to assess for cutibacterium acnes.

Bone loss
After ORIF, there can be profound bone loss on the humeral side, as well as occasionally on the glenoid side. The glenoid side can be particularly affected when locking screws have eroded through the humeral head and have damaged the articular surface of the glenoid and associated subchondral bone (Figure 5). In many cases of neglected humeral nonunions, there can be profound humeral bone loss as well. This can complicate surgical treatment options.
Rotator cuff
While the majority of reconstructive options in the setting of failed PHF surgery are based upon the reverse total shoulder arthroplasty (rTSA), there are certain indications in which salvage can be contemplated. In these cases, a functional rotator cuff will be necessary. In addition to exam (which is typically less helpful in this setting) we utilize the sagittal reconstructions of the CT scan to assess the rotator cuff in these patients.
Surgical treatment options
Revision ORIF
In young patients with preserved bone stock and humeral head anatomy, revision open reduction, internal fixation can be contemplated. Most commonly, this is in the setting of nonunion of the surgical neck, with non-fractured or anatomically fixed (and healed) tuberosity fragments. Typically, this is in patients under 60 years of age. Criteria for revision ORIF include:
- Preserved glenohumeral cartilage articulation;
- Anatomically healed or nonfractured tuberosities;
- Absence of infection;
- Adequate humeral head bone stock for fixation;
- Young patient (<60);
- Functional deltoid.
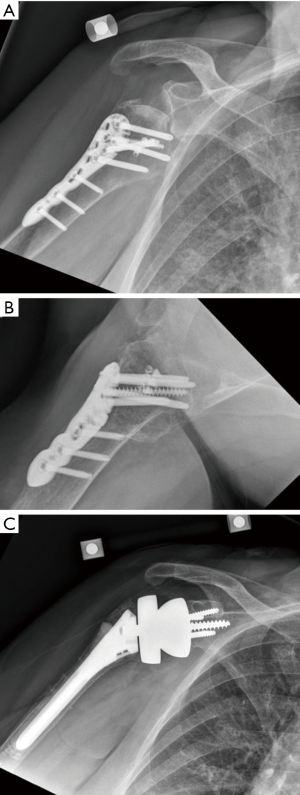
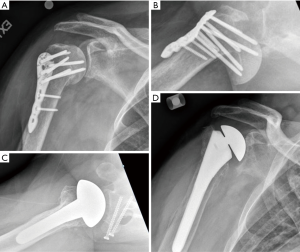
We approach ORIF in the revision setting using the previously described principle-based approach. We particularly will accept substantial proximal humeral shortening in this setting to get compression through the metaphysis of the surgical neck (Figure 6A,B).
Using a plate with multidirectional locking screws can accommodate this plate position and avoid previous screw holes. In some cases, biological augmentation with autograft iliac crest can be added to stimulate union.
Hemiarthroplasty
While rTSA has taken over as the main treatment of choice for displaced PHF, there may remain a role of hemiarthroplasty in select patients with failed ORIF. Patients who may benefit from hemiarthroplasty include patients who have:
- Unreconstructable/unlikely salvageable glenohumeral cartilage articulation;
- Salvageable tuberosities/functional rotator cuff;
- Functional deltoid;
- Young age (<50).
These situations are complex and failure rate remains high. In this setting, the majority of failures will be related to failure of the tuberosities/rotator cuff. For this reason, we believe it is important to use a convertible stem system—to allow for a more straightforward revision to rTSA in the setting of functional cuff deficiency. Surgical technique in the setting of hemiarthroplasty mirrors that of rTSA and will be documented in the subsequent section (Figure 7).
rTSA
The vast majority of patients with failed ORIF will be revised to rTSA. This is a reliable and reproducible option that does not depend on the function and status of the rotator cuff. While functional outcomes are not always reproducible, pain relief is reliable with this approach. While it was previously controversial, recent literature has suggested that reduction and healing of the tuberosities leads to improved function in the setting of rTSA for fracture (7). We believe this is also true in the setting of failed open reduction, internal fixation. Criteria for consideration of rTSA relies on:
- Glenoid bone stock adequate for glenoid baseplate fixation;
- Functional deltoid.
Surgical technique
We utilize a deltopectoral approach. In most cases, a previous deltopectoral approach has been utilized and the same incision can be used. In the setting of a previous deltoid splitting approach, we will most commonly convert this to a deltopectoral approach with either a separate skin incision (if separated by 5 cm) or with an extension of the previous skin incision and a different subcutaneous plane.
Careful identification of the deltopectoral interval and mobilization of the deltoid off the proximal humerus and rotator cuff is an important maneuver. We typically do this before removing any hardware. If the interval between the conjoint tendon and subscapularis can be identified and mobilized, the axillary nerve is typically palpated and protected (but not necessarily visualized). In the setting of profound scarring in this interval, we prefer to mobilize the subscapularis by working from inside the joint, and avoid dissection and trauma to the axillary nerve.
Management of the subscapularis depends up on the injury. In most cases, we will mobilize the lesser tuberosity for later repair if fractured and not united. If united, we will typically use an osteotomy, and incorporate the lesser tuberosity into our repair. The proximal humeral plate can then be removed. The head can be removed next and the joint and proximal shaft can be exposed.
In the setting of revision surgery, we will typically obtain 5 five cultures, each of which is held for two weeks to identify indolent infection, particularly by cutibacterium acnes. The proximal humerus is then prepared per manufacturer guidelines. If there is a supportive metaphysis, a press-fit humeral component can be utilized. In many cases, cement is utilized to augment fixation. After preparing the humeral canal, the tuberosities can be better mobilized and adhesions between the tuberosity and rotator cuff and the under-surface of the acromion can be lysed.
We next turn our attention to glenoid exposure. This begins with opening of the rotator interval to the level coracoid and mobilization of the subscapularis off the under surface of the coracoid at the rotator interval. The capsule and labrum can be removed from the anterior aspect of the glenoid. The posterior labrum and biceps tendon stump can be excised. Meticulous dissection of the inferior labrum off the glenoid is critical in order to identify the true inferior border of the glenoid and avoid high baseplate placement. We utilize our preoperative CT scan, and cannulated pin guides to place our centering pin and prepare the glenoid. We prefer cannulated glenoid preparation in order to ensure appropriate location, inclination, and version of our glenoid baseplate. Style and design of baseplate are up to surgeon’s discretion, however, we prefer a slightly lateralized design with a varus neck shaft angle on the humeral component.
After placement of the baseplate, we turn our attention back to the humeral component. We prefer to trial the reduction at this stage prior to tuberosity management. If we are happy with stability, the real humeral component can be placed. Prior to placement of the real humeral component, we place a series of sutures around the greater tuberosity which will enable reduction to the humeral stem. We utilize two high tensile sutures high in the greater tuberosity segment (at supraspinatus /infraspinatus junction) and two sutures low in the greater tuberosity segment (infraspinatus/teres junction). All sutures are passed through the medial portion of the stem. The real components are impacted or cemented into place and the shoulder is reduced. One high and one low suture through the greater tuberosity are tied to themselves around the greater tuberosity and the humeral component. The other two sutures are passed around the lesser tuberosity and tied around both the greater and lesser tuberosity segments.
The wound is copiously irrigated with normal saline. We also use adjuvant betadine irrigation to mitigate infection risk. The patient is placed into a sling and typically stays in the hospital overnight for pain control and medical management. In the setting of suspicion for infection, oral antibiotics are maintained until 2-week cultures are negative.
Fusion
With expanded use of the rTSA, fusion has been less commonly employed, even in the setting of profound anatomical distortion.
Criteria for fusion includes:
- Nonfunctional and nonreconstructible deltoid (failed nerve transfer or not a candidate for pedicled pectoralis transfer);
- Patient acceptance of motion limitation in exchange for pain relief.
Our preferred technique fuses the humeral head to both the glenoid and acromion. Further detail on this technique is beyond the scope of this article.
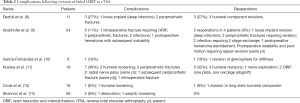
Outcomes
Given the relatively limited indications for revision ORIF and hemiarthroplasty after failed PHF fixation, the predominance of the literature centers around outcomes after rTSA. This literature is summarized in Tables 1,2. In all series, range of motion and outcome scores were significantly improved following revision to rTSA (compared with preop scores). The clinical outcomes, however, are consistently worse (both functional outcomes and complication rates) than those achieved in patients treated for non-fracture indications. Furthermore, in two of three studies, they are worse than those treated acutely with rTSA. This has been confirmed in a large population-based study (19% revision for rTSA after ORIF vs. 4% revision for acute rTSA after fracture) (14).

Full table
Full table
Conclusions
Savage of failed ORIF of PHF is complex and challenging. The need for revision of ORIF can be mitigated through careful patient selection, surgical technique, and postoperative management. A thorough workup includes assessment of infection, bone loss, rotator cuff function, and axillary nerve function. In select indications, revision ORIF, hemiarthroplasty, and fusion are indicated. In most cases, revision to rTSA will be the most reliable option. Revision to rTSA results in reliable improvement in function, but has worse functional outcomes and a higher complication rate than primary rTSA for fracture.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Adam Seidl) for the series “Management of Fractures Around the Shoulder” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-77). The series “Management of Fractures Around the Shoulder” was commissioned by the editorial office without any funding or sponsorship. JDB reports personal fees from Stryker, outside the submitted work. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barlow JD, Logli AL, Steinmann SP, et al. Locking plate fixation of proximal humerus fractures in patients older than 60 years continues to be associated with a high complication rate. J Shoulder Elbow Surg 2020;29:1689-94. [Crossref] [PubMed]
- Bayer J, Hammer T, Maier D, et al. Emergency radiological examination of the externally stabilized pelvis--there is a catch to it: lessons learned from two cases with symphyseal disruption despite initial inconspicuous computed tomography. BMC Surg 2016;16:11. [Crossref] [PubMed]
- Oppebøen S, Wikerøy AKB, Fuglesang HFS, et al. Calcar screws and adequate reduction reduced the risk of fixation failure in proximal humeral fractures treated with a locking plate: 190 patients followed for a mean of 3 years. J Orthop Surg Res 2018;13:197. [Crossref] [PubMed]
- Padegimas EM, Zmistowski B, Lawrence C, et al. Defining optimal calcar screw positioning in proximal humerus fracture fixation. J Shoulder Elbow Surg 2017;26:1931-7. [Crossref] [PubMed]
- Schnetzke M, Bockmeyer J, Porschke F, et al. Quality of reduction influences outcome after locked-plate fixation of proximal humeral type-C fractures. J Bone Joint Surg Am 2016;98:1777-85. [Crossref] [PubMed]
- Barlow JD, Sanchez-Sotelo J, Torchia M. Proximal humerus fractures in the elderly can be reliably fixed with a "hybrid" locked-plating technique. Clin Orthop Relat Res 2011;469:3281-91. [Crossref] [PubMed]
- Jain NP, Mannan SS, Dharmarajan R, et al. Tuberosity healing after reverse shoulder arthroplasty for complex proximal humeral fractures in elderly patients-does it improve outcomes? A systematic review and meta-analysis. J Shoulder Elbow Surg 2019;28:e78-91. [Crossref] [PubMed]
- Dezfuli B, King JJ, Farmer KW, et al. Outcomes of reverse total shoulder arthroplasty as primary versus revision procedure for proximal humerus fractures. J Shoulder Elbow Surg 2016;25:1133-7. [Crossref] [PubMed]
- Grubhofer F, Wieser K, Meyer DC, et al. Reverse total shoulder arthroplasty for failed open reduction and internal fixation of fractures of the proximal humerus. J Shoulder Elbow Surg 2017;26:92-100. [Crossref] [PubMed]
- García-Fernández C, Lopiz Y, Rizo B, et al. Reverse total shoulder arhroplasty for the treatment of failed fixation in proximal humeral fractures. Injury 2018;49:S22-6. [Crossref] [PubMed]
- Hussey MM, Hussey SE, Mighell MA. Reverse shoulder arthroplasty as a salvage procedure after failed internal fixation of fractures of the proximal humerus: outcomes and complications. Bone Joint J 2015;97-B:967-72. [Crossref] [PubMed]
- Cicak N, Klobucar H, Medancic N. Reverse shoulder arthroplasty in acute fractures provides better results than in revision procedures for fracture sequelae. Int Orthop 2015;39:343-8. [Crossref] [PubMed]
- Shannon SF, Wagner ER, Houdek MT, et al. Reverse shoulder arthroplasty for proximal humeral fractures: outcomes comparing primary reverse arthroplasty for fracture versus reverse arthroplasty after failed osteosynthesis. J Shoulder Elbow Surg 2016;25:1655-60. [Crossref] [PubMed]
- Nowak LL, Hall J, McKee MD, et al. A higher reoperation rate following arthroplasty for failed fixation versus primary arthroplasty for the treatment of proximal humeral fractures: a retrospective population-based study. Bone Joint J 2019;101-B:1272-9. [Crossref] [PubMed]
Cite this article as: Barlow JD. Complications after ORIF of proximal humerus fractures—how to deal with them. Ann Joint 2021;6:16.