
Current perspectives on elbow dislocation and instability
Introduction
The elbow is the second most commonly dislocated joint in adults. Simple dislocations have been described as those where there is no concomitant fracture other than small periarticular avulsions under 2mm in diameter. Where larger fragments are present it is classified as a fracture dislocation (1,2). The annual incidence of simple elbow dislocations is approximately 5.21 per 100,000 persons, slightly more frequent than fracture dislocations with a 53% male predominance (1). Falling from a standing height is the most common mechanism of injury (56%) while sporting activities accounted for 44% of elbow dislocation (3).
Anatomy
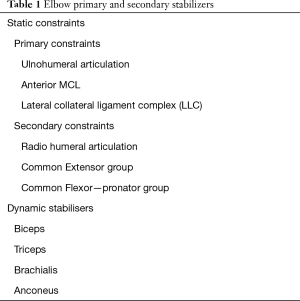
The elbow joint is comprised of bony, capsuloligamentous, and neuromuscular structures (Table 1).
Full table
Bony structures
Medially the ulnohumeral articulation consists of the trochlea and its reciprocating greater sigmoid cavity. The olecranon forms the posterior and central sections of the cavity, accommodating the triceps insertion at its proximal aspect and continuing as the ulna diaphysis distally. The coronoid process is a fan shaped structure with 2 discrete articular facets, anteromedial and anterolateral, which are separated by a ridge that runs the length of the greater sigmoid notch. The sublime tubercle is an important element of the medial side of the coronoid where the strong anterior bundle of the medial collateral ligament inserts. Laterally the radial head forms a shallow concave surface that only covers the capitellum over an arc of 90 degrees and so the lateral compartment has greater reliance on soft tissue restraints (4-6).
Capsuloligamentous structures
The elbow is bordered by medial and lateral collateral ligament complexes (LLC). The medial collateral ligament complex (MCLC) consists of anterior (aMCL), posterior (pMCL), and transverse components. The anterior bundle originates from the antero-inferior surface of the medial epicondyle of the humerus and inserts onto the sublime tubercle (7). The posterior bundle plays a greater role in stability in the context of associated injury (8,9).
The LLC consists of the radial collateral ligament (RCL), lateral ulnar collateral ligament (LUCL), accessory lateral ulna collateral ligament (AUCL), the annular ligament (AL), and the posterolateral ligament (PL) (10). The AL encircles the radial head with attachments to the anterior and posterior margins of the lesser sigmoid notch. The RCL, LUCL, and AUCL have a common origin at the inferior surface of the lateral epicondyle at the centre of the axis of rotation. The PL arises more posteriorly. The LUCL inserts on the crista supinatoris, the RCL inserts onto the annular ligament, and the less substantial accessory collateral ligament attaches to both (10-12). The PL inserts to the margin of the greater sigmoid notch proximal to the supinator crest.
Neuromuscular structures
The biceps, brachialis, triceps, and anconeus muscles cross the elbow and provide proprioceptive feedback as well as stability through dynamic compression across the articular surfaces. The anterior capsule inserts approximately 5mm distal to the joint line, whilst the strong and broad insertion of brachialis muscle lies just distal to this reinforcing the coronoid process (Table 1). The resultant moment of the triceps, biceps, brachialis and common extensor, and flexor-pronator mass pulls the forearm bones proximally and posteriorly on to the end of the humerus (11,13).
Elbow stability
Elbow stability is derived from a combination of the osseous, capsuloligamentous, and neuromuscular structures described above. These are traditionally categorised into primary and secondary stabilisers according to their relative contributions, and static constraints or dynamic restraints according to their mechanism of action (Table 1).
Primary stabilisers
The primary static constraints include the bony ulnohumeral articulation, the LLC, and aMCL. The contrasting levels of joint congruity between the medial and lateral bony articulations explain the greater importance of the lateral soft tissue structures.
Medially, the highly congruous relationship of the trochlea and greater sigmoid cavity has been said to contribute up to 50% of elbow stability. The coronoid and olecranon together enclose the trochlea through an arc of 170 degrees producing a high degree of concavity compression. The anteromedial coronoid facet has a mean surface area of 232 mm2, compared to a mean radial head surface area of 247 mm2, making the anteromedial facet a vital primary varus stabiliser. The anterolateral facet has a smaller mean surface area of 142 mm2 and is a second-degree valgus stabiliser acting in conjunction with the radial head (13-16).
The MCLC provides stability in valgus and posteromedial direction with the anterior bundle being the most important contributor to valgus stability throughout flexion arc. The pMCL functions primarily in providing posteromedial rotatory stability (17-19) (Table 2).

Full table
The LLC is the primary stabiliser to external rotation and varus stress. The posterolateral ligament has recently been shown to be of significant importance to posterior stability of the radial head (10). Therefore, LLC insufficiency not only causes varus and posterolateral instability but also subluxation of the radial head posteriorly (16,20) (Table 2).
Secondary stabilisers
The secondary stabilisers, which take on an important role in the context of injury to the primary stabilisers, include the radial head, the anterior capsule, and the musculotendinous structures crossing the elbow joint which have a combination of passive and active stabilising effects.
Forearm rotation has a significant impact on valgus - varus laxity with maximum laxity noted in neutral forearm rotation throughout the elbow flexion (21). The stabilising effect of biceps, brachialis, or triceps is independent of forearm rotation (17). The role of the common flexors as valgus stabilisers has been demonstrated in a cadaveric study evaluating the throwing action. The maximal valgus force generated during throwing is higher than the load to failure of the MCL illustrating the need for secondary valgus stabilisers to maintain stability. Stimulation of the FCU and FDS is able to restore stability in a MCL deficient cadaveric model (22). The muscles from the common extensor origin (CEO) have maximal tension in full pronation where they function most effectively as a varus stabiliser (17). Anconeus is assumed to act as a dynamic constraint to both varus and posterolateral instability (23-25). It follows that forearm rotation may play a role in stabilising the elbow joint in the presence of injury. Supination stabilises the MCL deficient elbow and those in which there is a large coronoid fracture, whereas pronation stabilises the LCL deficient elbow (26-28). This is supported by the clinical work of Josefsson et al. who identified disruption of the common flexor and extensor origins as an important determinant of instability after simple elbow dislocation (29,30).
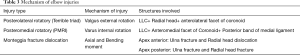
Mechanism and pathoanatomy (Table 3)
Full table
The mechanisms of injury for simple and fracture dislocation of the elbow are determined by injury factors including the rate of application and direction of force, and patient factors including bone quality.
Simple elbow dislocations
Simple elbow dislocations can be grouped into posterolateral, posterior, posteromedial, divergent (paediatric injuries), and anterior dislocations (extremely uncommon without fractures). The most common direction of elbow dislocation is posterolateral. The exact mechanism remains the subject of debate.
MRI studies support a valgus hyperextension model for the more common posterolateral dislocations (31-33). The valgus hyperextension theory proposes that dislocations occur following a fall onto a hyperextended elbow. As elbow goes into hyperextension and valgus, the MCL fails first followed by the LLC, and then the common flexor origin (CFO). Further displacement leads to disruption of anterior capsule (AC) followed by CEO. Posterior capsule (PC) tear though rare is seen only in case with complete CEO disruption (13,31).
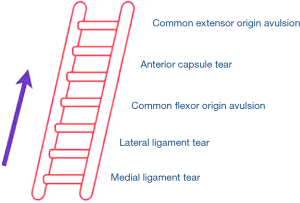
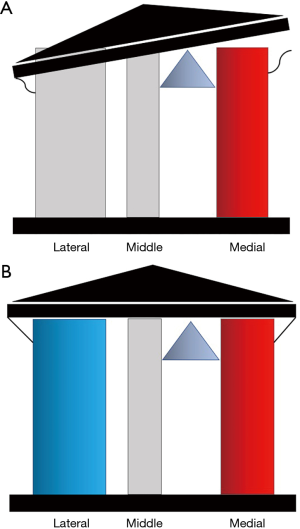
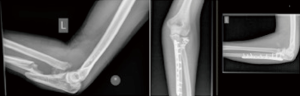
Schreiber et al. (34), in their study on video analysis of elbow dislocations, showed that most elbow dislocations occur as a result of hyperphysiologic valgus moment in an extended elbow with the typical arm position at the time of dislocation being forearm pronation, elbow extension, and shoulder abduction with forward flexion. This may result in a spectrum of injury (Figure 1) from grade 1 isolated medial ligament tear, grade two medial and lateral ligament, grade 3 ligamentous and CFO avulsion, and grade 4 (Figure 2) where all soft tissue stabilisers have been avulsed including the common extensor origin (31).
Posteromedial dislocations account for approximately 10% of all elbow dislocations and may follow a valgus external rotation model. Posteromedial dislocation are associated with severe soft tissue injury to the lateral ligament complex (LLC) on MRI scans (31,35).
O’Driscoll et al. (5,36) described sequential lateral to medial soft tissue disruption as “Horii circle”, beginning with partial or complete disruption of LUCL, leading to posterolateral rotatory subluxation (stage 1). Further anterior and posterior disruption leads to incomplete posterolateral dislocation (stage 2). Stage 3 describes progressive damage to the medial capsuloligamentous and musculotendinous structures resulting in complete dislocation. The valgus external rotation theory has been proposed with injury occurring as a result of a fall on a partially extended elbow. The force transmitted via the forearm is a combination of lateral rotation and valgus strain. This is due to the cam effect of the lateral sloping medial side of the trochlea. The greatest displacement is on the outer side of the joint leading to stripping of the lateral ligament sleeve and tearing of the posterolateral capsule (Osborn Cotterill ligament). As a result of this, the radial head rotates backwards from the capitellar surface. This may be the model for simple posteromedial dislocation that account for 10% of simple dislocations, but can also result in fracture dislocation.
Elbow instability
Posterolateral rotatory instability (PLRI)
Chronic PLRI, characterised by posterior subluxation of the radial head over the capitellum, typically occurs after a posterior or posterolateral subluxation/dislocation, and involves injury to all or parts of the lateral primary and secondary stabilising structures (LLC, posterolateral ligament and common extensor origin). Grade 1 PLRI follows an isolated posterior ligament avulsion resulting in positive drawer test but negative pivot shift test. Grade 2 PLRI (positive drawer and pivot shift test) is as a result of an LLC avulsion with or without posterior ligament involvement. Over a period of time repetitive subluxation and spontaneous reduction of the radio-capitellar joint leads to progressive lateral degeneration (10,13,16,37,38).
Valgus extension overload (VEO)
Throwing generates an average of 64Nm of valgus stress of which half is taken by MCL and the rest by the secondary and dynamic stabilisers (39). Risk factors for increased valgus laxity include; late trunk rotation, reduced shoulder external rotation, increased elbow flexion, and distal migration of the medial epicondyle in injuries to skeletally immature athletes (40,41).
Valgus loading results in MCL strain, compression of the radio-capitellar joint, and shearing forces at the posterior aspect of the elbow between the medial aspect of the tip of the olecranon and the olecranon fossa. Repetitive and/or high valgus stress can lead to attenuation or partial/complete tears of the MCL. The ensuing increased MCL strain can result in osteochondral capitellar lesions, loose bodies, and cartilage damage at the olecranon fossa leading to the classic finding of posteromedial osteophytes “kissing lesion”. Associated lesions may include; ulnar neuritis, flexor-pronator tendinopathy, or medial epicondyle apophysitis in skeletally immature (42-44).
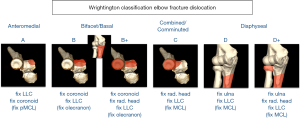
Fracture dislocations
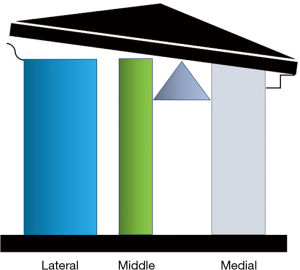
To understand the impact of fractures of the coronoid, proximal ulnar, and radial head on elbow instability a three-column proximal forearm model has been proposed with a corresponding classification system (Table 4) (16). The medial column is formed by the medial trochlea and anteromedial coronoid facet. The middle column is formed by the lateral trochlea and the anterolateral coronoid facet, and the lateral column is formed by the capitellum and radial head (Figures 3,4). A fulcrum exists between the middle and medial columns. The primary restraint to valgus collapse is therefore the lateral column with a secondary contribution from the middle column. The medial column is the only restraint to varus collapse. When the lateral column is intact the middle column has no significant stabilising role however removal of the lateral column makes the middle column essential for valgus stability (Figure 5). Osseous injures are associated with characteristic soft tissue injuries which further contribute to instability. The key soft tissue structure in most fracture dislocations is the LLC, which in most cases is avulsed from the humeral side.

Full table


Wrightington type A
Type A injuries are medial column injuries (anteromedial coronoid facet) without injury to the middle column (anterolateral facet). These injuries are typically the results of a posteromedial fracture dislocations (19,38,45,46). As the primary varus restraint, significant damage to the medial column can lead to varus collapse and gross instability or varus posteromedial rotatory instability (VPRI) (Figures 6,7)
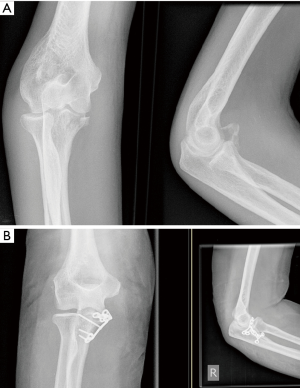
The obligate injury in VPRI, characterised by posteromedial elbow subluxation, is humeral detachment of the LLC. Loss of this key primary stabiliser permits posteromedial subluxation of the elbow joint resulting in impaction of the coronoid and trochlea with a potential anteromedial coronoid facet fracture. Further progression of deformity can lead to involvement of posterior band of medial collateral ligament (pMCL) (38,47). Recent studies have shown that isolated disruption of the pMCL causes an increase in varus angulation and internal rotation during flexion under varus load (8,9). Hwang et al. (19) studied the role of pMCL in the VPRI and found out that pMCL has to be disrupted for gross dislocation of the elbow to occur. If VPRI is not recognised and appropriately treated, the application of varus stress may cause opening of lateral ulnohumeral joint and point loading of medial ulnohumeral joint. Over time, this increase in medial contact forces can lead to early osteoarthritis (48,49).
Wrightington B/B+
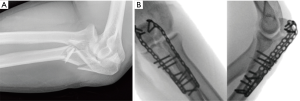
Type B are bifacet fractures (Figures 8) involving the middle and medial column. Bifacet fractures can occur in isolation as part of an extension type Monteggia fracture dislocation, or less commonly in posteromedial fracture dislocations with lateral extension of the anteromedial facet fracture. There may be an associated olecranon fracture or radial head fracture (Type B+, Figure 9). The latter results in a three-column injury with a poor prognosis if not recognised and managed appropriately. Monteggia fracture dislocations are more likely to occur in patients with osteoporotic bone and may be associated with coronoid comminution and extension to the sublime tubercle.

Wrightington Type C (Combined anterolateral facet and radial head/comminuted radial head)
A combined radial head and anterolateral facet fracture is a terrible triad injury. Loss of all valgus osseous restraints leads to instability. Isolated radial head fractures are single column injuries which are unlikely to lead to instability however highly comminuted fractures should raise the suspicion of higher energy injuries with associated damage to the medial and lateral soft tissue structures and possible resultant instability (Type C, Figure 5). These injuries may require lateral column reconstruction and soft tissue stabilisation as PLRI can occur in the presence of a minor radial head fracture with an associated avulsion of the posterolateral ligament (Osborn Cotterill Ligament) or LLC as described earlier (10,16,37).
Wrightington D/D+
Type D injuries are proximal ulna fracture dislocations in which the fracture is distal to the coronoid which remains in continuity with the olecranon. The middle and medial columns of the elbow joint remain intact (Type D). The radial head may be dislocated and intact (Type D) or fractured (Type D+, Figure 10). What differentiates a type D from type B injury is an intact coronoid and hence a stable ulnohumeral articulation. In a type D with an intact radial head the lateral ligament is frequently avulsed at its origin.
Assessment
An assessment of any significant elbow injury begins with a detailed history focussing on the mechanism of dislocation and any subjective feeling of elbow instability. The elbow should be examined for bruising over the medial or lateral side. Lateral bruising is an indicator of high-grade injury (13). Any open wounds should be managed according to local guidelines. Ligament examination in the acute setting is challenging. Reluctance to actively move the elbow may be a sign of more significant soft tissue or bony injury.
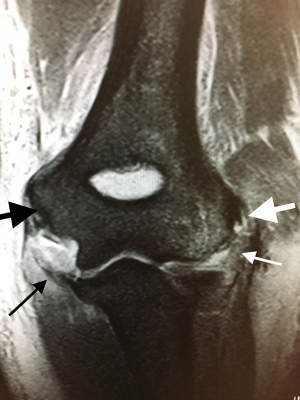
Standard anteroposterior and lateral radiographs are assessed to look for fractures and joint congruency. If there is a suspicion of a fracture, a computed tomography (CT) scan is the optimal imaging modality. Three dimensional (3D) reconstructions can be invaluable in understanding the pattern of injury particularly around the coronoid. Magnetic resonance imaging (MRI) scan can demonstrate integrity of the stabilising ligaments and tendons allowing stratification of simple elbow dislocations. When assessing an MRI scan it is important to assess the posterior and anterior bundles of MCL, flexor-pronator origin, LLC and common extensor origin. Ultrasound scanning can provide a dynamic examination of collateral ligaments and flexor and extensor tendons.
It is the practice of the senior author to reserve examination under anaesthesia (EUA) for simple dislocations with MRI proven soft tissue injury extending to the lateral structures or when there is clinical suspicion of high-grade soft tissue injury based on history of injury, degree of displacement, and clinical examination of soft tissue envelope. EUA involves an assessment of joint alignment under varus and valgus stress in full extension and 30 degrees of flexion, and in both pronation and supination. Re-dislocation under examination is indicative of gross instability. Mild and moderate instability are defined as less than or more than 10 degrees of joint opening respectively. Dynamic fluoroscopy has a role in delineating various grades of collateral ligament injuries and help with surgical decision-making (13,50,51).
PLRI and VPRI are clinical diagnoses. A careful history should include the position of the elbow at the time of injury if recalled. Radiographs and CT scans may reveal indirect signs of ligamentous injury such as calcification of ligaments and subluxation of the joint. Specific examination findings in PLRI may include a positive drawer and pivot shift test. Radiographs and CT imaging may reveal an avulsion fracture of the posterior aspect of capitellum (Osborne Cotterill lesion), and the drop sign (more than 4mm widening of ulnohumeral joint as seen on lateral radiograph) (52). An MRI scan will diagnose the ruptured LLC and also the presence of any osteochondral lesions.
Patients with VPRI will have positive posterolateral rotatory drawer test secondary to disruption of the LLC, which is avulsed from humeral condyle. AP radiographs show narrowing of the medial joint space, with a double crescent sign (distal displacement of medial contour of the coronoid appreciated on the lateral view radiograph) (47). Varus stress radiographs can be helpful to assess medial joint space collapse and lateral joint line widening. A CT scan with 3D reconstructions is particularly helpful in classifying any coronoid fracture but MRI best illustrates the soft tissue injury.
Patients with VEO typically present with painful throwing motion and reduced throwing velocity. A careful history can differentiate VEO from other sources of pain. Posterior elbow pain at ball release (elbow is in terminal extension) is the hallmark of VEO. By contrast, medial elbow pain at the onset of arm acceleration points to isolated MCL pathology, whereas posteromedial pain with resisted arm extension may be more likely due to triceps tendonitis.
The diagnostic test for VEO is valgus stress on the elbow at 20-30 degrees of flexion while forcing the elbow into terminal extension. This reproduces the pain over the posteromedial tip of the olecranon process experienced during throwing. Plain radiographs may show the presence of posteromedial olecranon osteophyte, olecranon stress fracture, or a loose body, however, the absence of these radiological signs does not eliminate VEO as impingement symptoms predate the formation of osteophytes and loose bodies. An MRI scan can evaluate the integrity of the MCL and show associated pathology such as loose bodies, olecranon stress fractures, and posteromedial olecranon tip osteophytes (41,53).
Treatment
Simple elbow dislocation
Stable simple elbow dislocation can be managed with early controlled mobilisation. Comparing early mobilisation (starting after 2 days) to plaster treatment, the functional outcomes, flexion-extension arc, return to work, and extension deficits have shown to be significantly improved following early mobilisation. There were no differences in pain, relapses, instability, and ossification in the two groups. Immobilization beyond three weeks had poorer outcomes (54-57).
Traditionally non-operative management was the standard treatment for simple dislocations. Josefsson et al. (29,58) showed no statistically significant difference in surgical versus non-surgical treatment of elbow dislocation but did not stratify by grade of injury. Both groups had extension deficits with full flexion, pro-supination, and no subjective instability or re-dislocation. Subjective instability has been reported in 8% of individuals (59) but Modi et al. reported only 2.3% of patients required stabilisation surgery at one year (60). Stratification of the extent of the injury with EUA, MRI, or US may identify those patients in whom all the soft tissue stabilisers have been stripped from the humerus and may benefit from early surgical stabilisation. The degree of instability is dependent on the extent of involvement of secondary dynamic stabilisers (2,51).
Surgical decision making in acute injuries relies on any of lateral joint line gapping, common extensor disruption, or EUA evidence of instability. Moderate instability is associated with poor function and a higher need for secondary revision surgery. Surgical stabilization is recommended for cases with moderate instability (51,61). Surgery aims to downgrade the level of injury and permit early mobilisation in the supine position in an attempt to avoid instability and stiffness. The acute repair involves open or arthroscopic repair of the lateral ligaments and common extensor origin. If instability persists following lateral ligament repair, an open repair of the medial ligament and CFO is undertaken (13).
Chronic instability
PLRI
Non-surgical management of established PLRI has a limited role as most functional activities put the elbow in the position of higher risk for instability and osteoarthritis. Anconeus and extensor muscles strengthening exercises may help in limiting mild PLRI (23,25). The primary aim of treatment is to restore and maintain articular congruity. Primary repair is the first line of treatment for ligament injuries that have occurred within six weeks. Daluiski et al. (62) found no difference in the range of movements and Mayo Elbow Performance Score (MEPS) in the acute versus delayed group respectively (<30 and >30 days). Sanchez-Sotelo et al. found better functional results and MEPS in the reconstruction group compared to the ligament repair group (63).
Grade 1 PLRI can be managed arthroscopically as described by Roger Van Riet (38). This technique consists of imbrication of the LUCL from the lateral epicondyle to the soft spot portal and then the supinator crest with the use of No 2 polydioxanone suture. The suture is then doubled and tails passed subcutaneously back to the soft spot portal and tied. Open repair of the Osborne Cotterill lesion can be performed using an all suture anchor in the posterior capitellum to restore the posterior capsular ligament.
LUCL reconstruction is preferred with an autograft, in cases of chronic instability. Allograft or synthetic grafts are used in patients with hypermobility syndrome.
VEO
Initial management in cases with isolated VEO with no MCL symptoms is with active rest followed by an interval throwing program and the gradual return to competition.
When conservative treatment fails, surgical treatments include arthroscopic posteromedial elbow decompression and +/− MCL reconstruction. The objective of arthroscopy is to assess the posterior surface of olecranon for osteophytes and any loose bodies. Posterior osteophytes should be removed with a shaver; however, excessive olecranon resection can lead to increased tensile forces across the MCL during valgus stress and lead to further valgus instability (64,65). Up to 8 mm of the olecranon can be resected safely without an increased strain on MCL (66). Eighty five percent of athletes are able to return to competitive sports after arthroscopic management (Reddy et al. arthroscopy 2000).
Formal reconstruction of MCL (Tommy Jones Procedure) involves open surgical procedure and is limited to the athlete who wishes to return to same level of competition and has failed conservative management (67).
Fracture dislocations
Unlike simple dislocations the presence of an associate fracture will normally mandate surgery. The Wrightington classification categorises these injuries and provides treatment algorithms based on the previously described three-column model of fracture dislocation instability (see algorithm, Figure 11).
Wrightington Type A
Type A fractures may result in a very small anteromedial facet fragment. Stability may be restored by fixing the lateral ligament only, but if instability persists bony fixation is mandatory. Repair of pMCL may be required if instability remains (Figure 7). Management of patients who develop VPRI, due to neglected injuries, ranges from non-operative management to LLC reconstruction and +/− reconstruction of the antermedial facet of the coronoid with a graft. Non-operative management is indicated in patients with no medial collapse of ulnohumeral joint space, no lateral gapping, and a firm endpoint in varus stress. Weekly radiographs are indicated for the first 3 weeks followed by another radiograph at 6 weeks interval to confirm maintenance of alignment and rule out any collapse. ROM exercises in the supine position are started early and progressive stretching is started at 6 weeks (38,48,68,69).
Surgery is recommended if subluxation or dislocation is seen, if the varus stress radiographs are positive, or clinical symptom of grinding or instability is observed when flexing the elbow in the horizontal plane with the shoulder abducted 90 degrees.
Surgical treatment aims to restore elbow kinematics with the aim of preventing chronic varus instability and the onset of early osteoarthritis. Conventional open approaches require extensive anterior capsular detachment to gain exposure and compromise vascularity and fixation. Arthroscopically assisted fixation allows for anatomic repair without extensive soft tissue dissection (70). This involves arthroscopic fixation of the coronoid fracture with a threaded 1.2 mm k-wire or cannulated screw from the dorsal surface of ulna into the coronoid. This can be facilitated by a tip aiming ACL guide. The pMCL repair is needed for cases with residual instability after LCL and anteromedial coronoid facet fixation (38,48).
Wrightington Type B
Bifacet fractures require fixation of the coronoid process usually with lag screws for single large fragments or plates where there is comminution. If the coronoid fracture is associated with a Monteggia fracture dislocation a plate should be applied to the ulna to restore the alignment of the olecranon and ulna diaphysis. Fixation of the coronoid should not be undertaken through the dorsal ulna plate as this compromises the coronoid fixation and risks recurrent instability (Figure 8). When bi-facet fractures occur in association with a radial head fracture, as part of a direct posterior injury or flexion type (apex posterior) Monteggia fracture dislocation the priority is to address the coronoid fracture which is aided by approaching the elbow through a lateral Kaplan approach (71) typically with a cannulated screw passed from the dorsum of the ulna across the fracture using the anterior trochlea as a “mould” to ensure adequate reduction. If the coronoid is fragmented a coronoid buttress plate can be inserted through a separate medial approach (Figure 9). Where the radial head is unsalvageable the coronoid is reduced and fixed prior to radial head replacement to ensure appropriate restoration of radial length. In Monteggia fracture dislocations the coronoid and radial head can be addressed through the ulna fracture via a posterior midline approach as described by McKee et al. (72). The lateral ligament is fixed once medial and lateral columns are restored (73).
Wrightington Type C (combined/comminuted radial head)
In type C fractures restoration of the radial head (lateral column), either by fixation or replacement, will restore stability without fixation of the anterolateral facet coronoid fracture (middle column) as long as the LLC injury is addressed (74,75). The MCL may need to be fixed if instability persists.
Wrightington D
Comminuted radial head fractures frequently require replacement and LLC repair. Where the radial head is intact the lateral ligament is frequently torn and needs to be repaired. In all cases, restoration of anatomical ulna alignment is important to ensure congruous articulation of the radial head with the capitellum, and to restore forearm biomechanics (Figure 10).
Rehabilitation protocol
Early elbow mobilisation has shown to have favourable outcomes (54-57). Splints, braces, plaster of paris, or external fixators can be avoided. Immediate mobilisation with a recumbent overhead regime has been described by Schreiber et al. (76). Above head exercises are performed whilst the patient is lying in a supine position with the shoulder flexed to 90, adducted and in neutral rotation. In this position the posteriorly directed forces are minimised by decreasing the effect of gravity and allowing the triceps to function as an elbow stabiliser. When biceps hypertonia had reduced, the patients then progress to open and closed chain functional exercises.
Conclusions
Elbow instability varies from simple dislocation with isolated soft tissue injury to fracture dislocation. Surgical intervention aims to restore stability to allow early range of movements. Understanding the pathoanatomy is vital for successful management of these injuries.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Spencer P. Lake) for the series “Emerging Trends in Elbow Injury, Pathology and Treatment” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-19-186). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kuhn MA, Ross G. Acute Elbow Dislocations. Orthop Clin North Am 2008;39:155-61. [Crossref] [PubMed]
- Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am 1984;66:927-30. [Crossref] [PubMed]
- Stoneback JW, Owens BD, Sykes J, et al. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am 2012;94:240-5. [Crossref] [PubMed]
- Regan WD, Korinek SL, Morrey BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop Relat Res 1991.170-9. [Crossref] [PubMed]
- O'Driscoll SW, Morrey BF, Korinek S, et al. Elbow subluxation and dislocation. A spectrum of instability. Clin Orthop Relat Res 1992.186-97. [PubMed]
- Ring D, Jupiter JB. Fracture-dislocation of the elbow. Hand Clin 2002;18:55-63. [Crossref] [PubMed]
- Fuss FK. The ulnar collateral ligament of the human elbow joint. Anatomy, function and biomechanics. J Anat 1991;175:203-12. [PubMed]
- Golan EJ, Shukla DR, Nasser P, et al. Isolated ligamentous injury can cause posteromedial elbow instability: a cadaveric study. J Shoulder Elbow Surg 2016;25:2019-24. [Crossref] [PubMed]
- Gluck MJ, Beck CM, Golan EJ, et al. Varus posteromedial rotatory instability: a biomechanical analysis of posterior bundle of the medial ulnar collateral ligament reconstruction. J Shoulder Elbow Surg 2018;27:1317-25. [Crossref] [PubMed]
- Edwards DS, Arshad MS, Luokkala T, et al. The contribution of the posterolateral capsule to elbow joint stability: a cadaveric biomechanical investigation. J Shoulder Elbow Surg 2018;27:1178-84. [Crossref] [PubMed]
- Miyasaka KC. Anatomy of the elbow. Orthop Clin North Am 1999;30:1-13. [Crossref] [PubMed]
- Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res 1991.187-95. [PubMed]
- Robinson PM, Griffiths E, Watts AC. Simple elbow dislocation. Shoulder Elbow 2017;9:195-204. [Crossref] [PubMed]
- Reichel LM, Milam GS, Hillin CD, et al. Osteology of the coronoid process with clinical correlation to coronoid fractures in terrible triad injuries. J Shoulder Elbow Surg 2013;22:323-8. [Crossref] [PubMed]
- Shin SH, Jeon IH, Kim HJ, et al. Articular surface area of the coronoid process and radial head in elbow extension: surface ratio in cadavers and a computed tomography study in vivo. J Hand Surg Am 2010;35:1120-5. [Crossref] [PubMed]
- Watts AC, Singh J, Elvey M, et al. Current concepts in elbow fracture dislocation. Shoulder Elbow 2019. [Crossref]
- Seiber K, Gupta R, McGarry MH, et al. The role of the elbow musculature, forearm rotation, and elbow flexion in elbow stability: an in vitro study. J Shoulder Elbow Surg 2009;18:260-8. [Crossref] [PubMed]
- Floris S, Olsen BS, Dalstra M, et al. The medial collateral ligament of the elbow joint: anatomy and kinematics. J Shoulder Elbow Surg 1998;7:345-51. [Crossref] [PubMed]
- Hwang J-T, Shields MN, Berglund LJ, et al. The role of the posterior bundle of the medial collateral ligament in posteromedial rotatory instability of the elbow. Bone Joint J 2018;100-B:1060-5. [Crossref] [PubMed]
- Olsen BS, Sojbjerg JO, Dalstra M, et al. Kinematics of the lateral ligamentous constraints of the elbow joint. J Shoulder Elbow Surg 1996;5:333-41. [Crossref] [PubMed]
- Safran MR, McGarry MH, Shin S, et al. Effects of elbow flexion and forearm rotation on valgus laxity of the elbow. J Bone Joint Surg Am 2005;87:2065-74. [Crossref] [PubMed]
- Park MC, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am 2004;86:2268-74. [Crossref] [PubMed]
- Buchanan TS, Delp SL, Solbeck JA. Muscular resistance to varus and valgus loads at the elbow. J Biomech Eng 1998;120:634-9. [Crossref] [PubMed]
- Pereira BP. Revisiting the anatomy and biomechanics of the anconeus muscle and its role in elbow stability. Ann Anat 2013;195:365-70. [Crossref] [PubMed]
- Gleason TF, Goldstein WM, Ray RD. The function of the anconeus muscle. Clin Orthop Relat Res 1985.147-8. [PubMed]
- Armstrong AD, Dunning CE, Faber KJ, et al. Rehabilitation of the medial col-lateral ligament-deficient elbow: an in vitro biomechanical study. J Hand Surg Am 2000;25:1051-7. [Crossref] [PubMed]
- Beingessner DM, Dunning CE, Stacpoole RA, et al. The effect of coronoid fractures on elbow kinematics and stability. Clin Biomech (Bristol, Avon) 2007;22:183-90. [Crossref] [PubMed]
- Dunning CE, Zarzour ZD, Patterson SD, et al. Muscle forces and pronation stabilize the lateral ligament deficient elbow. Clin Orthop Relat Res 2001.118-24. [Crossref] [PubMed]
- Josefsson PO, Gentz CF, Johnell O, et al. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am 1987;69:605-8. [Crossref] [PubMed]
- Josefsson PO, Johnell O, Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop Relat Res 1987.221-5. [Crossref] [PubMed]
- Luokkala T, Temperley D, Basu S, et al. Analysis of magnetic resonance imaging-confirmed soft tissue injury pattern in simple elbow dislocations. J Shoulder Elbow Surg 2019;28:341-8. [Crossref] [PubMed]
- Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand 1986;57:537-8. [Crossref] [PubMed]
- Linscheid RL, Wheeler DK. Elbow dislocations. JAMA 1965;194:1171-6. [Crossref] [PubMed]
- Schreiber JJ, Warren RF, Hotchkiss RN, et al. An online video investigation into the mechanism of elbow dislocation. J Hand Surg Am 2013;38:488-94. [Crossref] [PubMed]
- Cho CH, Kim BS, Rhyou IH, et al. Posteromedial Elbow Dislocations with-out Relevant Osseous Lesions: Clinical Characteristics, Soft-Tissue Injury Patterns, Treatments, and Outcomes. J Bone Joint Surg Am 2018;100:2066-72. [Crossref] [PubMed]
- O'Driscoll SW. Elbow instability. Acta Orthop Belg 1999;65:404-15. [PubMed]
- O'Driscoll SW, Jupiter JB, King GJ, et al. The unstable elbow. Instr Course Lect 2001;50:89-102. [PubMed]
- Tashjian RZ, Wolf BR, van Riet RP, et al. The Unstable Elbow: Current Concepts in Diagnosis and Treatment. Instr Course Lect 2016;65:55-82. [PubMed]
- Fleisig GS, Barrentine SW, Escamilla RF, et al. Biomechanics of overhand throwing with implications for injuries. Sports Med 1996;21:421-37. [Crossref] [PubMed]
- Aguinaldo AL, Chambers H. Correlation of throwing mechanics with elbow valgus load in adult baseball pitchers. Am J Sports Med 2009;37:2043-8. [Crossref] [PubMed]
- Dugas JR. Valgus extension overload: diagnosis and treatment. Clin Sports Med 2010;29:645-54. [Crossref] [PubMed]
- Wilson FD, Andrews JR, Blackburn TA, et al. Valgus extension overload in the pitching elbow. Am J Sports Med 1983;11:83-8. [Crossref] [PubMed]
- Eygendaal D, Safran MR. Postero-medial elbow problems in the adult athlete. Br J Sports Med 2006;40:430-4; discussion 434. [Crossref] [PubMed]
- King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop Relat Res 1969.116-23. [Crossref] [PubMed]
- O'Driscoll SW, Jupiter JB, Cohen MS, et al. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 2003;52:113-34. [PubMed]
- Ring D. Fractures of the Coronoid Process of the Ulna. The J Hand Surg Am 2006;31:1679-89. [Crossref] [PubMed]
- Sanchez-Sotelo J, O'Driscoll SW, Morrey BF. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow Surg 2005;14:60-4. [Crossref] [PubMed]
- Park SM, Lee JS, Jung JY, et al. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J Shoulder Elbow Surg 2015;24:74-82. [Crossref] [PubMed]
- Doornberg JN, Ring D. Coronoid Fracture Patterns. J Hand Surg Am 2006;31:45-52. [Crossref] [PubMed]
- Schnetzke M, Bergmann M, Wegmann K, et al. Determination of Elbow Laxi-ty in a Sequential Soft-Tissue Injury Model: A Cadaveric Study. J Bone Joint Surg Am 2018;100:564-71. [Crossref] [PubMed]
- Schnetzke M, Aytac S, Studier-Fischer S, et al. Initial joint stability affects the outcome after conservative treatment of simple elbow dislocations: a retrospective study. J Orthop Surg Res 2015;10:128-9. [Crossref] [PubMed]
- Coonrad RW, Roush TF, Major NM, et al. The drop sign, a radiographic warning sign of elbow instability. J Shoulder Elbow Surg 2005;14:312-7. [Crossref] [PubMed]
- Cain EL, Dugas JR, Wolf RS, et al. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med 2003;31:621-35. [Crossref] [PubMed]
- Iordens GI, Van Lieshout EM, Schep NW, et al. Early mobilisation versus plaster immobilisation of simple elbow dislocations: results of the FuncSiE multicentre randomised clinical trial. Br J Sports Med 2017;51:531-8. [Crossref] [PubMed]
- Maripuri SN, Debnath UK, Rao P, et al. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury 2007;38:1254-8. [Crossref] [PubMed]
- Rafai M, Largab A, Cohen D, et al. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases]. Chir Main 1999;18:272-8. [PubMed]
- Panteli M, Pountos I, Kanakaris NK, Tosounidis TH, Giannoudis PV. Cost analysis and outcomes of simple elbow dislocations. World J Orthop 2015;6:513-20. [Crossref] [PubMed]
- Josefsson PO, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment of ligamentous injuries following dislocations of the elbow joint. Clin Orthop Relat Res 1987.165-9. [Crossref] [PubMed]
- Anakwe RE, Middleton SD, Jenkins PJ, et al. Patient-reported outcomes after simple dislocation of the elbow. J Bone Joint Surg Am 2011;93:1220-6. [Crossref] [PubMed]
- Modi CS, Wasserstein D, Mayne IP, et al. The frequency and risk factors for subsequent surgery after a simple elbow dislocation. Injury 2015;46:1156-60. [Crossref] [PubMed]
- Schnetzke M, Aytac S, Keil H, et al. Unstable simple elbow dislocations: medium-term results after non-surgical and surgical treatment. Knee Surg Sports Traumatol Arthrosc 2017;25:2271-9. [Crossref] [PubMed]
- Daluiski A, Schrumpf MA, Schreiber JJ, et al. Direct repair for managing acute and chronic lateral ulnar collateral ligament disruptions. The J Hand Surg Am 2014;39:1125-9. [Crossref] [PubMed]
- Sanchez-Sotelo J, Morrey BF, O'Driscoll SW. Ligamentous repair and recon-struction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br 2005;87:54-61. [Crossref] [PubMed]
- Kamineni S, Hirahara H, Pomianowski S, et al. Partial posteromedial olecranon resection: a kinematic study. J Bone Joint Surg Am. 2003;85:1005-11. [Crossref] [PubMed]
- O'Driscoll SW, Morrey BF. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am 1992;74:84-94. [Crossref] [PubMed]
- Levin JS, Zheng N, Dugas J, et al. Posterior olecranon resection and ulnar collateral ligament strain. J Shoulder Elbow Surg 2004;13:66-71. [Crossref] [PubMed]
- O'Holleran JD, Altchek DW. The thrower's elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J 2006;2:83-93. [Crossref] [PubMed]
- Pollock JW, Brownhill J, Ferreira L, et al. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am 2009;91:1448-58. [Crossref] [PubMed]
- Pugh DM, Wild LM, Schemitsch EH, et al. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am 2004;86:1122-30. [Crossref] [PubMed]
- Rashid A, Copas D, Granville-Chapman J, et al. Arthroscopically-assisted fixation of anteromedial coronoid facet fracture and lateral ulnar collateral ligament repair for acute posteromedial rotatory fracture dislocation of the elbow. Shoulder Elbow 2019;11:378-83. [Crossref] [PubMed]
- Barnes LF, Lombardi J, Gardner TR, et al. Comparison of Exposure in the Kaplan Versus the Kocher Approach in the Treatment of Radial Head Fractures. Hand (N Y) 2019;14:253. [PubMed]
- McKee RC, McKee MD. Complex fractures of the proximal ulna: the critical importance of the coronoid fragment. Instr Course Lect 2012;61:227-33. [PubMed]
- Chan K, King GJ, Faber KJ. Treatment of complex elbow fracture-dislocations. Curr Rev Musculoskelet Med 2016;9:185-9. [Crossref] [PubMed]
- Hotchkiss RN. Displaced Fractures of the Radial Head: Internal Fixation or Excision? J Am Acad Orthop Surg 1997;5:1-10. [Crossref] [PubMed]
- Papatheodorou LK, Rubright JH, Heim KA, et al. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res 2014;472:2084-91. [Crossref] [PubMed]
- Schreiber JJ, Paul S, Hotchkiss RN, et al. Conservative management of elbow dislocations with an overhead motion protocol. J Hand Surg Am 2015;40:515-9. [Crossref] [PubMed]
Cite this article as: Singh J, Elvey MH, Hamoodi Z, Watts AC. Current perspectives on elbow dislocation and instability. Ann Joint 2021;6:10.


