
Reconstruction following periprosthetic joint infection: cemented or uncemented
Introduction
Periprosthetic joint infection (PJI) represents a devastating complication following total joint arthroplasty (TJA) for patients and surgeons alike. The incidence of PJI has been reported in 0.3–2.9% of patients following primary TJA procedures (1,2). The overall burden is expected to continue increase with an growing number of primary procedures being performed in our aging population (3). Two-stage revision remains the gold-standard for the treatment of PJI, with the primary goal of providing an infection-free and function joint for the patient.
While most surgeons have adopted the two-stage exchange arthroplasty treatment of PJI to include surgical debridement, explantation, and antibiotics, there remains some debate over the reconstruction method utilized at the time of definitive replantation. Components exist that take advantage of both cemented and cementless fixation techniques; however, there is no consensus on which fixation method is superior. This has resulted in a wide variety of reconstruction techniques employed at the second stage and can make interpretation of treatment success very difficult with the degree of heterogeneity present. The actual reconstruction method used is often overlooked, and it is difficult to know the significance it plays in the overall management of PJI. Therefore, the primary objective of this review is to discuss the reconstruction methods used at the time of replantation and whether this has any clinical significance in the successful management of infection.
Cemented prosthesis
Historically, cement is the most prevalent method of primary fixation in arthroplasty procedures. Until the more recent introduction of highly porous metals and press fit technology, cement was the predominant means of implant fixation. Cemented fixation has numerous proven and accepted benefits that have also been adopted in revision surgery and infection management.
First and foremost, cement is beneficial in the management of PJI as a local antibiotic delivery device. Once surgical debridement and implant resection is performed, high doses of antibiotics (often >4 g per 40 g bag of cement) are placed into temporary cement spacers to provide local delivery until replantation. However, medical and mechanical complications related to antibiotics cement have been reported at these higher levels (4). Many surgeons favor cemented fixation at the time of replantation to similarly allow for a local delivery of antibiotics at lower concentrations. Antibiotic supplementation of cement at concentrations less than 2 g per 40 g bag of cement allow for antibiotic delivery without significant detriment to the mechanical properties of the cement (5). This form of antibiotic delivery has been shown to be medically safe with no increased rate of systemic complications (6,7).
Cement is also frequently employed in the revision setting to help manage bone loss that is often not present at the time of the index procedure. (8). After extensive debridement with resection of diseased and infected bone, and prior instrumentation of the canals, there are greater areas of bone loss specifically in the articular and metaphyseal regions that require extended fixation into the diaphysis based on the zonal concept of fixation depicted in Figure 1 (9).
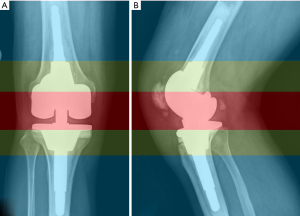
Several patient physiologic characteristics favor cemented fixation (9-11). These include poor diaphyseal bone stock and large canal diameter, and in patients with canal geometry that does not allow for adequate press fit. The use of cement in patients with poor bone stock helps to mitigate risk of iatrogenic fracture, perforation or stem pain. While most modern implants have slotted or fluted stem designs, larger diameter stems are known to be a risk factor fracture or stem pain, and patients who have weaker, osteoporotic bone may still have a modulus mismatch at the transition between the tip of the stem and their native bone. Patients with profound bowing in either the coronal or sagittal plane may not be candidates for diaphyseal press-fit stems that may perforate the cortex, even when using modern implants with a variety of stem offset options. This should be identified when templating on preoperative long leg alignment radiographs. Characteristics favoring cemented stem fixation are summarized in Table 1.
Table 1
| Revision total knee | Revision total hip |
|---|---|
| Poor diaphyseal bone | Poor diaphyseal bone |
| Large canal diameter | Large canal diameter |
| Abnormal distal femoral or proximal tibial bow | Abnormal proximal femoral bow |
| Sclerotic bone | Irradiated bone |
Cementless fixation
Cementless techniques have been increasingly adopted in primary hip and knee reconstruction; and as such, there has been increasing utilization in revision surgery and second stage reconstruction for PJI. In general, cementless fixation works by obtaining primary stability of the implants. Hoop stresses stabilize the implants enough to allow for early mobilization and weight bearing, while surface architecture allows for bony in-growth and on-growth for long term stability. Metaphyseal sleeves and cones can be added to increase fixation and fill bony voids.
Cementless fixation has been widely adopted in revision hip surgery to include infection management. The significantly enhanced survivorship with acetabular reconstruction has led to the use of cementless reconstruction even in patients with severe bone defects (12). Modular fluted tapered stems have also shown significantly improved survivorship when used in severe femoral bone defects with an intact diaphysis of less than 4 cm with the added benefit of increased flexibility to adjust length, offset and anteversion (13,14). Cementless fixation techniques in the knee are typically employed in a hybrid fashion, where cementless diaphyseal stems are utilized in conjunction with cemented articular fixation with or without the use of metaphyseal cones and sleeves.
Cementless fixation is preferred in patients with good diaphyseal bone stock and favorable osseous geometry (9-11). Patients with associated periprosthetic fracture also benefit from cementless fixation, as it allows the component to bypass the fracture site to achieve stability. Cementless fixation is also ideal in patients with sclerotic bone from pre-existing bone loss and instrumentation that would otherwise prohibit cement interdigitation. Patient factors favoring cementless stem fixation are summarized in Table 2.
Table 2
| Revision total knee | Revision total hip |
|---|---|
| Normal quality diaphyseal bone | Normal quality diaphyseal bone |
| Normal canal geometry that allows press fit | Normal canal geometry |
| Periprosthetic fracture | Periprosthetic proximal femoral fracture |
| Trochanteric osteotomy |
Hip specific outcomes after reimplantation
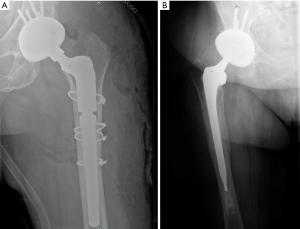
In revision hip surgery, there has been more widespread adoption of cementless fixation with a concomitant increase in utilization for primary hip surgery. It is well established that uncemented acetabular devices have a long track record of achieving reliable ingrowth and providing long-term component fixation in both the primary and revision setting (15,16). In femoral component fixation, initial design techniques evolved as an extension from primary cemented THA. However, early mechanical failure of cemented femoral components in aseptic revision reported in 1980s lead the development of extensively porous-coated, mono-block, cementless revision femoral stems that allowed for stable fixation into intact bone (17-19). These designs evolved into cylindrical stems and modern modular, fluted tapered stems that have shown high success even in the setting of severe bone defects as is shown in Figure 2A. The flexibility and modularity afforded by these types of implant systems help to address weaknesses inherent in cemented stem design (13,20). It can be very challenging to restore length and offset with a deficient or absent metaphyseal region, even with modular build-up or restoration of the calcar region. This has led to a diminished role for cement in revision total hip arthroplasty, including during reimplantation.
Utilizing this strategy, several authors have reported low 2-year re-infection rates following two-stage exchange arthroplasty with cementless fixation at reimlpantation (21-23). A study by Romano et al. prospectively followed a cohort of 19 patients with 20 infected total hip arthroplasties treated with two-stage revision and cementless reimplantation implants with only a single recurrent infection (23). Masri et al. retrospectively analyzed 29 PJI patients treated with two-stage exchange arthroplasty with final cementless components and reported a 10.3% re-infection rate. Of the 3 patients who got re-infected, one was able to be managed with intravenous antibiotic therapy alone, another was treated with irrigation and debridement followed by a course of antibiotics, and the third required resection arthroplasty (22). Kraay et al. evaluated 33 patients treated for infected THA with two-stage revision utilizing cementless fixation at reimplantation and found no re-infections in the 28 patients who reached 2 year follow-up (21).
Hybrid fixation, or cemented femoral components used with uncemented acetabular components similar to the construct shown in Figure 2B, may still play a role in select patients (24-27). Hybrid fixation in the aseptic revision setting has been shown to have 88–91% 10-year survival rate when used in patients who are older than 60 years of age, and those with lower baseline activity levels (24,26). Hybrid fixation may also have a role in select patients when one-stage revision is attempted for PJI treatment, in order to allow for more local delivery of antibiotics. This strategy should be reserved for patients with good local tissue, who are healthy hosts, and are known to be infected by low virulence organisms (28,29). Zahar et al. reported on 10-year outcomes in 85 hip PJI patients treated with one-stage exchange arthroplasty with hybrid component fixation. They reported a 10-year infection-free survival of 94% with 75.9% surgery free survival (29). Ilchmann et al. also reported their outcomes of 39 PJI hips in 38 patients who underwent one-stage exchange arthroplasty utilizing hybrid fixation (30). They reported no persistent, recurrent or new infection at minimum of 2 years.
Fully cemented fixation of the hip requires cementation of both the femoral and acetabular components. These reconstruction techniques have fallen out of favor with the widespread adoption of uncemented acetabular component fixation in revision total hip arthroplasty (15,16,31). Cementation does not provide biologic fixation, which increases the risk of long term mechanical failure. No series in literature exist that report on the outcomes of fully cemented component fixation at the time of reimplantation of infected THA.
Knee specific outcomes
There exists much greater heterogeneity and confusion regarding the management of knee reconstruction with regards to the use of cemented or cementless stems. The emergence of stem fixation in revision total knee arthroplasty has allowed for improved stability by off-loading the metaphyseal region where augmentation may otherwise be necessary. It also allows for dispersed stresses by increasing the bone-implant surface (32,33).
Unlike with hip replacement, the term “cementless” typically refers only to the choice of fixation strategy as it applies to the stems utilized in revision knee surgery. The method of fixation is not entirely cementless—surgeons who employ a “press-fit” or “cementless” technique are cementing the knee in a hybrid fashion where cement is applied to the articular and metaphyseal portions of the bone, which is then supported by long diaphyseal engaging stems. This type of construct is depicted in Figure 3A. These stems do not have a porous coating or any in-growth/on-growth potential. It is critical to engage at least 4 cm of the diaphysis to prevent early failure with this reconstruction technique (34).
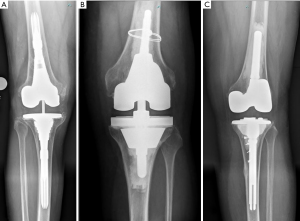
On the other hand, cemented stems enable the stress imparted by bone loss to be distributed along the entire length of the construct and can also support reconstructions that may require higher levels of constraint, as depicted in Figure 3B,C (35,36). Concerns regarding the durability of cemented fixation in revision knee surgery remain the same as in primary surgery. These concerns are magnified in patients who have large and even catastrophic bone loss that would typically fail without some form of reconstruction technique in the metaphyseal zone with highly porous metaphyseal cones or sleeves.
Benefits of hybrid fixation include reduced surgical time and ease in removal if subsequent revision is required. The literature demonstrates that this reconstruction technique is equivalent to cemented reconstructions for mild to moderate bone loss (34,37,38). Furthermore, because long stems engage the diaphysis, the overall mechanical alignment is improved when compared to cemented reconstructions in patients who do not have an anatomic bow (9).
Cementless stems may have lower rates of loosening than cemented stems in the setting of PJI. Edwards et al. retrospectively compared 102 cemented to 126 cementless following two-stage exchange total knee arthroplasty (37), and found cementless stems had a lower rate of radiographic loosening (17% in the cementless group vs. 32% in the cemented group P=0.006) with no difference in re-infection between the two groups. In contrast, Wang et al. performed a meta-analysis of 17 studies comparing cemented versus cementless stems in aseptic revision total knee arthroplasty and found no difference in failure from aseptic loosening or infection (11).
Conclusions
Fixation methods for definitive reconstruction following PJI remains a complex topic. In the hip, cementless fixation of the femoral component appears to provide increased stability and longevity; however, cement or hybrid fixation with a cemented femoral stem and cementless acetabular cup may still provide comparable results in select patient populations. For the reimplantation of infected total knee arthroplasty after two-stage exchange, cemented articular components remains the main mode of fixation, while cemented stems use depends on patient bone morphology and implant constraint. Higher quality comparative studies will remain challenging given the inherent complexity and heterogeneity of reimplantation after PJI. The plan for definitive fixation of implants should be individualized to address each patient’s unique demographic characteristics and osseous structures at the time of reimplantation.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Nemandra A Sandiford, Massimo Francescini and Daniel Kendoff) for the series “Prosthetic Joint Infection” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-74). The series “Prosthetic Joint Infection” was commissioned by the editorial office without any funding or sponsorship. AFC serves as an unpaid associate editor of Annals of Joint from June 2018 to May 2020. AFC reports personal fees from SLACK publishing, other from Joint Purification Systems, personal fees from Stryker, personal fees from bOne, other from Sonoran Biosciences, other from Graftworx, grants from OREF, personal fees from Pfizer, personal fees from Avanos, personal fees from Irrisept, personal fees from Convatec, personal fees from 3M, personal fees from Recro, personal fees from Heraeus, other from Hyalex, personal fees from DePuy - Ethicon, other from The Journal of Bone and Joint Surgery, personal fees from GLG, personal fees from UpToDate, outside the submitted work; and Editorial board: Journal of Arthroplasty; Annals of Joint; Bone and Joint 360 Journal; Clinical Orthopaedics and Related Research; Healthcare Transformation; Journal of Bone and Joint Infection; Knee Surgery, Sports Traumatology, Arthroscopy. Board/committee member: AAOS, AJRR, AAHKS, European Knee Association, International Congress for Joint Reconstruction, Musculoskeletal Infection Society. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Toulson C, Walcott-Sapp S, Hur J, et al. Treatment of infected total hip arthroplasty with a 2-stage reimplantation protocol: update on "our institution's" experience from 1989 to 2003. J Arthroplasty 2009;24:1051-60. [Crossref] [PubMed]
- Westrich GH, Walcott-Sapp S, Bornstein LJ, et al. Modern treatment of infected total knee arthroplasty with a 2-stage reimplantation protocol. J Arthroplasty 2010;25:1015-21, 1021.e1-2.
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Crossref] [PubMed]
- Edelstein AI, Okroj KT, Rogers T, et al. Nephrotoxicity After the Treatment of Periprosthetic Joint Infection With Antibiotic-Loaded Cement Spacers. J Arthroplasty 2018;33:2225-9. [Crossref] [PubMed]
- Duey RE, Chong AC, McQueen DA, et al. Mechanical properties and elution characteristics of polymethylmethacrylate bone cement impregnated with antibiotics for various surface area and volume constructs. Iowa Orthop J 2012;32:104-15. [PubMed]
- Berliner ZP, Mo AZ, Porter DA, et al. In-Hospital Acute Kidney Injury After TKA Revision With Placement of an Antibiotic Cement Spacer. J Arthroplasty 2018;33:S209-12. [Crossref] [PubMed]
- Iarikov D, Demian H, Rubin D, et al. Choice and doses of antibacterial agents for cement spacers in treatment of prosthetic joint infections: review of published studies. Clin Infect Dis 2012;55:1474-80. [Crossref] [PubMed]
- Mancuso F, Beltrame A, Colombo E, et al. Management of metaphyseal bone loss in revision knee arthroplasty. Acta Biomed 2017;88:98-111. [PubMed]
- Morgan-Jones R, Oussedik SI, Graichen H, et al. Zonal fixation in revision total knee arthroplasty. Bone Joint J 2015;97-B:147-9. [Crossref] [PubMed]
- Maggs J, Wilson M. The Relative Merits of Cemented and Uncemented Prostheses in Total Hip Arthroplasty. Indian J Orthop 2017;51:377-85. [Crossref] [PubMed]
- Wang C, Pfitzner T, von Roth P, et al. Fixation of stem in revision of total knee arthroplasty: cemented versus cementless-a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3200-11. [Crossref] [PubMed]
- Makita H, Kerboull M, Inaba Y, et al. Revision Total Hip Arthroplasty Using the Kerboull Acetabular Reinforcement Device and Structural Allograft for Severe Defects of the Acetabulum. J Arthroplasty 2017;32:3502-9. [Crossref] [PubMed]
- Abdel MP, Cottino U, Larson DR, et al. Modular Fluted Tapered Stems in Aseptic Revision Total Hip Arthroplasty. J Bone Joint Surg Am 2017;99:873-81. [Crossref] [PubMed]
- Kim YH, Park JW, Kim JS, et al. High Survivorship With Cementless Stems and Cortical Strut Allografts for Large Femoral Bone Defects in Revision THA. Clin Orthop Relat Res 2015;473:2990-3000. [Crossref] [PubMed]
- Morshed S, Bozic KJ, Ries MD, et al. Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop 2007;78:315-26. [Crossref] [PubMed]
- Yahiro MA, Gantenberg JB, Nelson R, et al. Comparison of the results of cemented, porous-ingrowth, and threaded acetabular cup fixation. A meta-analysis of the orthopaedic literature. J Arthroplasty 1995;10:339-50. [Crossref] [PubMed]
- Amstutz HC, Ma SM, Jinnah RH, et al. Revision of aseptic loose total hip arthroplasties. Clin Orthop Relat Res 1982;21-33. [Crossref] [PubMed]
- Kavanagh BF, Ilstrup DM, Fitzgerald RH Jr. Revision total hip arthroplasty. J Bone Joint Surg Am 1985;67:517-26. [Crossref] [PubMed]
- Pellicci PM, Wilson PD Jr, Sledge CB, et al. Long-term results of revision total hip replacement. A follow-up report. J Bone Joint Surg Am 1985;67:513-6. [Crossref] [PubMed]
- Huang Y, Zhou Y, Shao H, et al. What Is the Difference Between Modular and Nonmodular Tapered Fluted Titanium Stems in Revision Total Hip Arthroplasty. J Arthroplasty 2017;32:3108-13. [Crossref] [PubMed]
- Kraay MJ, Goldberg VM, Fitzgerald SJ, et al. Cementless two-staged total hip arthroplasty for deep periprosthetic infection. Clin Orthop Relat Res 2005;243-9. [Crossref] [PubMed]
- Masri BA, Panagiotopoulos KP, Greidanus NV, et al. Cementless two-stage exchange arthroplasty for infection after total hip arthroplasty. J Arthroplasty 2007;22:72-8. [Crossref] [PubMed]
- Romanò CL, Romano D, Meani E, et al. Two-stage revision surgery with preformed spacers and cementless implants for septic hip arthritis: a prospective, non-randomized cohort study. BMC Infect Dis 2011;11:129. [Crossref] [PubMed]
- Haydon CM, Mehin R, Burnett S, et al. Revision total hip arthroplasty with use of a cemented femoral component. Results at a mean of ten years. J Bone Joint Surg Am 2004;86:1179-85. [Crossref] [PubMed]
- Holt G, Hook S, Hubble M. Revision total hip arthroplasty: the femoral side using cemented implants. Int Orthop 2011;35:267-73. [Crossref] [PubMed]
- Ito H, Tanino H, Yamanaka Y, et al. Cemented calcar replacement femoral component in revision hybrid total hip arthroplasty. J Arthroplasty 2011;26:236-43. [Crossref] [PubMed]
- Nelson CL. Cemented femoral revision: technique and outcome. Am J Orthop (Belle Mead NJ) 2002;31:187-9. [PubMed]
- Haddad FS, Sukeik M, Alazzawi S. Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res 2015;473:8-14. [Crossref] [PubMed]
- Zahar A, Klaber I, Gerken AM, et al. Ten-Year Results Following One-Stage Septic Hip Exchange in the Management of Periprosthetic Joint Infection. J Arthroplasty 2019;34:1221-6. [Crossref] [PubMed]
- Ilchmann T, Zimmerli W, Ochsner PE, et al. One-stage revision of infected hip arthroplasty: outcome of 39 consecutive hips. Int Orthop 2016;40:913-8. [Crossref] [PubMed]
- Kim YH, Kim JS, Park JW, et al. Cementless revision for infected total hip replacements. J Bone Joint Surg Br 2011;93:19-26. [Crossref] [PubMed]
- Albrektsson BE, Ryd L, Carlsson LV, et al. The effect of a stem on the tibial component of knee arthroplasty. A roentgen stereophotogrammetric study of uncemented tibial components in the Freeman-Samuelson knee arthroplasty. J Bone Joint Surg Br 1990;72:252-8. [Crossref] [PubMed]
- van Loon CJ, Kyriazopoulos A, Verdonschot N, et al. The role of femoral stem extension in total knee arthroplasty. Clin Orthop Relat Res 2000;282-9. [Crossref] [PubMed]
- Gililland JM, Gaffney CJ, Odum SM, et al. Clinical & radiographic outcomes of cemented vs. diaphyseal engaging cementless stems in aseptic revision TKA. J Arthroplasty 2014;29:224-8. [Crossref] [PubMed]
- Moussa ME, Lee YY, Patel AR, et al. Clinical Outcomes Following the Use of Constrained Condylar Knees in Primary Total Knee Arthroplasty. J Arthroplasty 2017;32:1869-73. [Crossref] [PubMed]
- Yoshii I, Whiteside LA, Milliano MT, et al. The effect of central stem and stem length on micromovement of the tibial tray. J Arthroplasty 1992;7:433-8. [Crossref] [PubMed]
- Edwards PK, Fehring TK, Hamilton WG, et al. Are cementless stems more durable than cemented stems in two-stage revisions of infected total knee arthroplasties? Clin Orthop Relat Res 2014;472:206-11. [Crossref] [PubMed]
- Sinicrope BJ, Feher AW, Bhimani SJ, et al. Increased Survivorship of Cementless versus Cemented TKA in the Morbidly Obese. A Minimum 5-Year Follow-Up. J Arthroplasty 2019;34:309-14. [Crossref] [PubMed]
Cite this article as: Drayer NJ, Paik HK, Chen AF. Reconstruction following periprosthetic joint infection: cemented or uncemented. Ann Joint 2021;6:44.


