
Evaluation and management of patellar instability
Epidemiology and background
Patellar instability is a common clinical problem affecting between 6 and 23 per hundred thousand person-years with a higher incidence in females than males (1-4). The most predominantly affected group are adolescents between the ages of 14 and 18 years old (1,2). Patellofemoral instability is a multifactorial problem that can stem from a host of risk factors both demographic and anatomic. Demographic risk factors include young age, female sex, history of contralateral dislocation, and family history (5). Anatomic risk factors include trochlear dysplasia, elevated tibial tubercle to trochlear groove distance (TT-TG), patella alta, femoral and or tibial malalignment or rotational deformity, ligamentous laxity, and neuromuscular imbalance or control (6).
Recently, the risk of recurrence after a first time dislocation has been an area of research focus (4,7-12). Prediction models for first-time dislocators have concluded that there is a high-risk subset of young patients with trochlear dysplasia who have a much higher rate of recurrence than previously thought (4,11-13). The risk of recurrence after a first-time dislocation was previously documented as low as at 17%, however, this number was based on all-comers (4). More recent studies have demonstrated the risk of recurrence as high as 85% in high-risk subsets of the first-time dislocator group (13).
In addition to the pain and dysfunction caused by an instability event and the time away from sport required for recovery, with each dislocation, there is a significant risk of morbidity to the joint (14-16). In children and adolescents who sustained a first-time patellar dislocation, more than 90% will sustain an injury to the medial patellofemoral ligament (MPFL) (17), and greater than 90% will sustain some type of injury to their cartilage (14). The cartilage injury can vary from simple cracks and fissures to full-thickness cartilage defects and osteochondral fractures. These can be devastating injuries to the future health of the joint.
Current standard of care for first-time dislocators without a loose body or osteochondral fracture is nonoperative management (18). However, recent literature has demonstrated a high-risk population of patients with trochlear dysplasia who are under 25 years old at the time of their first dislocation. These risk factors predispose to an almost 70% risk of recurrence and as high as 85% in patients with a history of contralateral dislocation in addition to other anatomic risk factors (13). Given the young age of this high-risk population and increasing risk of cartilage damage with subsequent dislocation, there is a current focus in determining whether this high-risk group might be better treated with early surgical stabilization to prevent or reduce their risk of recurrent dislocation (6,7). While still controversial, there is growing evidence that a risk-stratified approach to surgical indications for the first time dislocator might be better than the one-size-fits-all model currently in use.
The two major questions we currently seek to answer in the field of patellar instability are (I) should we operate on a first time dislocator at high risk for recurrent dislocation and (II) what is the best surgical option for patients with recurrent dislocations? Is an MPFL alone enough for high-risk patients with several poor prognostic risk factors?
Clinical evaluation
Clinical evaluation should begin with a detailed history. This should include the patients age, skeletal maturity, sex, and activity level of the patient and any relevant family history. The clinician should determine if this was a first-time dislocation or a recurrent dislocation. In cases of recurrence, a detailed history of the first dislocation and any subsequent dislocations or subluxations, including age and mechanism of injury should be determined. It is very important to determine if this is an isolated instability problem or if pain is a substantial part of the chief complaint. This does not refer to pain associated with the instability events, but rather the clinician should seek to determine if there is daily or sports-related pain associated with weighted bent knee activities that would indicate overload and or malalignment in addition to the instability. If the patient is an athlete, it is important to understand what the patient’s expectations are with respect to returning to sport and how their seasonal timing may factor in so that the clinician can appropriately counsel the patient and their families (19).
A detailed physical exam begins with inspection and cartilage injury the patient standing alignment for any valgus or rotational deformities (19). Next, the Beighton scale is assessed, thumb to forearm, MCP hyperextension, elbow hyperextension, knee recurvatum, and palms to floor and a score out of 9 possible points is documented (20). All tests are scored bilaterally with the exception of palms to floor.
Next, in the seated position, a “J sign” is assessed while the patient flexes and extends their knee (21). This is done on both sides to compare the injured knee to the non-injured side. In the same seated position, crepitus is assessed with open chain knee extension to help focus the clinician’s attention to any potential underlying cartilage injuries. The patient is then asked to lie supine, and with the knee in extension, ballottement of the patella is performed to assess for effusion. Knee range of motion, including hyperextension, is assessed in the supine position and compared to the other knee. In the same position, hip range of motion including internal and external rotation is assessed.
Next, with the leg in full extension, the passive position of the patella is noted. In patients with passive patellar tilt, the clinician must assess whether or not the lateral structures are tight. This is done by maintaining the patella reduced in the trochlea and manually trying to evert the patella to neutral. If the clinician is unable to bring the patella parallel to the table then a tight lateral retinaculum is documented. An accurate assessment may not be possible as this maneuver may be too painful or uncomfortable for the patient, especially in those with a recent dislocation. For this reason, the ability to evert the patella to neutral and the tightness of the lateral retinaculum should also be performed prior to the start of each case as part of the exam under anesthesia in order to fully assess whether or not a lateral lengthening is a necessary part of the patellar stabilization surgery.
The patella is then translated both medially and laterally and quadrants of translation are assessed as well as the presence of any apprehension. Here, it is important to focus here on the presence of any medial apprehension in patients who have previously had surgery as often these patients are not aware that their symptoms are from medial subluxation. This can be seen in cases where an over-aggressive lateral release, over-tensioned MPFL, or overcorrection of a tibial tubercle has been performed.
In some cases, patients with chronic instability or significant ligamentous laxity do not demonstrate apprehension in full extension. In these instances, the moving patellar apprehension test can be useful and is most sensitive with the knee ranged from 0 to 45 degrees of flexion while lateral stress is placed on the patella (22). In addition to assessing quadrants of translation, the presence or absence of an endpoint to both medial and lateral translation should be documented.
Next, the patella should be palpated. We start by translating the patella laterally to unroof the lateral facet and then the lateral facet can be directly palpated to elicit tenderness. This is done for the inferior pole by applying a downward posteriorly directed pressure to the superior pole of the patella thus bringing the inferior pole anterior where it can be more readily palpated. The medial facet is also palpated for tenderness by translating the patella medially. In cases of acute dislocation, the area along the medial facet is an expected area of tenderness and can help to locate the site of injury or tear of the MPFL. Additionally, if there has been an injury to the cartilage the medial border of the patella at the insertion of the MPFL will be expectedly tender. The posterior superior aspect of the medial epicondyle at the sulcus where the MPFL originates is also palpated as this is the other common location for MPFL injury.
The patient is then asked to lie prone and hip range of motion can be assessed again in this position. Hip anteversion should also be checked in the prone position. This is done by flexing the knee to ninety degrees. The hip is then rotated internally and externally while palpating the greater trochanter. When the greater trochanter is brought parallel to the floor the position of the hip is assessed and documented. In addition, the thigh-foot axis is documented as this will help further guide the clinician to any rotational deformities that may be present.
Diagnostic imaging
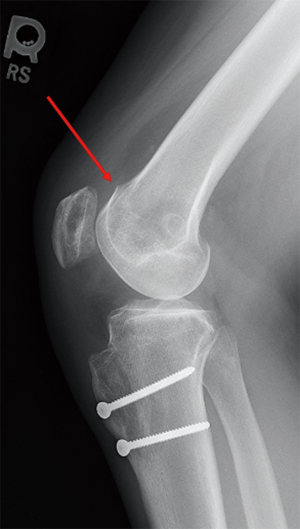
Standard radiographs include anteroposterior (AP) weight-bearing radiographs of both knees, posteroanterior (PA) weight-bearing radiographs with the knee at 45 degrees of flexion, true lateral radiograph and a bilateral Merchant view at 30 degrees of flexion. In addition to the above, full-length standing alignment views are helpful if there is any concern for coronal plane malalignment (19,23). The AP and PA flexion or tunnel views are most helpful to exclude tibiofemoral pathology. The lateral X-ray is best to identify trochlear dysplasia as can be evidenced by a supratrochlear bump and crossing sign (Figure 1). The merchant view is used to identify patellofemoral congruence, any joint space narrowing indicating chondral pathology, subluxation and tilt.
MRI is a critical diagnostic tool for any patient who has sustained a dislocation whether it is their first-time or a recurrence (24). Not only does MRI help to identify the dislocation event by the bone marrow edema pattern on the medial patella and lateral trochlea, but it is critical to identify any soft tissue ligament injury to the medial patellofemoral complex and, most importantly, presence and extent of chondral damage. In addition, MRI allows assessment of the TT-TG. This measurement was first identified and defined on CT scan but it has since been validated on MRI. It is important to note however, that MRI underestimates TT-TG by approximately 3 mm as compared to CT (25,26).
There is debate about the use of the TT-TG as a surgical indication for tibial tubercle transfers. Elevated TT-TGs are considered greater than 15 mm and some have used a TT-TG greater than 20 mm to indicate patients for the need for tibial tubercle transfers in addition to soft tissue stabilization (27,28).
Patellar height, classically defined on X-ray, is more accurately measured on MRI as the most useful patellar height classifications are mainly based on the articular length of the patella rather than the bony length. In addition to Caton-Deschamps index (CDI) and Blackburn Peel (BP), the patella trochlear index measured on MRI is a very useful assessment of patellar height (29,30). In cases of instability, surgeries that alter or move the tibial tubercle will affect the height ratios for the CDI and BP but these changes will not be reflected by the Insall-Salvati measurement (31).
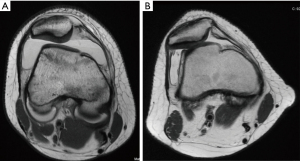
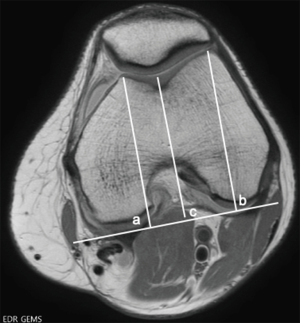
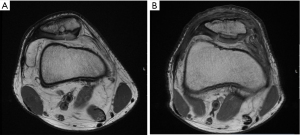
Classifications of trochlear dysplasia include the Dejour classification as described on both X-ray and MRI (Figure 2). This classification has demonstrated less inter-rater reliability and intra-rater reliability and as such, the authors favor using the trochlear depth index (TDI) (30,32). The TDI is measured by drawing a line parallel to the posterior femoral condyles on the axial slice that reflects the most posterior aspect of the condyles. The heights of the medial (a) and lateral (b) trochlear facets as well as the deepest aspect of the trochlea (c) are then measured with respect to this line. The TDI is then calculated using the equation [(a+b)/2−c] (Figure 3) (30,33). For normal knees and those with mild dysplasia, “a” was measured as the highest aspect of the medial condylar cartilage. For patients with severe dysplasia, the point where the cartilage ends on the medial aspect of the cliff is utilized for the medial height reference point. A TDI <3 mm can be considered dysplastic and has been shown to correlate with patellar instability (30,32,34).
The TT-PCL is preferred by some to measure coronal plane malalignment as both the tibial tubercle and the attachment of the PCL are tibial based and therefore do not cross the joint line and change with knee flexion or alignment, as is the criticism of the TT-TG (28). The TT-PCL was originally described by Seitlinger (35) and is the measure of the center of the patellar tendon attachment on the tibial tubercle to the distance of the center of the PCL attachment on the tibia. Normal ranges for the TT-PCL have been reported as 11.9±4.67 mm with a value of more than 20 mm considered pathologic (28). Several studies have demonstrated that TT-TG was more predictive of recurrent instability then TT-PCL (36,37) and TT-TG Remains the author’s preferred method for measurements of coronal plane dysplasia (28).
Given that patellar instability is clearly a multifactorial problem, it can be misguided to think that one risk factor would determine high rates of failure for isolated MPFL reconstruction. Instead, we believe there is a need for an Instability Severity Index Score (ISIS score) of the patella as we have previously seen utilized in the shoulder instability literature (38). This score will help to determine which patients will benefit from an isolated MPFL reconstruction versus which may have a higher failure rate and thus be better served with a combined MPFL reconstruction and bony realignment procedure. Current studies are underway to help create a Patella Instability Severity Index Score which we believe will help clinicians determine which patients should undergo boney realignment rather than using one measurement (i.e., TT-TG >20 mm) to determine this (10).
In addition to MRI and plain radiographs, CT can be useful to assess rotational deformities such as femoral anteversion or excessive tibial external rotation. This is done in cases where severe bony malalignment is suspected as a significant contributor to patellar instability. We do not use CT routinely to assess the knee or to calculate the TT-TG as we find MRI to be equally useful with the added benefit that it does not expose these young patients to unnecessary radiation.
Treatment
First-time dislocators
Historically the standard of care for patients with an acute patellar dislocation has been non-operative except for those with a concomitant loose body or osteochondral fracture requiring removal or fixation. However, as mentioned above, literature has clearly defined a high-risk subset of first-time dislocators who may benefit from early operative stabilization. This high-risk group includes patients under the age of 25 at the time of their first dislocation and trochlear dysplasia. The risk of re-dislocation goes up with additional risk factors such as a history of contralateral instability and anatomic risk factors such as elevated TT-TG and patella alta.
In addition to identifying patients at a high risk of recurrent instability, there have been several RCTs that have demonstrated significantly lower rates of re-dislocation and improved patient-reported outcomes in first-time dislocators treated with surgical stabilization versus those treated nonoperatively (39-41). In a study by Nwachukwu et al. (7) significantly greater rates of recurrence were found in skeletally immature patients treated nonoperatively compared with those who underwent surgical stabilization. In addition, patients undergoing surgery experienced significant improvements in function activity and quality of life compared to those treated nonoperatively (7).
Though further research is needed to clearly identify whether early operative intervention is the right treatment for high-risk first-time dislocators, it is clear that the one-size-fits-all approach is not appropriate. Risk stratified treatment for first-time dislocators will hopefully allow appropriate high-risk patients to undergo surgery early and prevent the long-term morbidity to cartilage seen with recurrent instability.
Current beliefs on surgeries for first-time dislocators are limited to medial sided reconstructions and repair. Though repair may be indicated in first-time dislocators, the author’s preferred method is reconstruction regardless of skeletal maturity due to the literature’s demonstration of superior outcomes (6,27). In skeletally immature patients, the MPFL is fixed below the growth plate which in most patients is at or very near the isometric point.
There are certainly patients who need bony realignment in addition to MPFL reconstruction even after a first-time dislocation. However, the literature is unclear on who these specific patients are and therefore, until we have more research in this area, the authors favor isolated soft-tissue surgery in first-time dislocators.
Recurrent dislocators
Based on higher recurrence rates, standard of care treatment for patients with recurrent instability is surgical stabilization. In this population, the important question becomes which type of surgery will best treat their recurrent instability. Much has been written about whether a MPFL reconstruction is enough. Based on literature available, we currently do not know which patients will benefit from an isolated MPFL reconstruction and which will have failure with recurrent instability and therefore be better stabilized with a concomitant bony realignment surgery.
As mentioned above, a patella-specific injury severity index score would be instrumental in helping to counsel our patients on whether they need a concomitant bony realignment procedure in addition to an MPFL reconstruction. Until we have this score, best practice supports isolated MPFL in patients without pain as a major source of their chief complaint, unloadable chondral injuries (inferior and/or lateral), and anatomic abnormalities, such as severe rotational deformities, valgus deformity, patella alta, or significantly elevated TT-TG. There is currently mixed data on the use of autograft vs. allograft and both have shown successful outcomes with decreased recurrence rates without clearly defining one as superior over the other (42,43). Overall recurrence of instability after MPFL reconstruction has been reported at less than 3% (44). Isolated MPFL reconstruction has been shown in multiple studies to be successful in reducing the risk of redislocation even in the presence of trochlear dysplasia (45,46).
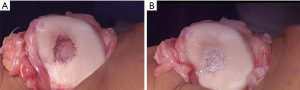
For recurrent dislocations that involve concomitant cartilage injury, we recommend addressing these lesions at the same time as their surgical stabilization. For patients with an isolated cartilage problem, this should be managed with either a one-stage or two-stage cell-based repair. In patients where the cartilage injury also involves the subchondral bone (subchondral architectural changes such as undulations, cysts and cavitation or bone loss) one must take, a structural approach that involves either an osteochondral autograft or allograft. However, it is important to note that subchondral edema does not necessarily indicate structural pathology within the subchondral bone that needs correction, and in appropriate situations, unloading this region will resolve the edema. For patellar lesions that have associated subchondral bone pathology, our preferred technique is osteochondral allograft utilizing a fresh patellar allograft due to the patella’s unique chondral topography and cartilage thickness which would be unmatched with an autograft (Figure 4), For contained lesions that do not have underlying structural bony pathology, our preferred technique is a one-staged approach utilizing particulated juvenile articular cartilage (PJAC) that is preformed using a small flexible mold created on the back table and which is then placed into the defect and gently shaped before sealing with fibrin glue (Figure 5).
In patients who have significant valgus that is believed to contribute to patellar instability, surgical options depend on skeletal maturity. For patients with adequate growth remaining, a simple guided growth or epiphysiodesis may be sufficient to correct the valgus deformity and this can be combined with an MPFL reconstruction during the same procedure. In skeletally mature patients, the correction must be performed through a distal femoral osteotomy and can be combined with a simultaneous MPFL reconstruction, as well as a tibial tubercle osteotomy (TTO) if needed. In cases of severe femoral anteversion, a derotational distal femoral osteotomy can laterally rotate the trochlea to help reduce the TT-TG and stabilize the patella. This can also be done at the same time as an MPFL reconstruction (with or without a concomitant TTO if indicated).
It is important to note that pain from malalignment and patella overload cannot be treated with an isolated MPFL reconstruction as this will only serve to stabilize the patella but not unload it. It is important to understand if the patient is complaining of chronic pain in addition to the instability, as this can only be addressed with an unloading tibial tubercle osteotomy.
Tibial tubercle osteotomy is a very versatile operation for patellar instability. It can reduce the TT-TG and the lateral vector on the patella by medializing the tubercle and simultaneously via an oblique osteotomy, the tubercle can be anteriorized to help unload the patellofemoral compartment decreasing pain or unloading cartilage injuries at the same time as addressing the coronal plane malalignment. In patients with severe alta, the tubercle can be distalized so that the patella engages in the trochlea earlier in flexion to help decrease the risk of dislocation. The acuity of the angle of the TTO can be flattened to obtain more medialization or made steeper to obtain more anteriorization based on the patient’s pathoanatomy.
Trochleoplasty has become more popular in the United States over the last five years as instrumentation has become available to make the procedure more guided, standardized, and hopefully safer for patients. Where past cuts were made completely freehand, current instrumentation exist to help protect the cartilage and guide the surgeon in the amount of bony resection. Even with the invention and implementation of newer instruments and guides, this procedure is intra-articular and immediately adjacent to the cartilage surface. Complications from trochleoplasty can include injury to the cartilage at the time of surgery and/or decreased viability of the cartilage as a late effect because of undermining the subchondral bone which provides nutrients and blood supply to the cartilage. Though there are some specific instances where trochleoplasty is indicated, some surgeons believe it to be a first-line surgery for patients with severe trochlear dysplasia. The authors prefer to reserve the use of trochleoplasty for severe failed cases of instability when a properly executed MPFL and TTO have failed. The concern is that generally, patellofemoral dysplasia is bipolar and not isolated to the trochlea alone but often involves patella dysplasia as well. Addressing only one side of the joint will often lead to more incongruity. If the joint can be stabilized via surgeries that are extra-articular and with lower risk, that is the best option for the patient. There is currently no evidence that trochleoplasty normalizes patellofemoral contact pressures and if done only for stabilization and not the long-term health of the joint, then we believe that other methods with lower complication rates and morbidities should be trialed first.
In summary, patellofemoral instability is a complex problem and current recommendations regarding the timing and type of surgical intervention are evolving. It is essential to identify whether the patient is presenting with pain, instability or a combination of both, as the best treatment for these pathologies varies significantly. Current research is ongoing with the goal of understanding and clarifying which subgroup of first time dislocators should be managed operatively as well as which subset of recurrent dislocators require concomitant bony realignment procedures. This research is paramount to our ability to provide the best care for patients with patellar instability. Please find a supplemental Q&A between the authors and editors in Appendix 1.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Sommer Hammoud and Robin V. West) for the series “Sports Related Injuries of the Female Athlete” published in Annals of Joint. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-2020-02). The series “Sports Related Injuries of the Female Athlete” was commissioned by the editorial office without any funding or sponsorship. BESS reports personal fees from Arthrex, outside the submitted work. In addition, a member of her family receives royalties from Arthrex, outside of the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sanders TL, Pareek A, Hewett TE, et al. Incidence of First-Time Lateral Patellar Dislocation: A 21-Year Population-Based Study. Sports Health 2018;10:146-51. [Crossref] [PubMed]
- Waterman BR, Belmont PJ, Owens BD. Patellar Dislocation in the United States: Role of Sex, Age, Race, and Athletic Participation. J Knee Surg 2012;25:51-7. [Crossref] [PubMed]
- Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: Incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-5. [Crossref] [PubMed]
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [Crossref] [PubMed]
- Redler LH, Meyers KN, Brady JM, et al. Anisometry of Medial Patellofemoral Ligament Reconstruction in the Setting of Increased Tibial Tubercle-Trochlear Groove Distance and Patella Alta. Arthroscopy 2018;34:502-10. [Crossref] [PubMed]
- Shubin Stein BE, Gruber S, Brady JM. MPFL in First-Time Dislocators. Curr Rev Musculoskelet Med 2018;11:182-7. [Crossref] [PubMed]
- Nwachukwu BU, So C, Schairer WW, et al. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:760-7. [Crossref] [PubMed]
- Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: A randomized clinical trial. J Bone Joint Surg Am 2008;90:463-70. [Crossref] [PubMed]
- Garth WP Jr, DiChristina DG, Holt G. Delayed proximal repair and distal realignment after patellar dislocation. Clin Orthop Relat Res 2000;132-44. [Crossref] [PubMed]
- Erickson BJ, Mascarenhas R, Sayegh ET, et al. Does operative treatment of first-time patellar dislocations lead to increased patellofemoral stability? A systematic review of overlapping meta-analyses. Arthroscopy 2015;31:1207-15. [Crossref] [PubMed]
- Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575-81. [Crossref] [PubMed]
- Lewallen L, McIntosh A, Dahm D. First-Time Patellofemoral Dislocation: Risk Factors for Recurrent Instability. J Knee Surg 2015;28:303-9. [Crossref] [PubMed]
- Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop 2017;37:484-90. [Crossref] [PubMed]
- Nomura E, Inoue M. Cartilage Lesions of the Patella in Recurrent Patellar Dislocation. Am J Sports Med 2004;32:498-502. [Crossref] [PubMed]
- Stanitski CL, Paletta GA. Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med 1998;26:52-5. [Crossref] [PubMed]
- Franzone JM, Vitale MA, Shubin Stein BE, et al. Is there an association between chronicity of patellar instability and patellofemoral cartilage lesions? An arthroscopic assessment of chondral injury. J Knee Surg 2012;25:411-6. [Crossref] [PubMed]
- Askenberger M, Arendt EA, Ekström W, et al. Medial Patellofemoral Ligament Injuries in Children with First-Time Lateral Patellar Dislocations. Am J Sports Med 2016;44:152-8. [Crossref] [PubMed]
- Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar Instability Management: A Survey of the International Patellofemoral Study Group. Am J Sports Med 2018;46:3299-306. [Crossref] [PubMed]
- Weber AE, Nathani A, Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am 2016;98:417-27. [Crossref] [PubMed]
- Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis 1973;32:413-8. [Crossref] [PubMed]
- Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy 1999;15:841-51. [Crossref] [PubMed]
- Ahmad CS, McCarthy M, Gomez JA, et al. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med 2009;37:791-6. [Crossref] [PubMed]
- Merchant AC. Patellofemoral imaging. Clin Orthop Relat Res 2001;15-21. [Crossref] [PubMed]
- Sanders TG, Morrison WB, Singleton BA, et al. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr 2001;25:957-62. [Crossref] [PubMed]
- Schoettle PB, Zanetti M, Seifert B, et al. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 2006;13:26-31. [Crossref] [PubMed]
- Camp CL, Stuart MJ, Krych AJ, et al. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med 2013;41:1835-40. [Crossref] [PubMed]
- Erickson BJ, Nguyen J, Gasik K, et al. Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability Regardless of Tibial Tubercle-Trochlear Groove Distance and Patellar Height: Outcomes at 1 and 2 Years. Am J Sports Med 2019;47:1331-7. [Crossref] [PubMed]
- Brady JM, Rosencrans AS, Shubin Stein BE. Use of TT-PCL versus TT-TG. Curr Rev Musculoskelet Med 2018;11:261-5. [Crossref] [PubMed]
- Biedert RM, Albrecht S. The patellotrochlear index: A new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc 2006;14:707-12. [Crossref] [PubMed]
- Askenberger M, Janarv PM, Finnbogason T, et al. Morphology and Anatomic Patellar Instability Risk Factors in First-Time Traumatic Lateral Patellar Dislocations. Am J Sports Med 2017;45:50-8. [Crossref] [PubMed]
- Middleton KK, Gruber S, Shubin Stein BE. Why and Where to Move the Tibial Tubercle: Indications and Techniques for Tibial Tubercle Osteotomy. Sports Med Arthrosc Rev 2019;27:154-60. [Crossref] [PubMed]
- Pfirrmann CWA, Zanetti M, Romero J, et al. Femoral trochlear dysplasia: MR findings. Radiology 2000;216:858-64. [Crossref] [PubMed]
- Stepanovich M, Bomar JD, Pennock AT. Are the Current Classifications and Radiographic Measurements for Trochlear Dysplasia Appropriate in the Skeletally Immature Patient? Orthop J Sports Med 2016;4:2325967116669490. [Crossref] [PubMed]
- Skelley N, Friedman M, McGinnis M, et al. Inter- and intraobserver reliability in the MRI measurement of the tibial tubercle-trochlear groove distance and trochlea dysplasia. Am J Sports Med 2015;43:873-8. [Crossref] [PubMed]
- Seitlinger G, Scheurecker G, Högler R, et al. Tibial tubercle-posterior cruciate ligament distance: A new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 2012;40:1119-25. [Crossref] [PubMed]
- Camp CL, Heidenreich MJ, Dahm DL, et al. Individualizing the Tibial Tubercle-Trochlear Groove Distance: Patellar Instability Ratios That Predict Recurrent Instability. Am J Sports Med 2016;44:393-9. [Crossref] [PubMed]
- Brady JM, Sullivan JP, Nguyen J, et al. The Tibial Tubercle-to-Trochlear Groove Distance Is Reliable in the Setting of Trochlear Dysplasia, and Superior to the Tibial Tubercle-to-Posterior Cruciate Ligament Distance When Evaluating Coronal Malalignment in Patellofemoral Instability. Arthroscopy 2017;33:2026-34. [Crossref] [PubMed]
- Balg F, Boileau P. The instability severity index score: A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7. [Crossref] [PubMed]
- Sillanpää PJ, Mäenpää HM. First-time patellar dislocation: Surgery or conservative treatment? Sports Med Arthrosc Rev 2012;20:128-35. [Crossref] [PubMed]
- Camanho GL, Viegas Ade C, Bitar AC, et al. Conservative Versus Surgical Treatment for Repair of the Medial Patellofemoral Ligament in Acute Dislocations of the Patella. Arthroscopy 2009;25:620-5. [Crossref] [PubMed]
- Bitar AC, D’Elia CO, Demange MK, et al. Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop 2015;46:675-83. [Crossref] [PubMed]
- McNeilan RJ, Everhart JS, Mescher PK, et al. Graft Choice in Isolated Medial Patellofemoral Ligament Reconstruction: A Systematic Review With Meta-analysis of Rates of Recurrent Instability and Patient-Reported Outcomes for Autograft, Allograft, and Synthetic Options. Arthroscopy 2018;34:1340-54. [Crossref] [PubMed]
- Hendawi T, Godshaw B, Flowers C, et al. Autograft vs allograft comparison in pediatric medial patellofemoral ligament reconstruction. Ochsner J 2019;19:96-101. [Crossref] [PubMed]
- Schneider DK, Grawe B, Magnussen RA, et al. Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for the Treatment of Recurrent Lateral Patellar Dislocations: A Systematic Review and Meta-analysis. Am J Sports Med 2016;44:2993-3005. [Crossref] [PubMed]
- Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med 2006;34:1254-61. [Crossref] [PubMed]
- Liu JN, Brady JM, Kalbian IL, et al. Clinical Outcomes After Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability Among Patients With Trochlear Dysplasia. Am J Sports Med 2018;46:883-9. [Crossref] [PubMed]
Cite this article as: Dennis ER, Gruber S, Marmor WA, Shubin Stein BE. Evaluation and management of patellar instability. Ann Joint 2022;7:2.


