Arthroscopic management of the nonunion avulsion fracture of ischial tuberosity for a teenager dancer: a case report
Introduction
The ischial tuberosity (IT) serves as the origin of the hamstring muscles (long head of the biceps femoris, the semitendinosus, and the semimembranosus muscle) (1,2). The avulsion fracture of IT is very rare and typically occurs in younger athletes or competitive players (1,3). A study of 228 pelvic apophyseal avulsion fractures (25 patients with IT avulsion fractures) found that almost IT patients are around 14 years old, before the closure of the apophysis with the ischium (4). As a rare variant of proximal hamstring injuries, the clinical presentations of IT avulsion fractures are similar to symptoms associated with hamstring strains, which can cause an incorrect diagnosis during the initial visit. Unfortunately, misdiagnosis and inappropriate management can mislead a strictly restricted activity in the early stage, which may increase the risk of fractures displacement and a painful nonunion (5).
Owing to the demands of the high sports of these young patients, operative intervention should be considered once displacement exceeds 15 mm (1). Several operative techniques for the avulsion fractures of IT are reported. Open reduction and internal screw fixation or plate fixation should be chosen in the early stage in consideration of the possibility of fracture healing (1,6). And for the delayed or nonunion cases, resection of the IT fragment and hamstring reattachment is the most commonly used technique (3,7). The fracture displacement and formation of pseudoarthrosis may disturb the sciatic nerve and cause radiating pain in some patients, who required an additional operation for neurolysis and scar debridement (3,8). Recently, several minimally invasive techniques have been introduced to IT avulsion fractures, like platelet-rich plasma (PRP) injections or percutaneous needle fenestration (9,10). And these techniques have achieved promising results in the early follow-up.
With enhanced understanding and improvement in hip arthroscopy, the indications of this technique have been extended from original intraarticular pathologies to peri-articular hip disorders, like greater trochanteric pain syndrome, internal hip snapping, extra-articular impingement or proximal hamstring injuries (11). Given its minimally invasive and fine operation, endoscopy can be an option, as well as an alternative to open procedures for injuries around IT. Arthroscopic has the advantage of faster recovery, reduced stiffness, and improved cosmesis when compared with open surgery. Although some surgeons used endoscopy techniques to perform the repairing and reattachment of hamstring tendons, there is no report of hip arthroscopy for IT avulsion fractures in the literature.
This is the first time that the arthroscopic technique has been introduced to treat a nonunion avulsion fracture of the IT. All experiences based on this case, including positioning, approach, intraoperative IT targeting, manipulation, and tendon fixation and a brief discussion will be present. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/aoj-20-122).
Case presentation
A 19-year-old male dancer complained of intermittent dull pain of left buttock over 5 years after a strain. His initial injury occurred acutely in his training to stretch hamstring muscle when he was a 14-year-old dance student. Just at that moment, he was feeling a sense of tearing and pain. But he could walk without any activity limitations of left hip, which misled his school hospital, the first visiting, to put forward an incomplete diagnose of muscle strain and give him a little external painkiller. After two weeks of rest, he was back to dancing with an intermittent dull pain of left buttock. After sitting for a long time, he felt worse pain in his buttocks. In the past five years, he had tried physical therapy and local block, but there was no obvious relief of pain. Gradually, the pain bothered him to do some dance movements involving the back extension of the left hip (Figure 1).
Physical examination revealed mild muscle atrophy from the left buttocks down to the back of the thigh. The left ischial tubercle was larger, bulged and moved down compared with the contralateral tubercle. There was tenderness around the left ischial tubercle but no radiation pain of lower limbs. The range of motion in the left hip was normal, but the strength of hip extension and knee flexion was slightly weaker than that of the right side.
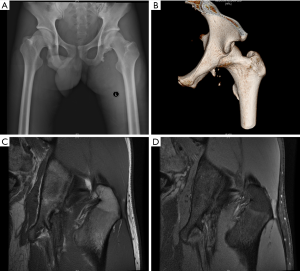
The X-ray and CT scan revealed an obvious group of fractured bone fragments along the outer part of the ischial tubercle, and the biggest one piece of fracture fragments was about 4×2×1.3 cm3 (Figure 2A,B). There was a gap between the fracture fragments and the ischial tubercle, which was filled with scar tissues revealed by magnetic resonance imaging (MRI) (Figure 2C). The narrowing of the ischiofemoral space (IFS) was also observed, which may cause pain in the left hip. There was no abnormality in the laboratory test.

Surgical procedure
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
With general anesthesia, the patient was placed in a prone position. Firstly, we located and marked the sciatic nerve and bone structure by ultrasound, which helps us to identify the fractured mass and avoid neurovascular structures during portal placement (Figure 3). We also marked four pilot portals under the guidance of ultrasound (Figure 3).

In order to prevent pollution, we used a cotton pad to protect the perineum and then sealed this region with a protective membrane. And we completely disinfected the operative area with indoor. The procedure begins with fluoroscopic localization of the inner lower (IL) portal. Under fluoroscopic guidance, the direction of puncture is directed at approximately 30 degrees cranially and 20 degrees laterally to the gap between the fracture fragments and the ischial tubercle. The positioning of the other portals around the fracture fragments is facilitated by viewing of a 30° arthroscope through this portal. We used a shaver and radiofrequency to clears the subgluteal space of scar tissue and exposure of bone block and attached tendons. Then we continued debridement further to show the gap between the fracture fragments and the ischial tubercle, which was the pseudoarthrosis. A 5.5-mm burr was used to grind off the bone mass after exposing the whole fracture mass and its relationship with ischial tubercle. The footprint of hamstring tendons on ischial tubercle was cleared of soft tissue and burred to augment the healing of the tendons. Under arthroscopic monitoring, we adjusted the fixation position to obtain a good tension of these tendons. At last, this group of tendons was fixed to its insertion by two absorbable anchors (Smith & Nephew, Andover, MA) under assistance to maintain the reduction of the tendon (Figure 4).

Postoperative rehabilitation
Rehabilitation is done in phases, and it is paramount to progress at a gradual pace to avoid inflammatory flares, which may prolong the recovery process. At first 3 weeks postoperatively, the ankle pump, quadriceps, and knee joint muscle isometric contraction exercises were allowed to perform. At this time, the open kinetic chain exercises of the left hip, especially flexion, was avoided. The patient began passive range-of-motion exercises in the painless range from 4 weeks after the operation. Partial weight-bearing was performed 2 months after surgery, while continuing passive and active hip movement within the tolerable range was performed, including adduction, abduction, and pronation. After 3 months, patients could walk with full weight and resume normal functional activities of lower limbs. Patients gradually returned to normal activities and tried to take a walk, jogging and other physical activities 6 months after the operation. Then the patient gradually returned to dancing exercises.
Results
With this arthroscopic surgery, we successfully removed the nonunion bone mass, which may reduce the ischiofemoral impingement. As we expected, the removal of the bone mass eased the pain significantly (Figure 5A,B). At 2 months postoperatively, this young patient could finish partial weight-bearing activities without pain. Moreover, the avulsed hamstring tendons were re-attached with sufficient tension to the insertion on the IT. At 6 months, the follow-up MRI showed good healing of reattached tendons (Figure 5C,D). The strength of hip extension increased significantly after he gradually returned to training. The dancer was very satisfied with the relief of pain and the recovery of activity strength. He also successfully returned to dance training. For this uncommon and delayed case, arthroscopy can be introduced into its operative management as a minimally invasive and effective technique
Discussion
The avulsion fracture of IT is very rare and typically occurs in younger athletes or competitive players. The clinical presentations of IT avulsion fracture are similar to symptoms associated with hamstring strains, which can lead to a misdiagnosis during the initial visit. Unfortunately, misdiagnosis and delayed treatment can cause a nonunion or pseudoarthrosis at the avulsion site, which annoyed the patients a lot. Gidwani et al. (5) presented a case series of 12 patients with IT avulsion fractures, in which 66.7% (8/12) patients had a misdiagnosis and subsequently a delayed therapy for 5 to 12 months. And these patients suffered residual pain or other symptoms and required a surgical treatment at last. Some patients without timely management also complained of a pain radiating down to the back of the thigh, which was caused by irritation of the sciatic nerve within circumjacent scar tissues. Prolonged sitting or some stretching movements can aggravate the pain, which may require sciatic neurolysis during the surgeries (6,12).
In this report, the young patient suffered an initial injury five years ago. After misdiagnosis, there was an intermittent dull pain in his left buttock symptoms, especially when he performed back extension of the left hip. But the pain did not radiate to other body regions. The imaging examination showed a narrowing space between IT and lesser trochanter, which implied ischiofemoral impingement. In literatures, it has been reported that patients with symptomatic ischiofemoral impingement have a significantly narrower IFS than asymptomatic patients (13,14). And the normality threshold of IFS is still nonconsensus and commonly suggested as measurements of 15 mm (15), taking in the degree of hip rotation, abduction, and extension at which the images are acquired (16). In our case report, the images showed an extremely shorter IFS of 9.56 mm, which was caused by the displacement of the ischial tubercle after avulsion. The IFS was widened to >30 mm after removing the nonunion avulsion fracture of IT under arthroscopy. The pain of this young dancer was completely relieved as well at 6 weeks postoperatively. This is the first time that the arthroscopic technique has been successfully introduced to treat nonunion avulsion fracture of IT. However, more clinical studies are needed to further validate the efficacy of arthroscopy.
The displacement of IT after avulsion fracture also descended the insertion of hamstring tendons, which caused a declined tension and strength of the hamstring muscle group. For this young man, we decided to reattach the tendons back to restore the strength using reported techniques (17,18), which required debridement of IT and reattachment with suture anchors. However, the huge bony avulsions and pseudojoint made this case a unique challenge, especially under arthroscopy. Although some authors reported open surgical treatments for IT avulsion fractures and with a good outcome in the majority of cases at short-term follow-up, but only five patients (50%) rated their hip as normal there are no arthroscopic techniques in the literature for reference. And we summarized several key points from this case: (I) clean up scar tissues to provide a good vision under endoscopy; (II) locate the sciatic nerve and fracture block using ultrasound to help the intraoperative localization; (III) outline the position of pseudojoint to determine the range of the burring of bony fractures; (IV) debride the footprint of tendons deep to cancellous bone; (V) test the tension of tendons to determine anchor locations. At 6 months postoperatively, the MRI showed good healing of hamstring tendons with IT (Figure 5C,D), which is consistent with the literature (19).
Proper postoperative rehabilitation is a key component in the successful management of this rare case. Misdiagnose and delayed treatment for 5 years caused the displacement of bony avulsion and hamstring contraction, which increased the risk of anchor failure and the difficulty of healing. The rehabilitation course was extended according to previous reports (17,18). In a report of IT avulsion of three young athletes, Biedert (20) used biodegradable suture anchors to repair the avulsed fragment and attached tendons via open surgery. During anesthesia recovery, one patient experienced an excessive muscle contraction, which caused loosening of the sutures and a revision operation to repeated refixation of the avulsed fragment. Therefore, the mobilization and limitations of active movements, especially flexion, are necessary for the early stage of rehabilitation course. And we suggested a postoperative regimen of passive range-of-motion exercises in the painless range from 4 weeks, followed by partial weight-bearing and walk with full weight at 4 months. Gradually return to dancing exercises was expected from 6 months postoperatively. Given the scarcity and the incoherence of research for IT avulsion fractures, the management of rehabilitation still is a challenging and require more continuous clinical studies.
Conclusions
The avulsion fractures of IT are uncommon and relatively specific in children or teenager. Without proper imaging and/or clinical suspicion, this injury can be mismanaged and cause nonunion or displacement of the bony avulsion, which may require surgery. In this article, we reported a 19-year-old male dancer with nonunion avulsion fractures of the IT, which was missed initially and delayed for 5 years. Plain radiograph should be done if patients had buttock pain. MRI is recommended when sciatic nerve symptoms exist. CT is recommended in patients with surgical indications. Under hip arthroscopy, we removed the nonunion bone and repaired the insertion of the hamstring tendon. The patient was satisfied and returned to sports within 6 months. Although there is only one patient, this is the first time that the arthroscopic technique has been successfully introduced to treat this unusual injury, which may be a pilot reference for the management of IT avulsion fractures.
Acknowledgments
Funding: The work was supported by the National Natural Science Foundation of China (81902205).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/aoj-20-122
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoj-20-122). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlic PW, Sadoghi P, Singer G, et al. Treatment for ischial tuberosity avulsion fractures in adolescent athletes. Knee Surg Sports Traumatol Arthrosc 2014;22:893-7. [Crossref] [PubMed]
- Schiller J, DeFroda S, Blood T. Lower Extremity Avulsion Fractures in the Pediatric and Adolescent Athlete. J Am Acad Orthop Surg 2017;25:251-9. [Crossref] [PubMed]
- Spencer-Gardner L, Bedi A, Stuart MJ, et al. Ischiofemoral impingement and hamstring dysfunction as a potential pain generator after ischial tuberosity apophyseal fracture non-union/malunion. Knee Surg Sports Traumatol Arthrosc 2017;25:55-61. [Crossref] [PubMed]
- Schuett DJ, Bomar JD, Pennock AT. Pelvic Apophyseal Avulsion Fractures: A Retrospective Review of 228 Cases. J Pediatr Orthop 2015;35:617-23. [Crossref] [PubMed]
- Gidwani S, Bircher MD. Avulsion Injuries of the Hamstring Origin – A Series of 12 Patients and Management Algorithm. Ann R Coll Surg Engl 2007;89:394-9. [Crossref] [PubMed]
- Gidwani S, Jagiello J, Bircher M. Avulsion fracture of the ischial tuberosity in adolescents - An easily missed diagnosis. BMJ 2004;329:99-100. [Crossref] [PubMed]
- Kaneyama S, Yoshida K, Matsushima S, et al. A Surgical Approach for an Avulsion Fracture of the Ischial Tuberosity. J Orthop Trauma 2006;20:363-5. [Crossref] [PubMed]
- Spinner RJ, Atkinson JLD, Wenger DE, et al. Tardy sciatic nerve palsy following apophyseal avulsion fracture of the ischial tuberosity. J Neurosurg 1998;89:819-21. [Crossref] [PubMed]
- Levy GM, Phil L, Nigel H. Efficacy of a platelet-rich plasma injection for the treatment of proximal hamstring tendinopathy: A pilot study. J Sci Med Sport 2019;22:247-52. [Crossref] [PubMed]
- Schoensee SK, Nilsson KJ. A novel approach to treatment for chronic avulsion fracture of the ischial tuberosity in three adolescent athletes: a case series. Int J Sports Phys Ther 2014;9:974-90. [PubMed]
- Perets I, Rybalko D, Mu BH, et al. Hip Arthroscopy: extra-articular Procedures. Hip Int 2019;29:346-54. [Crossref] [PubMed]
- Saikku K, Vasenius J, Saar P. Entrapment of the proximal sciatic nerve by the hamstring tendons. Acta Orthopaedica Belgica 2010;76:321-4. [PubMed]
- Arévalo Galeano N, Santamaría Guinea N, Gredilla Molinero J, et al. Extra-articular hip impingement: A review of the literature. Radiología 2018;60:105-18. [PubMed]
- Tosun O, Algin O, Yalcin N, et al. Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skeletal Radiol 2012;41:575-87. [Crossref] [PubMed]
- Singer AD, Subhawong TK, Jose J, et al. Ischiofemoral impingement syndrome: a meta-analysis. Skeletal Radiol 2015;44:831-7. [Crossref] [PubMed]
- Hernando MF, Cerezal L, Perez-Carro L, et al. Evaluation and management of ischiofemoral impingement: a pathophysiologic, radiologic, and therapeutic approach to a complex diagnosis. Skeletal Radiol 2016;45:771-87. [Crossref] [PubMed]
- Domb BG, Linder D, Sharp KG, et al. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech 2013;2:e35-9. [Crossref] [PubMed]
- Dierckman BD, Guanche CA. Endoscopic Proximal Hamstring Repair and Ischial Bursectomy. Arthrosc Tech 2012;1:e201-7. [Crossref] [PubMed]
- van der Made AD, Reurink G, Gouttebarge V, et al. Outcome After Surgical Repair of Proximal Hamstring Avulsions: A Systematic Review. Am J Sports Med 2015;43:2841-51. [Crossref] [PubMed]
- Biedert RM. Surgical Management of Traumatic Avulsion of the Ischial Tuberosity in Young Athletes. Clin J Sport Med 2015;25:67-72. [Crossref] [PubMed]
Cite this article as: Huang H, Yang F, Zheng X, Zhang X, Wang J, Xu Y. Arthroscopic management of the nonunion avulsion fracture of ischial tuberosity for a teenager dancer: a case report. Ann Joint 2021;6:35.