
Biomechanics of the lateral meniscus: evidences from narrative review
Introduction
Menisci are crucial structures of the knee joint and effectively contribute to maintaining a normal articular function. Their peculiar anatomy and mechanical properties provide joint congruity, minimize the shocks on the articular cartilage by distributing the loads, and grant joint stability in a synergic role with the surrounding knee structures (1,2).
The biomechanical role of the menisci has been extensively investigated over time (3-6). The differences between medial and lateral meniscus, their role at different degrees of knee flexion, and the effect of different surgical treatments have been the most debated issues. The research on the latter issues contributed to extending the knowledge on the function of the menisci, leading to influence the choices of daily clinical practice and to develop new solutions, such as biological/artificial transplantation.
In this scenario, greater attention has been given to the biomechanics of the medial meniscus, while less on the lateral one. This was probably due to the primary effect of the medial meniscus in articular cartilage preservation and anterior-posterior (AP) knee stability and a more difficult assessment of lateral meniscus function (4,7,8). Indeed, the lateral meniscus was proved to have a key role in rotatory instability (8-11), which requires a more complex evaluation setting, either in vitro or in vivo.
The aim of the present study was to provide an overview of literature knowledge regarding the biomechanics of lateral meniscus and give further insights about its role through novel experimental analyses from our study group.
We present the following article in accordance with the Narrative Review checking checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-123/rc).
Literature overview and authors’ experience
For the sake of clarity, the literature overview on the biomechanics of lateral meniscus was divided into three sections, namely “Mobility”, “Laxity” and “Contact mechanics”. In each section, different clinical procedures such as meniscal repair, meniscectomy, and meniscus allograft transplantation (MAT) were considered. The authors’ experience was also reported in terms of experimental analyses.
Mobility
Meniscus mobility is aimed to ensure the largest contact surface between femur and tibial during the entire knee range of motion. This allows to avoiding cartilage overloading and to increasing overall knee stability. The lateral meniscus mobility has been widely investigated. As compared to the medial one, the lateral meniscus shows higher mobility during knee motion (Figure 1). In particular, there is a more pronounced posterior translation of the lateral meniscus compared to the medial one as knee flexion increases. With a fully flexed knee, the lateral meniscus drops off from the posterior rim of the tibia (12). This happens because of its structural characteristics: lateral meniscus has a more circular shape, is thicker at the periphery and is less firmly attached to the lateral collateral ligament and to the popliteal hiatus (13). Moreover, the convex posterior aspect of the lateral tibial plateau allows a higher posterior displacement of the lateral meniscus in deep flexion (14). During the knee range of motion from 0° to 90°, the maximum posterior displacement of the lateral meniscus has been identified for the anterior horn, average respectively in 9.5 mm in weightbearing conditions and 6.3 mm in non-weightbearing conditions (14).
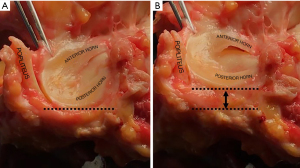
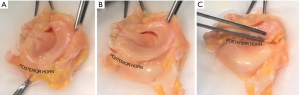
Simonian et al. (15) investigated the contribution of the anteroinferior and posterosuperior popliteomeniscal fasciculi to the mobility of lateral meniscus. The authors performed a subsequent resection of the two fasciculi and applied a 10-N load to 7 fresh-frozen cadavers. They highlighted that the popliteal hiatus both provides higher mobility to the lateral meniscus and is crucial to preserve the stability of the posterior horn (Figure 2A,2B). However, the section of both anteroinferior and posterosuperior popliteomeniscal fasciculi was never able to allow anterior meniscal displacement and to cause meniscal locking. Therefore, other structures such as menisco-tibial ligament play a role in meniscal stability under extreme antero-posterior excursion (Figure 2C). Thus, the lesion or absence of these structure could be responsible of different clinical symptoms, from catching and popping to real knee unreducible locking.
These peculiar characteristics makes the lateral meniscus a key structure in dynamic movements since it supports the activity of anterolateral complex in stabilizing the knee during high demanding daily life activities and sport.
Laxity
Due to its larger mobility to the medial one, lateral meniscus plays a greater role in restraining rotatory laxity. Either in vitro, in silico, or in vivo studies were conducted to assess the role of the lateral meniscus on knee laxity. Cadaveric studies were conducted with heterogeneous settings: either surgical navigation systems or robotic and servo-hydraulic testing systems were used. The pivot-shift maneuver, either mechanized or manually performed by surgeons, was the most investigated test. Limited literature can be found regarding computational knee models including menisci. Musculoskeletal and finite element (FE) analyses often adopt simplification of knee anatomy to reduce model complexity and computational cost (16,17), e.g., menisci or ligaments are not present or are simulated with spring bundles, neglecting the real anatomy (18). The effect of lateral meniscus laxity has been poorly investigated in vivo. A difficult clinical setting, the need for highly experienced surgeons with robust reliability in pivot-shift movements, and a limited number of eligible cases are the most likely reasons. Indeed, the effect of lateral meniscus removal or repair was mainly evaluated in association with ACL-deficient or ACL-reconstructed knees.
On the one hand, when assessing anterior tibial translation (ATT) during static tests, e.g., Lachman test, several authors confirmed a limited or null effect of lateral meniscus both in ACL-deficient and ACL-reconstructed knees (19,20). On the other hand, Musahl et al. reported an increase of anterior translation of knee lateral compartment after total lateral meniscectomy and ACL reconstruction during manual pivot-shift maneuver evaluated through surgical navigation system (21). Similar findings were also reported in the presence of bilateral meniscectomy after ACL reconstruction (22).
Using a combined musculoskeletal and FE in silico model, Hu et al. (23) simulated normal gait with intact menisci and with bilateral meniscectomy. The authors found a more posterior tibial translation and internal tibial rotation in the model without menisci. Liu et al. (24) simulated a level walking from gait analysis of ACL-deficient patients with different meniscal lesions (either medial, lateral, and bilateral). Altered kinematics and kinetics were found in the presence of bilateral meniscectomy, with lower abduction-adduction and internal-external moment peaks compared to the control group. Such differences were not found in the presence of isolated lateral meniscectomy.
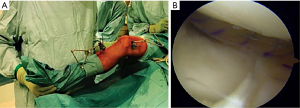
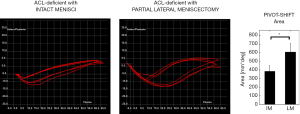
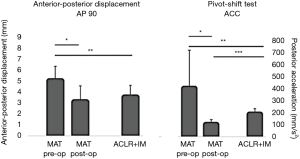
A recent in vivo study (9) provided an extensive intraoperative evaluation (164 patients) of ACL-deficient knee combined with either medial, lateral, and bilateral meniscectomy (Figure 3). In the present study, the quantitative kinematical assessment was performed after meniscus treatment and before ACL reconstruction during surgery. The present study confirmed the distinct effect of medial and lateral meniscectomy on knee laxity and particularly highlighted an increased rotatory instability during the pivot-shift maneuver for patients with combined lateral meniscectomy (Figure 4).
Navigation systems in cadaver settings were also used to investigate the effect of lateral posterior root lesions in ACL-deficient conditions (25,26). An overall stability reduction during rotational loadings was noted. Particularly, an increase of internal tibial rotation at high degrees of knee flexion was found compared to the isolated ACL-deficiency (25,27).
Other than navigation systems and robots, triaxial accelerometers were used to investigate combined ACL and meniscal lesions in non-invasive clinical ambulatory settings Figure 5. Musahl et al. (28) quantitatively investigated the knee laxity through iPad image analysis technique in 41 ACL-deficient knees under-anesthesia. Combined lesions to surrounding structures were assessed through MRI. The authors concluded that the presence of lateral meniscus lesion in ACL-deficient knees was associated with an increase of rotatory laxity during the pivot-shift maneuver. A further study with a similar setting performed by the same group (29) on 77 patients concluded that the combination of ACL and lateral meniscus injury generates an increase in tibial lateral compartment acceleration and translation and could therefore be a reason for qualitatively-evaluated high rotatory instability. Hoshino et al. (30) reached similar conclusions assessing that high rotatory instability during pivot-shift could be symptomatic of combined ACL and lateral meniscal lesion.

Meniscus repair was claimed as the most valuable solution to restore intact knee stability (8,31). Forkel et al. found that lateral posterior meniscus root repair can reduce internal rotation in ACL-deficient knee conditions (27). Also, a significant improvement in rotatory knee stability was found by Tang et al. (32). The latter studies were both performed in cadaveric conditions. Katakura et al. (33) found similar results in 41 patients undergoing ACL-reconstruction and meniscal repair through a triaxial accelerometer.
Residual laxity in animal in vitro models was also assessed after arthroscopic centralization techniques for irreparable lateral meniscus defects (34). Significant rotational laxity reduction was found in ACL-reconstructed porcine knees in the presence of arthroscopic centralization.
Few in vitro studies investigated the biomechanical effect of lateral MAT. Through a surgical navigation system, Spang et al. (35) demonstrated an effective reduction of ATT when MAT was performed. In a similar setting, Novaretti et al. (36) demonstrated a partial reduction of AP laxity compared to a meniscectomized knee. In both studies, however, criticisms emerged regarding the restoration of intact knee stability after MAT.
In vivo, a preliminary kinematic analysis of knee laxity was conducted in the presence of lateral MAT and ACL reconstruction (37). Using a surgical navigation system, the authors suggested a synergic role of MAT and ACL in restraining knee laxity, especially AP translation. No other evidence in literature is present regarding the in vivo kinematical evaluation of MAT. An unpublished study from the same group was aimed to describe the kinematical effect of lateral MAT by comparing three different conditions: intact ACL with lateral meniscectomy, intact ACL with MAT, and ACL-reconstructed with intact menisci. The analysis was again performed through a surgical navigation system. Both static and dynamic laxity parameters, in particular, AP30, AP90, VV0, and pivot-shift parameters, improved at time zero after MAT surgery. Moreover, patients undergoing MAT showed similar or even lower laxity than patients in ACL-reconstructed with intact menisci conditions (Figure 6). These results demonstrated a significant positive effect of MAT on knee laxity, both in ACL-deficient and ACL-injured conditions.
Contact mechanics
The shock absorber role for axial and circumferential loads is carried out in synergy by medial and lateral meniscus. They have peculiar viscoelastic material properties that allow substantial shape-changing under weight-bearing conditions. For example, compression stresses (e.g., during standing) are first resisted (“creep” behavior) and then distributed and reduced over time (“stress relaxation” behavior) (3). The lateral meniscus mainly carries circumferential loads and to undergoes shear stresses (38), unloading the tibial cartilage more than how it happens on the medial side (39).
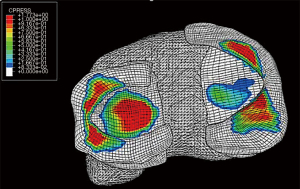
The setup required to investigate menisci contact mechanics is hugely complex and invasive. For this reason, the lateral meniscus has been investigated only in cadaveric and in computer model studies. Several cadaver studies were conducted to analyze knee contact mechanics with lateral meniscus either in intact condition, in the presence of tears, or after transplantation. Setups and loading conditions were highly heterogeneous. In silico studies were used to extend the findings of cadaver studies or to reproduce from scratch either meniscus tears or allograft transplantation contact mechanics (Figure 7). Different levels of complexity were adopted, especially in terms of loads applied. Furthermore, meniscectomies, meniscal lesions, and repairs were often evaluated in the same cadaveric or computational study.
Koh et al. (40) investigated tibiofemoral contact mechanics in intact lateral meniscus conditions and in the presence of partial lateral meniscectomy. The study was conducted on fresh-frozen cadavers under axial load in full knee extension and at 60°. The author found significantly reduced contact areas and increased peak contact pressure after resection of either only inferior leaf or both leaves. A similar loading condition was simulated in the cadaveric study by LaPrade et al. (10), even though the evaluation was performed at more flexion angles, and meniscus repair was investigated as well.
A significant decrease in the contact area and an increase in peak contact pressure were found in the presence of meniscal tears at all the flexion angles. Interestingly, the authors demonstrated that pull-out suture repair restored both contact area and pressure to the ones of the intact lateral meniscus only at high degrees of knee flexion (from 45° to 90°), while no differences were found between repair and meniscectomized knees at 0° and 30°. The authors concluded that repair techniques are less effective at lower flexion angles at increasing distances between radial tear and the posterior horn root attachment. A more complex setup was used to simulate human gait in lateral meniscus intact, with radial tears, repaired, and meniscectomized conditions (41). The authors found increased knee contact pressure in all the non-intact conditions. In particular, contact pressures after large radial tears and meniscectomies were statistically equivalent, while significant pressure reduction was found after meniscus repair.
A simple compressive axial load of 1,000 N was applied in the FE study by Bao et al. (42). The authors compared contact pressure in three lateral meniscus conditions of ascending complexity: complete radial posterior lateral meniscus root tear, a complete radial posterior lateral meniscus root tear with posterior meniscofemoral ligament deficiency, and total meniscectomy of the lateral meniscus. They concluded that increasing contact pressure and decreased contact area followed the complexity of lateral meniscus condition. Radial tears and partial meniscectomy were evaluated by Mononen et al. (43) with a complex MRI-based knee model and simulated gait cycle. The authors suggested anterior radial tears as the main cause for the progression of meniscal rupture and partial meniscectomy as the main risk factor for the progression of lateral tibial cartilage osteoarthritis. The highest contact pressures were found during the mid-stance and loading response of the stance phase. Similarly, Zhang et al. (44) simulated longitudinal lesions on the posterior horn during static stance and mid-flexion. The authors concluded that an increased contact pressure was present on the posterior lateral tibial cartilage in the mid-flexion condition.
In vitro models were also adopted to investigate centralization procedures’ biomechanical role in the presence of extruded lateral meniscus (45,46) and of meniscal scaffolds (47,48). Significant reduction in contact area and increased contact pressure were found in lateral meniscus extrusion (created by resecting the posterior root) in porcine knee joints (45,46). Centralization procedures showed a restored loading-distribution as well as reduction of lateral meniscus extrusion. Positive biomechanical evidences emerged also from the use of lateral meniscus scaffolds. Although all the studies concluded that in vivo evidence is still lacking, promising results emerged from pre-clinical analyses in animal models in terms of load distribution recover (47,48).
The role of MAT on knee contact pressure and area was also evaluated in cadaveric setting. Different techniques were investigated: both bony and keyhole fixation of the native meniscus (49) and bone-block and suture-only fixation of allograft (36) meniscus. Brial et al. used a multidirectional dynamic simulator to reproduce two specific instants of the gait cycle (14% and 45% of the stance phase). Compared to the meniscectomized knees, MAT contributes to reducing peak contact pressure and to restoring both contact area and cartilage-to-cartilage contact as in the intact conditions. They concluded that keyhole fixation reproduced the closest intact knee mechanics. Novaretti et al. applied multiple combined loading conditions (anteroposterior + axial, internal rotation + valgus torque, external rotation + valgus torque) at different degrees of knee flexion through a robotic system. The authors found that resultant forces on MAT were 50% to 60% of the ones on the intact lateral meniscus, thus strongly contributing to load-bearing function even without restoring the native meniscus conditions. Moreover, they found no differences between bone-block and suture-only MAT fixation techniques.
A computational simulation was also conducted to evaluate the influence of lateral MAT on knee mechanics (50). An MRI-based knee model was used to simulate the stance phase of the gait cycle either in lateral intact meniscus conditions or after lateral MAT. The authors found that the presence of lateral MAT increases the contact stress on the lateral side up to 20% while reducing on it the medial one. This last aspect was considered predictive for reduced risk of medial osteoarthritis onset.
Conclusions
Different aspects emerged from the present literature overview regarding the biomechanics of lateral meniscus. First, great effort has been put into exploring this topic from multiple perspectives, such as laxity and contact mechanics, type of lesion, and repair technique. All the studies agreed on the crucial role of the lateral meniscus in knee biomechanics, both in terms of pivoting movements and daily life activities such as gait. Second, strong evidence emerged from both in vivo, cadaveric, and computer model studies regarding the importance of lateral meniscus repair. Increased knee stability at high degrees of knee flexion and reduction of peak contact pressures on tibial cartilage were the most reported benefits from repair. The MAT is also emerging as a concrete alternative in the presence of irreparable tears. Recent studies confirmed its role in restoring intact-like biomechanics and balancing the loads onto the tibial cartilage. Further studies are needed to investigate the influence of MAT on knee biomechanics at long term follow-ups.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Joint for the series “The Lateral Meniscus”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Revie reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-123/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-123/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. SZ served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Joint from March 2021 to February 2023. AG served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 1998;193:161-78. [Crossref] [PubMed]
- Hulet C, Pereira H, Peretti G, et al. Surgery of the Meniscus. Berlin, Heidelberg: Springer Berlin Heidelberg, 2016.
- Ellman MB, Chahla J. Meniscus: Biomechanics and Biology. In: Yanke AB, Cole BJ, editors. Joint Preservation of the Knee, Cham: Springer International Publishing, 2019:25-39.
- Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am 1986;68:71-9. [Crossref] [PubMed]
- Masouros SD, McDermott ID, Amis AA, et al. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc 2008;16:1121-32. [Crossref] [PubMed]
- Smoak JB, Matthews JR, Vinod AV, et al. An Up-to-Date Review of the Meniscus Literature: A Systematic Summary of Systematic Reviews and Meta-analyses. Orthop J Sports Med 2020;8:2325967120950306. [Crossref] [PubMed]
- Allen CR, Wong EK, Livesay GA, et al. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res 2000;18:109-15. [Crossref] [PubMed]
- Grassi A, Dal Fabbro G, Di Paolo S, et al. Medial and lateral meniscus have a different role in kinematics of the ACL-deficient knee: a systematic review. J ISAKOS 2019;4:233. [Crossref]
- Grassi A, Di Paolo S, Lucidi GA, et al. The Contribution of Partial Meniscectomy to Preoperative Laxity and Laxity After Anatomic Single-Bundle Anterior Cruciate Ligament Reconstruction: In vivo Kinematics With Navigation. Am J Sports Med 2019;47:3203-11. [Crossref] [PubMed]
- LaPrade CM, Jansson KS, Dornan G, et al. Altered Tibiofemoral Contact Mechanics Due to Lateral Meniscus Posterior Horn Root Avulsions and Radial Tears Can Be Restored with in Situ Pull-Out Suture Repairs. J Bone Joint Surg Am 2014;96:471-9. [Crossref] [PubMed]
- Hoshino Y, Hiroshima Y, Miyaji N, et al. Unrepaired lateral meniscus tears lead to remaining pivot-shift in ACL-reconstructed knees. Knee Surg Sports Traumatol Arthrosc 2020;28:3504-10. [Crossref] [PubMed]
- Nakagawa S, Kadoya Y, Todo S, et al. Tibiofemoral movement 3: full flexion in the living knee studied by MRI. J Bone Joint Surg Br 2000;82:1199-200. [Crossref] [PubMed]
- Benazzo F, Zanon G. Meniscal Sutures. Tech Knee Surg 2010;9:159-64. [Crossref]
- Vedi V, Williams A, Tennant SJ, et al. Meniscal movement. An in vivo study using dynamic MRI. J Bone Joint Surg Br 1999;81:37-41. [Crossref] [PubMed]
- Simonian PT, Sussmann PS, van Trommel M, et al. Popliteomeniscal Fasciculi and Lateral Meniscal Stability. Am J Sports Med 1997;25:849-53. [Crossref] [PubMed]
- Pfeiffer FM. The Use of Finite Element Analysis to Enhance Research and Clinical Practice in Orthopedics. J Knee Surg 2016;29:149-58. [Crossref] [PubMed]
- Benos L, Stanev D, Spyrou L, et al. A Review on Finite Element Modeling and Simulation of the Anterior Cruciate Ligament Reconstruction. Front Bioeng Biotechnol 2020;8:967. [Crossref] [PubMed]
- Bolcos PO, Mononen ME, Mohammadi A, et al. Comparison between kinetic and kinetic-kinematic driven knee joint finite element models. Sci Rep 2018;8:17351. [Crossref] [PubMed]
- Wieser K, Betz M, Farshad M, et al. Experimental loss of menisci, cartilage and subchondral bone gradually increases anteroposterior knee laxity. Knee Surg Sports Traumatol Arthrosc 2012;20:2104-8. [Crossref] [PubMed]
- Musahl V, Bedi A, Citak M, et al. Effect of single-bundle and double-bundle anterior cruciate ligament reconstructions on pivot-shift kinematics in anterior cruciate ligament- and meniscus-deficient knees. Am J Sports Med 2011;39:289-95. [Crossref] [PubMed]
- Musahl V, Citak M, O’Loughlin PF, et al. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2010;38:1591-7. [Crossref] [PubMed]
- Petrigliano FA, Musahl V, Suero EM, et al. Effect of meniscal loss on knee stability after single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:S86-93. [Crossref] [PubMed]
- Hu J, Xin H, Chen Z, et al. The role of menisci in knee contact mechanics and secondary kinematics during human walking. Clin Biomech (Bristol, Avon) 2019;61:58-63. [Crossref] [PubMed]
- Liu X, Huang H, Yin W, et al. Anterior cruciate ligament deficiency combined with lateral and/or medial meniscal injury results in abnormal kinematics and kinetics during level walking. Proc Inst Mech Eng H 2020;234:91-9. [Crossref] [PubMed]
- Frank JM, Moatshe G, Brady AW, et al. Lateral Meniscus Posterior Root and Meniscofemoral Ligaments as Stabilizing Structures in the ACL-Deficient Knee: A Biomechanical Study. Orthop J Sports Med 2017;5:2325967117695756. [Crossref] [PubMed]
- Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2015;43:905-11. [Crossref] [PubMed]
- Forkel P, von Deimling C, Lacheta L, et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 2018;26:2302-9. [Crossref] [PubMed]
- Musahl V, Rahnemai-Azar AA, Costello J, et al. The Influence of Meniscal and Anterolateral Capsular Injury on Knee Laxity in Patients With Anterior Cruciate Ligament Injuries. Am J Sports Med 2016;44:3126-31. [Crossref] [PubMed]
- Musahl V, Burnham J, Lian J, et al. High-grade rotatory knee laxity may be predictable in ACL injuries. Knee Surg Sports Traumatol Arthrosc 2018;26:3762-9. [Crossref] [PubMed]
- Hoshino Y, Miyaji N, Nishida K, et al. The concomitant lateral meniscus injury increased the pivot shift in the anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc 2019;27:646-51. [Crossref] [PubMed]
- Tang X, Marshall B, Wang JH, et al. Partial meniscectomy does not affect the biomechanics of anterior cruciate ligament reconstructed knee with a lateral posterior meniscal root tear. Knee Surg Sports Traumatol Arthrosc 2020;28:3481-7. [Crossref] [PubMed]
- Tang X, Marshall B, Wang JH, et al. Lateral Meniscal Posterior Root Repair With Anterior Cruciate Ligament Reconstruction Better Restores Knee Stability. Am J Sports Med 2019;47:59-65. [Crossref] [PubMed]
- Katakura M, Horie M, Watanabe T, et al. Effect of meniscus repair on pivot-shift during anterior cruciate ligament reconstruction: Objective evaluation using triaxial accelerometer. Knee 2019;26:124-31. [Crossref] [PubMed]
- Nakamura T, Linde MA, Marshall BD, et al. Arthroscopic centralization restores residual knee laxity in ACL-reconstructed knee with a lateral meniscus defect. Knee Surg Sports Traumatol Arthrosc 2019;27:3699-704. [Crossref] [PubMed]
- Spang JT, Dang ABC, Mazzocca A, et al. The effect of medial meniscectomy and meniscal allograft transplantation on knee and anterior cruciate ligament biomechanics. Arthroscopy 2010;26:192-201. [Crossref] [PubMed]
- Novaretti JV, Lian J, Sheean AJ, et al. Lateral Meniscal Allograft Transplantation With Bone Block and Suture-Only Techniques Partially Restores Knee Kinematics and Forces. Am J Sports Med 2019;47:2427-36. [Crossref] [PubMed]
- Zaffagnini S, Di Paolo S, Stefanelli F, et al. The biomechanical role of meniscal allograft transplantation and preliminary in vivo kinematic evaluation. J Exp Orthop 2019;6:27. [Crossref] [PubMed]
- Andrews SHJ, Adesida AB, Abusara Z, et al. Current concepts on structure-function relationships in the menisci. Connect Tissue Res 2017;58:271-81. [Crossref] [PubMed]
- Walker PS, Hajek JV. The load-bearing area in the knee joint. J Biomech 1972;5:581-9. [Crossref] [PubMed]
- Koh JL, Zimmerman TA, Patel S, et al. Tibiofemoral Contact Mechanics With Horizontal Cleavage Tears and Treatment of the Lateral Meniscus in the Human Knee: An In vitro Cadaver Study. Clin Orthop Relat Res 2018;476:2262-70. [Crossref] [PubMed]
- Bedi A, Kelly N, Baad M, et al. Dynamic contact mechanics of radial tears of the lateral meniscus: implications for treatment. Arthroscopy 2012;28:372-81. [Crossref] [PubMed]
- Bao HRC, Zhu D, Gong H, et al. The effect of complete radial lateral meniscus posterior root tear on the knee contact mechanics: a finite element analysis. J Orthop Sci 2013;18:256-63. [Crossref] [PubMed]
- Mononen ME, Jurvelin JS, Korhonen RK. Effects of radial tears and partial meniscectomy of lateral meniscus on the knee joint mechanics during the stance phase of the gait cycle--A 3D finite element study. J Orthop Res 2013;31:1208-17. [Crossref] [PubMed]
- Zhang K, Li L, Yang L, et al. The biomechanical changes of load distribution with longitudinal tears of meniscal horns on knee joint: a finite element analysis. J Orthop Surg Res 2019;14:237. [Crossref] [PubMed]
- Kubota R, Koga H, Ozeki N, et al. The effect of a centralization procedure for extruded lateral meniscus on load distribution in porcine knee joints at different flexion angles. BMC Musculoskelet Disord 2020;21:205. [Crossref] [PubMed]
- Ozeki N, Koga H, Matsuda J, et al. Biomechanical analysis of the centralization procedure for extruded lateral menisci with posterior root deficiency in a porcine model. J Orthop Sci 2020;25:161-6. [Crossref] [PubMed]
- Di Matteo B, Perdisa F, Gostynska N, et al. Meniscal Scaffolds - Preclinical Evidence to Support their Use: A Systematic Review. Open Orthop J 2015;9:143-56. [Crossref] [PubMed]
- Moran CJ, Busilacchi A, Lee CA, et al. Biological Augmentation and Tissue Engineering Approaches in Meniscus Surgery. Arthroscopy 2015;31:944-55. [Crossref] [PubMed]
- Brial C, McCarthy M, Adebayo O, et al. Lateral Meniscal Graft Transplantation: Effect of Fixation Method on Joint Contact Mechanics During Simulated Gait. Am J Sports Med 2019;47:2437-43. [Crossref] [PubMed]
- Koh YG, Lee JA, Kim YS, et al. Biomechanical influence of lateral meniscal allograft transplantation on knee joint mechanics during the gait cycle. J Orthop Surg Res 2019;14:300. [Crossref] [PubMed]
Cite this article as: Di Paolo S, Grassi A, Lucidi GA, Macchiarola L, Dal Fabbro G, Zaffagnini S. Biomechanics of the lateral meniscus: evidences from narrative review. Ann Joint 2022;7:19.


