
A narrative review of lateral meniscus root tears and extrusion: techniques and outcomes
Introduction
Menisci play a pivotal role in the shock-absorbing and load-dispersing functions of the knee joint. They also contribute to its stability (1,2). The medial meniscus (MM) can act as a secondary stabilizer of anterior tibial translation. The lateral meniscus (LM) provides anterolateral laxity in anterior cruciate ligament (ACL)-deficient knees (3,4). Meniscal extrusion induces dysfunction of load distribution (1,2,5) and is caused by the disruption of the meniscus hoop function. It is often observed after meniscectomy (1,6,7), meniscus root tears (8), discoid LM (6,9) and in aging (10-12). Consequently, meniscal extrusion initiates osteoarthritis (OA) and is accompanied by its progression (13-16).
Posterior root tear (PRT) is an avulsion injury or radial tear within 1 cm of the meniscal attachment site. LM posterior root tears (LMPRT) occur in 10–15% of all ACL injury cases (17,18). However, PRTs on the MM are rare in ACL-injured knees (18). LMPRT should be repaired if at all possible. LMPRT has been shown to affect anterolateral knee laxity and tibiofemoral contact pressure in ACL-injured knees in both clinical (18) and biomechanical studies (19,20). In terms of the effects of LMPRT repair, some biomechanical studies have revealed that LMPRT repair improves knee stability, reduces ACL graft force, and restores load-distribution function (21-23). In this review, we described our surgical technique for LMPRT repair. We also performed a narrative search of the literature.
Previously, there was no surgical solution for a meniscal extrusion for causes seen after meniscectomy and discoid LM. We developed an arthroscopic centralization technique to reduce meniscal extrusion. The capsule attached to the meniscus was sutured to the edge of the tibial plateau using suture anchors (24). The centralization technique could restore the lost function caused by meniscal extrusion (25-27). It could also delay OA progression (28). In addition, arthroscopic centralization of the extruded LM improved clinical outcomes at the 2-year follow-up (29). In this article, a narrative review of the literature for the arthroscopic centralization technique for lateral extruded meniscus was performed. It describes the indications, surgical techniques, clinical outcomes, and biomechanics of this procedure.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-112/rc).
LMPRT repair
A literature review of LMPRT repair
A narrative review of the literature for LMPRT repair was performed using PubMed. The main criteria for selection were articles focused on the biomechanical role of LMPRT, magnetic resonance imaging (MRI) examination of LMPRT, and the clinical outcomes of LMPRT repair.
Biomechanical role of LMPRT and repair
Meniscal root tears substantially affect meniscal hoop function and accelerate cartilage degeneration. The LM posterior root also plays an important role as a secondary restraint against pivotal shift in ACL-deficient knees. A cadaveric study showed that LMPRT significantly increased the pivotal shift in ACL-deficient knees (19). Clinically, it has also been shown that LMPRT is associated with a larger pivot shift grade in ACL-injured knees (30). Its repair decreases tibial acceleration during the pivot shift test (4). Tang et al. (23) reported that LMPRT repair improves anterolateral laxity and reduces ACL graft force in ACL-reconstructed knees in a cadaveric study. Therefore, the importance of LMPRT repair at the time of ACL surgery has been widely recognized. In recent years efforts have been made to develop successful repair techniques (31).
MRI diagnosis of LMPRT
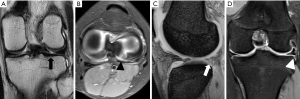
A high percentage of LMPRTs are often missed. It is nearly impossible to diagnose them preoperatively with imaging techniques (32). Consequently, surgeons should prepare the necessary instruments for LMPRT repair in all ACL reconstruction surgeries. Nevertheless, several studies have demonstrated the usefulness of MRI findings. Minami et al. (18) calculated the sensitivities and specificities of vertical linear defects in the coronal plane (Figure 1A), radial linear defects in the axial plane (Figure 1B), ghost sign in the sagittal plane (Figure 1C), and meniscus extrusion in the coronal plane (Figure 1D). The authors demonstrated that 71.8% of patients showed at least one positive sign. The highest sensitivity was 69.2% for vertical linear defects. Asai et al. (33) examined three specific signs: vertical linear defects (cleft sign), ghost signs, and the truncated triangle sign in the sagittal plane. They further demonstrated that vertical linear defects (cleft sign) showed the highest sensitivity of 65.6%. They also demonstrated that the combination of these signs improved the approximate sensitivity by up to 80%. With regard to meniscal extrusion, there was a relationship between the meniscal extrusion and the status of LMPRT in ACL injury patients (34). The average meniscus extrusion width was 0.2±0.5 mm in patients with intact LM, 0.4±0.8 mm in patients with partial LMPRT, and 2.0±0.6 mm in patients with complete LMPRT. This suggests that meniscal extrusion is a useful indicator for estimating the status of LMPRT. Therefore, careful preoperative evaluation with MRI would assist in the diagnosis of LMPRT.
Clinical outcomes of LMPRT repair
There were primarily two surgical techniques utilized in LMPR repairs. Side-to-side suture repair was performed in radial tears if there was a root remnant with adequate tissue quality. A pull-out repair was conducted in root avulsions and radial tears with an inadequate meniscal remnant. Ahn et al. (35) demonstrated favorable short-term results of an all-inside side-to-side LMPRT repair in ACLR patients. They reported that over a mean follow-up period of 18 months the mean subjective International Knee Documentation Committee Subjective Knee Form (IKDC) scores and Lysholm scores significantly improved from 67 to 90 and from 62 to 93, respectively. Anderson et al. (36) also reported the clinical outcomes of both an all-inside side-to-side repair and a transtibial pull-out repair over a mean follow-up of 58 months in ACLR patients. In patients who underwent a side-to-side repair, the mean subjective IKDC and Lysholm scores were 82 and 87, respectively; patients who underwent a transtibial pull-out repair had scores of 84 and 86, respectively. However, these studies were case series. They did not show the effects of the LMPRT repair itself. In contrast, Pan et al. (37) compared ACLR patients who underwent an LMPRT repair with those who did not. They reported higher functional scores (although not significant) and statistically lower rates of radiological osteoarthritic changes in patients who underwent an LMPRT repair. In terms of meniscal extrusion, a transtibial pull-out repair of LMPRT achieved reduction of meniscal extrusion (38,39). These results indicate that an LMPRT repair successfully recovered the hoop function of the LM. Several studies have reported the healing rates of LMPRT after a repair with second-look arthroscopy. The complete/partial healing rate ranged from 86.7% to 100% (35,36,40,41). This seemed to be better than the 61% healing rate of radial tears in the midbody of LM (42). Overall, LMPRT repair concomitant with an ACLR resulted in favorable outcomes.
Our surgical technique of LMPRT repair and its clinical outcomes
Our indications for LMPRT repair include all types of LMPRT to prevent acceleration of articular cartilage degeneration as well as to control anterolateral instability. First, a standard arthroscopy is performed through anterolateral and anteromedial portals to evaluate the status of the menisci and ACL. If LMPRT is identified (Figure 2A-2C), it is repaired appropriately. Most type 2a and 2b tears under the LaPrade classification (43) are repaired using a pull-out technique. Fibrous tissues around the torn meniscus edge are removed and adhesions around the torn meniscus edge are released using a motorized shaver. An ACUFEX™ Director ACL Tip Aimer (Smith and Nephew Endoscopy, Andover, MA, USA) is inserted from the anteromedial portal with the tip of the aimer placed over the attachment site of the LM posterior root (Figure 2D). A 2.4 mm guidewire is inserted from the anteromedial aspect of the proximal tibia. A 6-mm-diameter tunnel is then created with a cannulated drill (Figure 2E). The 6-mm-diameter tunnel allows the meniscus and bone to heal by pulling the torn edge of the LM posterior root into the tunnel. Articular cartilage around the bone tunnel is removed with a curette until the subchondral bone is exposed to promote adhesion of the meniscus to the bone (Figure 2F). A vertical mattress suture with a 2-0 FiberWire (Arthrex, Naples, FL, USA) is applied approximately 3 mm away from the torn edge of the meniscus using a Knee Scorpion Suture Passer (Arthrex) (Figure 2G). The tied suture is left uncut so that it can be pulled into the tunnel. Two racking hitch knot sutures with SutureTapes (Arthrex) are placed over the vertical mattress suture as a locking suture to securely hold the torn edge of the meniscus (Figure 2H,I). The sutures are then shuttled through the tunnel to the anteromedial aspect of the proximal tibia (Figure 2J). Using the arthroscopic view from the anterolateral port, the suture ends for the LMPRT are finally tied over a TightRope ABS Button (Arthrex) under adequate tension (Figure 2K). A final arthroscopic evaluation is performed to confirm reattachment of the LM posterior root to the insertion site, adequate tension within the entire meniscus, and reduction of the extruded meniscus (Figure 2L). The tips and pitfalls of this technique are presented in Table 1. Type 2c and type 4 tears are repaired using the all-inside suture technique. ACL reconstruction is performed following LMPRT repair.
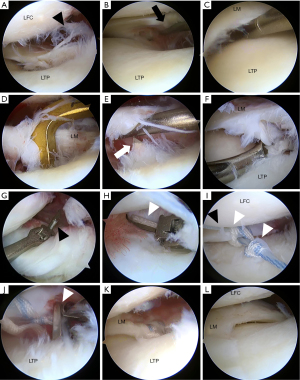
Table 1
| Tips | Pitfalls |
|---|---|
| Use a curette to remove articular cartilage around the tunnel to enhance adhesion of the meniscus to bone | LMPRT (especially in chronic phase) is often missed even under arthroscopic observation. Careful probing to check lift-off sign is useful for diagnosis of LMPRT |
| Position the transtibial tunnel for the pull-out repair at the anatomic footprint of the LM posterior root insertion site | When resecting fibrous tissues around torn site, surgeons should be careful not to resect the meniscofemoral ligament |
| As secure a fixation as possible should be performed for the LMPRT repair, and if the fixation is not secure enough or reduction of the meniscus extrusion is not achieved, additional centralization for augmentation should be considered | Avoid overlap of bone tunnels for LMPRT repair and ACL reconstruction |
LM, lateral meniscus; LMPRT, lateral meniscus posterior root tear; ACL, anterior cruciate ligament.
The postoperative rehabilitation protocol is the same regardless of the presence of LMPRT repair. Patients can begin to practice range of motion and quadriceps-setting exercises one day after surgery. Weightbearing and walking exercises with crutches and a knee brace are ordered on the third postoperative day. Crutches are removed after four-weeks. Running exercises are initiated at three months. Patients progress to full activity after 6 months.
We compared 22 ACLR patients with simultaneous LMPRT repair with 75 ACLR patients without meniscus injury. The Knee Injury and Osteoarthritis Outcome Score (KOOS) and IKDC subjective score were used which were validated to evaluate ACL injury patients (44). We found that patients with concomitant LMPRT showed greater pivot shift grade and poorer subjective outcomes (KOOS and IKDC subjective score) than patients with isolated ACL preoperatively. However, the differences were not significant at 2 years postoperatively (unpublished observation). Our short-term results of LMPRT repair in ACLR patients were equivalent to those reported in previous studies (35,36).
Arthroscopic centralization for LM extrusion
A literature review of arthroscopic centralization
No surgical technique for LM extrusion was seen after meniscectomy or in the discoid LM. We developed an arthroscopic centralization technique to reduce meniscal extrusion. Herein, we describe the indications, surgical techniques, rehabilitation protocols, clinical outcomes, and biomechanical effects of this technique based on published articles searched by PubMed.
Indications for arthroscopic centralization
Original indication
The original indications for arthroscopic centralization were a symptomatic knee (pain, swelling, and/or catching) despite sufficient conservative treatment, with OA (Kellgren-Lawrence grades 0 to 2) in the lateral compartment, or after partial meniscectomy of the LM. The extrusion of the midbody of the LM had been confirmed preoperatively on coronal view of an MRI (24). Meniscal extrusion was determined by measuring the distance between the most peripheral aspect of the meniscus and the border of the tibia (excluding osteophytes) on coronal views of the MRI (45). This technique is also applicable in cases of symptomatic torn discoid meniscus (pain, swelling, and/or catching) after conservative treatment. In such cases, centralization is performed concomitantly with saucerization to prevent extrusion. Extrusion of the LM was defined as an extrusion of ≥3 mm based on MRI measurements.
Expanded indications
Recently, the indications for this technique have been expanded to include advanced lateral compartment OA through the development of a new meniscoplasty technique. This technique is for patients with lateral compartment OA due to LM defects. The released meniscotibial capsule is advanced and centralized onto the rim of the lateral tibial plateau to reform a meniscus-like configuration. Regeneration of meniscus-like tissue is expected (46,47). Indications for meniscoplasty due to capsular advancement include symptomatic knee (pain, swelling, and/or catching) with neutral alignment (mechanical axis <60%) after sufficient conservative treatment with OA (Kellgren-Lawrence grade 3–4) in the lateral compartment due to LM defects. This is regardless of a history of meniscectomy, and in patients who are too young to undergo arthroplasty. This is also for patients who are active and desire to continue sports activity. In patients with valgus knee alignment, distal femoral closed osteotomy is performed concomitantly. In cases of meniscal extrusion due to LMPRT or radial tear, if a repair would be insufficient to restore hoop function because of the chronic and/or degenerative status of the torn site, arthroscopic centralization is considered for augmentation of an anatomical repair. Centralization is also effective for augmentation of MMPRT repairs (48-51) as well as for LM allograft transplantation (52). This includes improvements in load distribution function and reduction of meniscus extrusion.
Surgical technique of arthroscopic centralization
This technique has been described previously (24,29). A standard arthroscopic examination can be performed via routine anteromedial and anterolateral portals. Other ligament and cartilage injuries should be managed according to the injury status. The LM status was evaluated, and extrusion of the meniscus was confirmed (Figure 3A). The size of the osteophytes, both at the lateral femoral condyle and the lateral tibial plateau, were also evaluated. A midlateral portal was made 1 cm proximal to the LM and 1 cm anterior to the popliteal hiatus under an arthroscopic view from the anterolateral portal (Figure 3B,3C). If osteophytes were present on both the femoral and tibial sides, they were resected using an osteotome and/or a motorized abrader through the midlateral and anterolateral portals. The resected area on the femoral side was coagulated to prevent regrowth of the osteophytes. The tibial side was left uncoagulated to ensure adhesion of the meniscotibial capsule to the tibia. The meniscotibial capsule was released from the tibia from anterior to posterior using a rasp to mobilize the lateral capsule (Figure 3D). The extruded meniscus was confirmed to be easily reduced (or in cases with meniscal defects, the released capsule was easily and sufficiently advanced to form a meniscus-like configuration) by pulling the meniscus centrally using a grasper. Subsequently, the centralization technique was performed. A soft anchor loaded with a No. 1 suture (JuggerKnot Soft Anchor; Zimmer-Biomet, Warsaw, IN, USA, Q-Fix Anchor; Smith & Nephew Endoscopy, or FiberTak Soft Anchor, Arthrex) was inserted into the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus (Figure 3E). A micro suture lasso small curve with a Nitinol wire loop (Arthrex) was then inserted through the midlateral portal. The tip of the Micro SutureLasso penetrated the capsule from superior to inferior direction (Figure 3F). One strand of the suture was passed into the wire loop, and the other limb of the wire loop was pulled to pass the suture from the inferior to the superior direction (Figure 3G). The same procedure was repeated for another strand of the suture to create a mattress suture configuration. An additional soft anchor was inserted on the lateral edge of the lateral tibial plateau 1 cm anterior to the first anchor. The same procedure was then repeated. The sutures were tied through the midlateral portal using a self-locking sliding knot (Figure 3H). The extruded meniscus was centralized onto the rim of the lateral tibial plateau (Figure 3I). Figure 4 schematically demonstrates the surgical technique for arthroscopic centralization. The tips and pitfalls of this technique are listed in Table 2. The rehabilitation protocol has been described previously (29). Range-of-motion exercises without restriction are encouraged immediately after surgery. Partial weight-bearing with a knee immobilizer and crutches were allowed for the first 4 weeks. After 4 weeks, partial weight-bearing without the knee immobilizer was permitted with progression to full weight-bearing at 6 weeks. Deep squatting over 90° was permitted after three months. Running was allowed at three months. Patients progressed to full activity after six months.
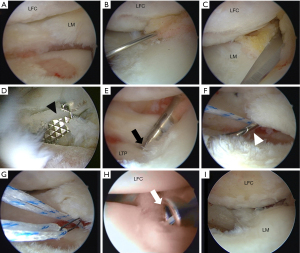
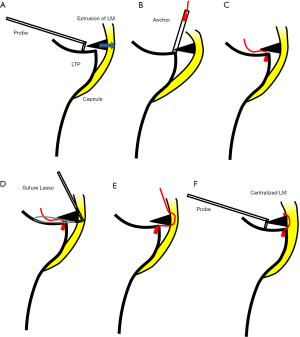
Table 2
| Tips | Pitfalls |
|---|---|
| The appropriate placement of the midlateral portal is essential. Use a spinal needle to check portal placement before creation | Instruments such as the rasp and suture passer should be handled carefully to avoid chondral damage |
| Use an arthroscopic rasp to release the meniscotibial capsule to mobilize the LM centrally | Anchors on the osteophyte or on weightbearing areas of the tibial plateau must be avoided and should be inserted at the rim of lateral tibial plateau |
| The resection of osteophytes is very important (especially on the tibial side) to reduce the extruded meniscus | The Micro SutureLasso should penetrate the capsule at the margin between the meniscus and the capsule during the centralization procedure. Penetration of the meniscus body would result in overconstrainment of the LM |
LM, lateral meniscus.
Clinical outcomes of arthroscopic centralization
Arthroscopic centralization of the extruded LM obtained satisfactory clinical results as indicated by KOOS or Lysholm scores at the 2-year follow-up. MRI evaluation showed a significant reduction in meniscus extrusion width. The radiographic lateral joint space width in a standing 45-degree flexion posteroanterior view was also significantly increased at 3 months post-surgery and was maintained for 2 years (29).
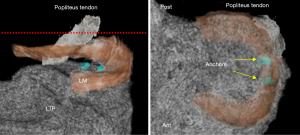
Three-dimensional reconstructed (3D recon) MRI has been reported to quantitatively evaluate the meniscus in more detail (13,53,54). Wenger et al. (12) used 3D recon MRI to analyze the three-dimensional meniscal morphology and position in patients with knee OA. We analyzed the effects of arthroscopic centralization on the degree of LM extrusion using 3D recon MRI (Figures 5,6) in five patients (average age: 32 years, range, 15–47 years) who had an extruded LM from partial meniscectomy or meniscoplasty of the discoid meniscus. Each patient underwent MRI prior to and one year post-surgery. MR images were acquired using a proton density-weighted sequence using a 3.0T scanner (Achieva, Philips Medical System, Andover, MA, USA) and an eight-channel knee coil (Philips Medical System). For 3D recon images, Ziostation2 software (Ziosoft Inc., Tokyo, Japan) was used. Segmentation of the external surface of the LM and tibia was performed in the coronal view (47). The length (mm) and area (mm2) of the portion of the LM extrusion and the meniscus coverage of the tibial plateau (mm2) were quantified. The meniscal extrusion lengths (Figure 6C-6E) and area (Figure 6F-6H) at 1-year postoperatively were significantly lower than those measured preoperatively. Additionally, meniscus coverage (Figure 6I-6K) at 1-year was significantly higher than that prior to the operation. These data further support the concept that the arthroscopic centralization technique is a promising option for the treatment of extruded LM.

Biomechanics of centralization
The biomechanical analyses of the centralization procedure for extruded LM with posterior root deficiency were performed using a porcine model. Ozeki et al. (25) reported that the centralization procedure restored the load distribution to a value closer to that of the normal knee joint at 45° of knee flexion (Figure 7). Additionally, further analysis demonstrated that this effect was also observed at various knee flexion positions at 30°, 60°, and 90° (26). Nakamura et al. (27) demonstrated that centralization improved the residual rotational laxity of the ACL-reconstructed knee accompanied by middle segment LM defects in porcine knees, as evaluated by a robotic testing system. These biomechanical studies further strengthened the rationale for the centralization procedure.

Discussion
The treatment of LMPRT has received increased attention among surgeons who perform ACLR. Several biomechanical studies have revealed the efficacy of LMPRT repair for decreasing the tibiofemoral contact pressure and restoring the kinematics of the knee joint (20,55). To restore knee function, the LMPRT should be repaired as completely as possible. LMPRT is often accompanied by ACL injury. Therefore, surgeons should prepare the necessary instruments for LMPRT repair for all ACL reconstruction surgeries. Specific MRI signs and careful arthroscopic observation will ensure that the diagnosis of LMPRT is not overlooked. Pull-out techniques can provide adequate fixation strength and will result in favorable clinical outcomes.
The centralization technique has been proven to reduce meniscal extrusion and has beneficial effects on load distribution and joint stability (25-27). In a clinical study, arthroscopic centralization of the extruded LM improved patient-reported outcomes and meniscus extrusion width 2 years post-surgery. This new technique has expanded the surgical indications for addressing secondary OA caused by meniscal defects and achieved satisfactory clinical and radiographic outcomes (46,47).
A limitation of this narrative review is that the literature includes laboratory studies or low-level evidence clinical studies (case series or cohort study). So far, there have been no high-level evidence clinical trials such as randomized control trials (RCTs) regarding LMPRT repair or arthroscopic centralization. Additionally, as these techniques are relatively new, long-term clinical results remain controversial. Further studies with higher evidence levels and long-term follow-up are required to confirm the efficacy of LMPRT repair and arthroscopic centralization.
Conclusions
To restore knee function, LMPRT should be repaired as much as possible during ACLR. The centralization technique is a promising surgical treatment for extruded lateral menisci due to meniscectomy and discoid meniscus.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-112/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-112/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-112/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. HK serves as an unpaid editorial board member of Annals of Joint from September 2019 to August 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res 1975;184-92. [Crossref] [PubMed]
- Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand 1980;51:871-9. [Crossref] [PubMed]
- Musahl V, Citak M, O'Loughlin PF, et al. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2010;38:1591-7. [Crossref] [PubMed]
- Katakura M, Horie M, Watanabe T, et al. Effect of meniscus repair on pivot-shift during anterior cruciate ligament reconstruction: Objective evaluation using triaxial accelerometer. Knee 2019;26:124-31. [Crossref] [PubMed]
- Ambra LF, Mestriner AB, Ackermann J, et al. Bone-Plug Versus Soft Tissue Fixation of Medial Meniscal Allograft Transplants: A Biomechanical Study. Am J Sports Med 2019;47:2960-5. [Crossref] [PubMed]
- Choi NH. Radial displacement of lateral meniscus after partial meniscectomy. Arthroscopy 2006;22:575.e1-4. [Crossref] [PubMed]
- Kijowski R, Woods MA, McGuine TA, et al. Arthroscopic partial meniscectomy: MR imaging for prediction of outcome in middle-aged and elderly patients. Radiology 2011;259:203-12. [Crossref] [PubMed]
- Magee T. MR findings of meniscal extrusion correlated with arthroscopy. J Magn Reson Imaging 2008;28:466-70. [Crossref] [PubMed]
- Matsuo T, Kinugasa K, Sakata K, et al. Post-operative deformation and extrusion of the discoid lateral meniscus following a partial meniscectomy with repair. Knee Surg Sports Traumatol Arthrosc 2017;25:390-6. [Crossref] [PubMed]
- Puig L, Monllau JC, Corrales M, et al. Factors affecting meniscal extrusion: correlation with MRI, clinical, and arthroscopic findings. Knee Surg Sports Traumatol Arthrosc 2006;14:394-8. [Crossref] [PubMed]
- Stehling C, Luke A, Stahl R, et al. Meniscal T1rho and T2 measured with 3.0T MRI increases directly after running a marathon. Skeletal Radiol 2011;40:725-35. [Crossref] [PubMed]
- Wenger A, Wirth W, Hudelmaier M, et al. Meniscus body position, size, and shape in persons with and persons without radiographic knee osteoarthritis: quantitative analyses of knee magnetic resonance images from the osteoarthritis initiative. Arthritis Rheum 2013;65:1804-11. [Crossref] [PubMed]
- Bloecker K, Guermazi A, Wirth W, et al. Tibial coverage, meniscus position, size and damage in knees discordant for joint space narrowing - data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 2013;21:419-27. [Crossref] [PubMed]
- Sharma L, Chmiel JS, Almagor O, et al. Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol 2014;66:1811-9. [Crossref] [PubMed]
- Willinger L, Foehr P, Achtnich A, et al. Effect of Lower Limb Alignment in Medial Meniscus-Deficient Knees on Tibiofemoral Contact Pressure. Orthop J Sports Med 2019;7:2325967118824611. [Crossref] [PubMed]
- Berthiaume MJ, Raynauld JP, Martel-Pelletier J, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis 2005;64:556-63. [Crossref] [PubMed]
- Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc 2015;23:112-8. [Crossref] [PubMed]
- Minami T, Muneta T, Sekiya I, et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients. Knee Surg Sports Traumatol Arthrosc 2018;26:1174-81. [PubMed]
- Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2015;43:905-11. [Crossref] [PubMed]
- LaPrade CM, Jansson KS, Dornan G, et al. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am 2014;96:471-9. [Crossref] [PubMed]
- Forkel P, von Deimling C, Lacheta L, et al. Repair of the lateral posterior meniscal root improves stability in an ACL-deficient knee. Knee Surg Sports Traumatol Arthrosc 2018;26:2302-9. [Crossref] [PubMed]
- Schillhammer CK, Werner FW, Scuderi MG, et al. Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med 2012;40:2604-9. [Crossref] [PubMed]
- Tang X, Marshall B, Wang JH, et al. Lateral Meniscal Posterior Root Repair With Anterior Cruciate Ligament Reconstruction Better Restores Knee Stability. Am J Sports Med 2019;47:59-65. [Crossref] [PubMed]
- Koga H, Muneta T, Yagishita K, et al. Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech 2012;1:e209-12. [Crossref] [PubMed]
- Ozeki N, Koga H, Matsuda J, et al. Biomechanical analysis of the centralization procedure for extruded lateral menisci with posterior root deficiency in a porcine model. J Orthop Sci 2020;25:161-6. [Crossref] [PubMed]
- Kubota R, Koga H, Ozeki N, et al. The effect of a centralization procedure for extruded lateral meniscus on load distribution in porcine knee joints at different flexion angles. BMC Musculoskelet Disord 2020;21:205. [Crossref] [PubMed]
- Nakamura T, Linde MA, Marshall BD, et al. Arthroscopic centralization restores residual knee laxity in ACL-reconstructed knee with a lateral meniscus defect. Knee Surg Sports Traumatol Arthrosc 2019;27:3699-704. [Crossref] [PubMed]
- Ozeki N, Muneta T, Kawabata K, et al. Centralization of extruded medial meniscus delays cartilage degeneration in rats. J Orthop Sci 2017;22:542-8. [Crossref] [PubMed]
- Koga H, Muneta T, Watanabe T, et al. Two-Year Outcomes After Arthroscopic Lateral Meniscus Centralization. Arthroscopy 2016;32:2000-8. [Crossref] [PubMed]
- Minami T, Koga H, Sekiya I, et al. Posteriorly inserted anterior cruciate ligament in knees with discoid lateral meniscus corresponding to bony morphological characteristics of femoral lateral condyle. J Orthop Sci 2018;23:350-5. [Crossref] [PubMed]
- Vaquero-Picado A, Rodríguez-Merchán EC. Arthroscopic repair of the meniscus: Surgical management and clinical outcomes. EFORT Open Rev 2018;3:584-94. [Crossref] [PubMed]
- Krych AJ, Wu IT, Desai VS, et al. High Rate of Missed Lateral Meniscus Posterior Root Tears on Preoperative Magnetic Resonance Imaging. Orthop J Sports Med 2018;6:2325967118765722. [Crossref] [PubMed]
- Asai K, Nakase J, Oshima T, et al. Lateral meniscus posterior root tear in anterior cruciate ligament injury can be detected using MRI-specific signs in combination but not individually. Knee Surg Sports Traumatol Arthrosc 2020;28:3094-100. [Crossref] [PubMed]
- Kamatsuki Y, Furumatsu T, Fujii M, et al. Complete tear of the lateral meniscus posterior root is associated with meniscal extrusion in anterior cruciate ligament deficient knees. J Orthop Res 2018;36:1894-900. [Crossref] [PubMed]
- Ahn JH, Lee YS, Yoo JC, et al. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy 2010;26:67-75. [Crossref] [PubMed]
- Anderson L, Watts M, Shapter O, et al. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy 2010;26:1625-32. [Crossref] [PubMed]
- Pan F, Hua S, Ma Z. Surgical treatment of combined posterior root tears of the lateral meniscus and ACL tears. Med Sci Monit 2015;21:1345-9. [Crossref] [PubMed]
- Okazaki Y, Furumatsu T, Kamatsuki Y, et al. Transtibial pullout repair of the lateral meniscus posterior root tear combined with anterior cruciate ligament reconstruction reduces lateral meniscus extrusion: A retrospective study. Orthop Traumatol Surg Res 2020;106:469-73. [Crossref] [PubMed]
- Zhuo H, Pan L, Xu Y, et al. Functional, Magnetic Resonance Imaging, and Second-Look Arthroscopic Outcomes After Pullout Repair for Avulsion Tears of the Posterior Lateral Meniscus Root. Am J Sports Med 2021;49:450-8. [Crossref] [PubMed]
- Song HS, Bae TY, Park BY, et al. Repair of a radial tear in the posterior horn of the lateral meniscus. Knee 2014;21:1185-90. [Crossref] [PubMed]
- Tsujii A, Yonetani Y, Kinugasa K, et al. Outcomes More Than 2 Years After Meniscal Repair for Radial/Flap Tears of the Posterior Lateral Meniscus Combined With Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2019;47:2888-94. [Crossref] [PubMed]
- Tsujii A, Amano H, Tanaka Y, et al. Second look arthroscopic evaluation of repaired radial/oblique tears of the midbody of the lateral meniscus in stable knees. J Orthop Sci 2018;23:122-6. [Crossref] [PubMed]
- Pache S, Aman ZS, Kennedy M, et al. Meniscal Root Tears: Current Concepts Review. Arch Bone Jt Surg 2018;6:250-9. [PubMed]
- Rodriguez-Merchan EC. Knee instruments and rating scales designed to measure outcomes. J Orthop Traumatol 2012;13:1-6. [Crossref] [PubMed]
- Gale DR, Chaisson CE, Totterman SMS, et al. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthritis and Cartilage 1999;7:526-32. [Crossref] [PubMed]
- Koga H, Nakamura T, Katagiri H, et al. Two-Year Outcomes After Meniscoplasty by Capsular Advancement With the Application of Arthroscopic Centralization Technique for Lateral Compartment Knee Osteoarthritis. Am J Sports Med 2020;48:3154-62. [Crossref] [PubMed]
- Nakagawa Y, Muneta T, Watanabe T, et al. Arthroscopic centralization achieved good clinical improvements and radiographic outcomes in a rugby player with osteoarthritis after subtotal lateral meniscectomy: A case report. J Orthop Sci 2020;25:537-43. [Crossref] [PubMed]
- Daney BT, Aman ZS, Krob JJ, et al. Utilization of Transtibial Centralization Suture Best Minimizes Extrusion and Restores Tibiofemoral Contact Mechanics for Anatomic Medial Meniscal Root Repairs in a Cadaveric Model. Am J Sports Med 2019;47:1591-600. [Crossref] [PubMed]
- Koga H, Watanabe T, Horie M, et al. Augmentation of the Pullout Repair of a Medial Meniscus Posterior Root Tear by Arthroscopic Centralization. Arthrosc Tech 2017;6:e1335-9. [Crossref] [PubMed]
- Ozeki N, Seil R, Krych AJ, et al. Surgical treatment of complex meniscus tear and disease: state of the art. J ISAKOS 2021;6:35-45. [Crossref] [PubMed]
- Nakamura R, Takahashi M, Kuroda K, et al. Suture Anchor Repair for a Medial Meniscus Posterior Root Tear Combined With Arthroscopic Meniscal Centralization and Open Wedge High Tibial Osteotomy. Arthrosc Tech 2018;7:e755-e761. [Crossref] [PubMed]
- Masferrer-Pino A, Monllau JC, Abat F, et al. Capsular fixation limits graft extrusion in lateral meniscal allograft transplantation. Int Orthop 2019;43:2549-56. [Crossref] [PubMed]
- Sekiya I, Koga H, Otabe K, et al. Additional Use of Synovial Mesenchymal Stem Cell Transplantation Following Surgical Repair of a Complex Degenerative Tear of the Medial Meniscus of the Knee: A Case Report. Cell Transplant 2019;28:1445-54. [Crossref] [PubMed]
- Vangsness CT Jr, Farr J 2nd, Boyd J, et al. Adult human mesenchymal stem cells delivered via intra-articular injection to the knee following partial medial meniscectomy: a randomized, double-blind, controlled study. J Bone Joint Surg Am 2014;96:90-8. [Crossref] [PubMed]
- Perez-Blanca A, Espejo-Baena A, Amat Trujillo D, et al. Comparative Biomechanical Study on Contact Alterations After Lateral Meniscus Posterior Root Avulsion, Transosseous Reinsertion, and Total Meniscectomy. Arthroscopy 2016;32:624-33. [Crossref] [PubMed]
Cite this article as: Nakagawa Y, Ozeki N, Koga H. A narrative review of lateral meniscus root tears and extrusion: techniques and outcomes. Ann Joint 2022;7:15.


