
The hypermobile and unstable lateral meniscus: a narrative review of the anatomy, biomechanics, diagnosis and treatment options
Introduction
In contrast to the more stable medial meniscus, the lateral meniscus (LM) has less stabilizers at its posterolateral aspect (1,2). The important stabilizers of the posterior LM are the popliteomeniscal fascicles (PMF), the posterior capsule, the meniscofemoral ligaments (MFL) and the posterior meniscotibial ligament (MTL), which are divided by a bare area, the popliteal hiatus (2-8). Atraumatic insufficiency or rupture of one of these key structures may have a high impact on the mobility of the LM and can lead to an unstable, hypermobile LM (7,9-13). Lateral meniscus hypermobility (LMH) can cause lateral knee pain and mechanical symptoms as locking or giving way (6,7,14-18). In a stable knee, LMH is a rare condition. Its prevalence be it isolated or in association with cruciate injuries remains unknown. To date, only case reports and series are available and prospective studies on LMH are needed. However, a PMF rupture is reported in up to 25% of patients with an anterior cruciate ligament (ACL) injury and in up to 80% of patients with a grade 3 posterolateral corner injury (9,19,20). Since the PMF, MFL and MTL play a role in the rotational and anteroposterior knee stability, it may be crucial to repair these structures during ligament reconstruction (5,8,9,20-22).Both isolated LMH or LMH associated with ACL injury are often unrecognized, since the patient’s history, clinical tests and magnetic resonance imaging (MRI) are unspecific (6,14,15,17,18,23,24). A dynamic arthroscopic evaluation remains the gold standard to diagnose LMH (6,15,25,26). Therefore, it is up to the surgeon to interpret the various finding before a knee arthroscopy is proposed to the patient. Knee surgeons should be aware and recognize isolated or associated LMH. The purpose of this review is to improve the awareness of lateral meniscal hypermobility by describing its relevant anatomy, biomechanics, pathophysiology, imaging and arthroscopic findings as well as the treatment options. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-9/rc).
Methods
This is a narrative overview of the literature synthesizing current knowledge about the hypermobile LM. Anatomy, biomechanics, diagnosis and treatment of this entity was of particular interest for this review. Literature was retrieved from PubMed database, hand searches and cross-reference checking.
Anatomy
The anatomy of the LM and its attachments remains a topic of debate (2-5,27-29). The area of interest in LMH runs from just lateral to the popliteal hiatus to just medial from the posterior root of the LM (2-8). The popliteus tendon (PT) splits this area when it passes through the popliteal hiatus transforming from an intra-articular into an extra-articular structure (2,3,9). The PT/muscle complex has multiple attachments to the tibia, fibular head and the joint capsule as well as to the LM via a complex of fascicles (4,30). These PMF are together with the posterior capsule, the MTL and MFL the main stabilizers of the posterolateral meniscus (2,4,8,9). Figure 1 shows an illustration of these anatomic attachments to the LM.
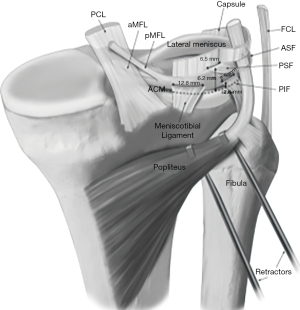
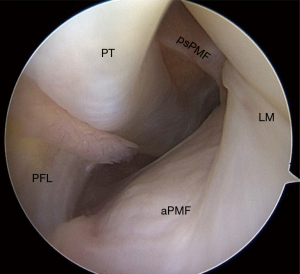
The reported number of PMF is variable and many anatomical variations have been described (2-5,11,23,28-31). However, most studies identified three PMF; an anterior- (a-), a posterosuperior- (ps-) and a posteroinferior- (pi-) PMF. Although previous studies agreed on an anteroinferior fascicle (3,9), more recent studies quantified it as an anterosuperior fascicle (2,29,32). To avoid any confusion, it will be described in this review as the anterior PMF (aPMF).
The aPMF originates lateral from the PT on the mid height of the lateral aspect of the LM and runs inferoposterior where it blends in on the PT (2,29). Some authors describe the aPMF as the floor of the popliteal hiatus as it forms a sling around the PT by running from an anterosuperior to an inferoposterior direction (3,9). The aPMF is the anterior border of the superior and inferior popliteal hiatus (2,4).
The psPMF originates medial from the PT on the superior margin of the LM (2,3,9,28,29). It courses directly posteriorly where it attaches to the PT (2,3,9,28,29). The aPMF and piPMF form together a hoop-like structure, called the superior popliteal hiatus (2,5).
The piPMF is inconsistently reported in anatomic studies (2,3,5,9,28,32). The piPMF originates medial from the PT on the inferior margin of the LM, it then courses inferior to join the popliteus muscle aponeurosis where it has some attachments to the tibia (2,4).
The popliteofibular ligament runs from the fibular head and inserts on the PT (5,29). Here it is in close contact with the PMF (5,29). The anterior part of the popliteofibular ligament has attachments to the aPMF and, while running along the aPMF, to the LM (5,9). Some authors refer to this direct connection between the fibular head and LM as the meniscofibular ligament (33).
Medially from the psPMF, the posterior capsule attaches on the superior margin of the LM (2).
There are two MFL, an anterior (aMFL) and posterior (pMFL) (2,34,35). A cadaveric study of 84 knees, showed that 93% of the knees have at least one MFL and in 50% both MFL were present (35). The aMFL, also known as the ligament of Humphrey, originates distal and anterior to the posterior cruciate ligament (PCL) footprint on the medial femoral condyle, runs anterior to the PCL and then inserts on the LM just lateral from the posterior root (2,34,35). The pMFL, also known as the ligament of Wrisberg, originates proximal and posterior to the PCL footprint on the medial femoral condyle, runs posterior to the PCL and then inserts on the LM lateral from the aPMF (2,34,35).
Two MTL are described, one lateral, anterior from the aPMF and one posterior, lateral from the posterior LM root (2,4,5,27,36). Both MTLs have been named coronary ligaments (4,5,29,36). The lateral MTL is part of the anterolateral ligament complex, it runs from the lateral side of the LM and inserts on the tibia anterior to the popliteal hiatus (5). The posterior MTL originates just lateral from the PCL on the tibia and inserts on the inferior margin of the posterior horn of the LM (2,5). It is reinforced by aponeurotic attachment of the popliteus muscle (2,5).
The inferior popliteal hiatus is the space between the posterior MTL and the anterior part of the aPMF (2). In contrast to the more stable medial meniscus, which has multiple stabilizers at its posteromedial aspect, the PMF and posterolateral capsule are the only stabilizers of the LM at the inferior popliteal hiatus area (1,2). This may explain why the LM is more mobile than the medial meniscus (2). Furthermore, rupture of one of these key structures may have a high impact on the stability of the LM.
A congenital deficiency of the PMF and the posterior MTL is known as the Wrisberg variant of the discoid meniscus, and is a described cause of LMH (12,16,37). In this variant, the MTL or root attachment is/are absent, but the LM presents otherwise a near normal shape (12,16,37).
Biomechanics
The PMF and the popliteus musculotendinous unit act together to restrain varus/valgus stress and coupled external rotation with posterior displacement (5,9,21,22). However, cutting the PMF in a PCL deficient knee did not show a significant increase in varus/valgus, anteroposterior and rotational stability (22). The influence of PMF rupture on the stability of the knee may therefore be minimal in comparison to the other posterolateral structures (5,22). They do have an important function in preventing intraarticular entrapment or impingement of the LM between the femoral condyle and the tibial plateau during flexion and extension movements, and have a great influence on the stability of the LM (5,8,9,20,22). The MFL may antagonize the posterior/lateral pull of the PMF and popliteus musculotendinous unit, by pulling the LM anterior/medial during knee motion and hereby controlling LM motion (8,34,38,39). Furthermore, the MFL are found to contribute to rotational and anteroposterior stability of the knee, especially when the PCL and/or the posterior root is ruptured (40-43). However, in contrast to the PMF, their biomechanical influence on the instability of the LM is not documented.
In 1997, Simonian et al. conducted a cadaveric biomechanical study in which they evaluated the LM mobility using a 10 N load before and after sequential sectioning of the a- and psPMF (8). After sectioning the aPMF, they demonstrated an average significant increase of anterior motion of the LM from 3.6 to 5.4 mm (8). After cutting both the a- and psPMF, they reported a significant increase to 6.4 mm of this anterior motion (8). Compared to the intact state, the LM anterior mobility increased significantly with 2.8 mm or 78% (8). Several anatomic studies evaluated the aPMF as the most robust of the PMF and concluded that the aPMF may be the most important PMF in stabilizing the LM (27-29). Furthermore, Suganuma et al. suggested that an abnormal or absent psPMF puts the knee at risk for instability of the LM, but a lesion of the aPMF is the essential lesion to allow the LM to become unstable (24). In agreement, Stäubli et al. reported that an isolated lesion of one PMF probably plays a minimal role in LMH instability (9). However, combined extended lesions of the LM stabilizers lead to a loss of LM hoop tension and consequently, to LMH (9,24). These extended lesions can include rupture of the posterior MTL (7,16). The posterior MTL provides resistance to hyperextension and posterolateral rotation of the knee (5). Consequently, rupture of the posterior MTL may influence knee and LM stability (5).To our knowledge, the biomechanical attribution of the posterior MTL to LMH has not yet been investigated.
Pathophysiology, symptoms and clinical findings
LMH may be congenital, or occur after a posttraumatic tear of one or several PMF, the posterior MTL and/or one or both MFL with or without associated ligament injury (7,9-13). Especially in young patients with bilateral atraumatic symptoms, clinicians should be conscious of a Wrisberg variant discoid LM (6,12,16,44). From an anamnestic point, a congenital variant may be difficult to distinguish from isolated posttraumatic LMH without associated ligament injury since trauma leading to this instability may be minimal and patients may often not recall any traumatic mechanism (6,9,45). Furthermore, posttraumatic LMH can be the result of repeated microtraumas (6,9,45).
The prevalence of PMF lesions in association with ligamentous knee injury is high, however may be often missed due to the focus on the ligamentous injury and its management. Stäubli et al. reported an isolated aPMF or psPMF tear in 25% and 7.5% of patients with an acute ACL injury and in respectively 25% and 3.6% of those with a chronic ACL injury (9). Rupture of both PMF has been reported in 25% and 21.4% of patients with acute and chronic ACL injury (9).In agreement with these findings, Temponi et al. recently showed a prevalence of 17.3% and 11.1% of an aPMF or a psPMF tear in ACL injured patients (19)Furthermore, Lee et al. found that the most common posterolateral corner structure injured in association with an ACL injury is the aPMF followed by the psPMF (13). If a grade 3 posterolateral corner injury is present with or without ACL injury, the aPMF, the psPMF and posterior MTL are ruptured in 60% to 85% of the cases (20).
As the posterior lateral root tear and PCL is commonly seen in association with ACL and posterolateral corner injury, the incidence of MFL rupture, which are in close relation with these structures, may be common as well (46,47). However, their presence, absence or rupture is not reported in these injuries.
The different causes of LMH lead to a variable spectrum of patients history, presentation and symptoms (6). In a stable knee scenario, common complaints include pain and mechanical symptoms such as clicking, locking and a giving way sensation in the lateral compartment (6,14,15). Locking typically occurs in deep flexion and patients may have these symptoms for years (6,45). Symptoms may even be misinterpreted as patellar instability, as reported by Arendt et al. (17). In a knee with an associated ligamentous injury, the patient exhibit symptoms of acute knee injury which often masquerade the symptoms of LMH.
LaPrade et al. described the “figure of 4” test as a diagnostic tool for LMH (15). The test consists of placing the affected knee in flexion, varus and external rotation (a “figure of 4” position), which may induce medial displacement of the LM when the PFM are ruptured (15).The test is considered positive when pain occurs that reproduces the patients symptoms at the lateral joint line (15). However, it is important to note that the test has only been validated in 6 patients (15).
MRI
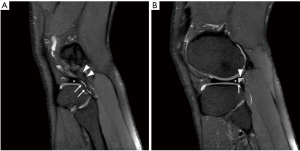
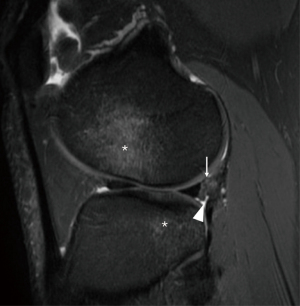
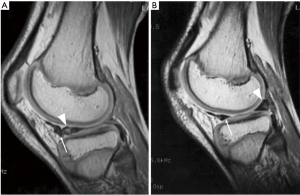
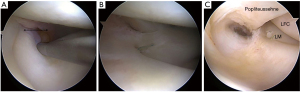
The anatomy and visualization of the PMF, MFL and MTL on MRI is still debated. In uninjured knees, Johnson and De Smet visualized the a- and psPMF in 97.0% of the patients (31), whereas Sakai et al. could visualize the aPMF and the psPMF in respectively 94.1% and 88.2%, in a total of 34 cases (23). The piPMF is less described on MRI. In a cadaveric MRI study involving 10 knees, Peduto et al. identified the a- and psPMF in all specimens, whereas the piPMF was only identified in 4 cases (48). Figure 2 shows the normal anatomy of the PMF on MRI. To improve its visualization on MRI, Sakai et al. recommends MRI to perform T2 weighted 45° oblique coronal images with a 3-mm slice thickness (23). However, visualization of PMF alterations on MRI does not necessarily imply LMH (23,24). Suganuma et al. evaluated 238 MRIs from 142 patients with (unilateral) atraumatic knee pain who underwent bilateral knee MRIs (24). LMH was confirmed in 16 (21%) of the 76 joints who underwent arthroscopic evaluation (24). They found abnormal psPMF on MRI in 41% and abnormal aPMF in 26% of the control group (222 knees) and in all patients with LMH (16 knees) (24). At the same time, just as alterations in PMF anatomy do not necessarily imply LMH, a normal MRI does not necessarily rule out LMH (17).Retrospective evaluation of MRIs of unstable lateral menisci did not always show alterations of the PMF (17,18). Ahn et al. reported that in a retrospective evaluation of 17 out of 24 patients operated for LMH, the MRI findings showed no abnormalities (18). Consequently, clinicians cannot deduct from an MRI if the LM is hypermobile (24). However, several indirect signs for the LMH have been highlighted, such as discontinuity of the PMF (Figure 3), rupture or absence of the posterior MTL and a water-signal between the posterior capsule and the posterior horn of the LM (11,23,44). Recently, widening of the popliteal hiatus on MRI has been described as a sign for LMH (49). In certain unusual cases, MRI was performed when the LM was dislocated (Figure 4) (50-52). Rupture or absence of the MFL have not been described as sign of LMH. However, as they are important stabilizers of the LM, they should be evaluated during the MRI workup (8,34,38,39). In an MRI study of 446 knees, Ebrecht et al. found in 70.6% of the cases at least one MFL on MRI (53). The aMFL and pMFL were found on MRI in 21.8% and 53.1% of the cases, respectively. In 4.5% of the MRIs, both ligaments were found. These numbers are markedly lower than the prevalence of the MFL found in cadaver studies (35,53).
The main explanation for the lack of sufficient sensitivity of MRI in the diagnosis of LMH is that LMH is a dynamic pathology and MRI, as a static investigation, may not be fully suited as diagnostic tool. However, if the MRI investigation shows alterations of the PMF, MFL or posterior MTL in the presence of adequate mechanical symptoms, LMH should be highly suspected.
Arthroscopic evaluation
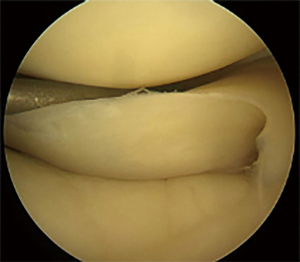
As knee arthroscopy is the only option to properly dynamically evaluate the LM, it currently remains the gold standard for the diagnosis of LMH. The arthroscopic evaluation initially includes a visual inspection of the LM and lateral compartment cartilage as well as the level of opening of the lateral compartment. A “drive-through sign” is present if there is an increased opening of the posterolateral compartment and is a sign of posterolateral corner injury (20). The popliteal hiatus can be observed from the anterior view, especially when there is an increased opening of the lateral compartment. Widening of the popliteal hiatus may indicate LMH (18). The dynamic evaluation for LMH is done by probing and aspiration (with arthroscope or shaver) (7,15,26). Translation of the posterolateral LM by over 50% of the lateral tibial plateau, lateral femoral condyle or “beyond the equator” is considered as unstable (Figure 5) (6,15). In addition, moving the knee from a more flexed to a more extended position during the “figure of 4” position also allows to assess for excessive translation of the LM. If the forward translation is not conclusive, the presence of an osteochondral lesion at the posterior lateral femoral condyle or at the posterior lateral tibia plateau, as a sign of repetitive luxation of the LM, may aid in diagnosing LMH (14,18). For further the assessment of the PMF and posterior TML, a 30° arthroscope can be placed in the lateral gutter, while the knee is slightly flexed and placed in valgus. Here, the superior popliteus hiatus, the PT and the integrity of the a- and psPMF (Figure 6) can be evaluated (9,15). Medial LM subluxation and PMF rupture may be seen by placing varus stress on the knee, by performing anterior traction with a probe or by an anterior aspiration test (9,15,45). Flexing the knee to 90° may allow to advance the arthroscope in the popliteal space, especially when widening is present due to a PMF tear, PT tear or extended posterolateral corner injury (20,55). The possibility to advance the arthroscope until the posterolateral compartment is called a “lateral gutter drive-through sign” and is found in up to 95.5% of the patients with a hypermobile LM (25,55). This allows for visualization of the posterior tibial plateau, posterior lateral femoral condyle, the posterior aspect of the LM, the menisco-capsular attachments, the posterior MTL and the piPMF. Alternatively, the posterolateral compartment can be visualized by advancing the arthroscope through the intercondylar notch.
Treatment and results
Various techniques have been described in the past including open or arthroscopic repair, thermal shrinkage and reconstruction of the PMF (6,7,11,14-18,45,49,56-59).LaPrade and Konowalchuk described an open PMF repair technique in 6 patients after the diagnosis had been made arthroscopically (15). They reported a complete resolution of symptoms at a mean follow-up of 3.8 years (15).However, they suggested that arthroscopic or arthroscopically assisted repair of the PMFs and/or the capsular attachment to the LM may also be successful. Multiple case reports or series have been published on arthroscopic repair (6,7,11,14,16-18,45,49,56,57). Higuchi et al. and Ohtoshi et al. described thermal shrinkage of the popliteal hiatus area until the LM becomes stable as a successful arthroscopic technique (56,57). However, thermal shrinkage has been abandoned in meniscal surgery and may not be the first treatment choice. In more recent literature, authors propose a repair by suturing the LM to the posterior or posterolateral capsule from an anterior view (Figure 7) (6,7,11,16,17,45,49,59). Simonian et al. was the first to report on three cases of successful arthroscopic repairs (11). They did a second look arthroscopy on one of the patients 6 weeks following initial repair due to loss of range of knee motion, showing a stable LM (11).
Steinbacher et al. presented the largest case series in literature of 46 knees in 45 football players (7). They performed an all-inside suture in all cases and placed the first suture just medial to the PT, suturing the LM to the posterior capsule. Consequently, they added sutures medial to the first until the LM was stabilized. In most knees [27/46] 2 sutures were performed. Although 82% returned to play, only 56% returned to the same pre-injury activity level. Three were re-operated: one patient had pain while squatting and the two others suffered from a LM tear. Similar to the repair of a ramp lesion of the medial meniscus, some authors described a repair technique through a posterolateral portal (14,18,60).
In most case series, the surgeons sutured the LM to the capsule without specific repair of the ruptured structure/s. Li et al. and Kamiya et al. did, however, repair the aPMF and/or the psPMF and/or the posterior MTL depending on which one was ruptured (49,59). Their total of 30 patients did not have recurrent mechanical symptoms after a follow-up of at least 24 months (49,59). The LM fixation on the PT is controversial (54). However, in a case series of 200 patients, Ouanezar et al. reported no specific complications following stabilization of LM tears using an all-inside fixation to the PT (61). Suganuma et al. recently proposed an additional surgical technique involving reconstruction of the a- and psPMF (58). In their surgical technique, they pulled an autologous iliotibial band graft through the periphery of the LM and fixed it on the popliteal tendon (58). Results of this technique have not yet been published.
Results of arthroscopic repair from case reports and case series are promising with overall high success rates (6,7,11,14,16-18,45,49). Furthermore, complications of arthroscopic repair were generally rare with reported complications including recurrence of mechanical symptoms, LM meniscal tear, knee stiffness and continued postoperative pain (7,11,18,56). Finally, improving the indication and optimizing the surgical technique, for example by better identification and repair of the injured structures, may further improve the results.
Summary
LMH is a challenging pathology. The diagnosis is difficult due to a lack of specific and distinctive clinical symptoms and clinical tests. Moreover, MRI has a limited sensitivity and specificity in the diagnosis of LMH as it does not allow for a dynamic evaluation. Consequently, the diagnosis of LMH is often delayed or missed. It is up to the clinician to be minded to the diagnosis, especially when assessing knees with persistent lateral related symptoms. Ultimately, the diagnosis is confirmed during knee arthroscopy, when the LM can be mobilized over 50% of the lateral tibial plateau or lateral femoral condyle using probing or aspiration. Treatment involves stabilizing the posterior menisco-capsular complex which can be achieved via an all-inside meniscal suturing technique with satisfactory outcomes and low rates of recurrence.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-9/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-9/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- DePhillipo NN, Moatshe G, Chahla J, et al. Quantitative and Qualitative Assessment of the Posterior Medial Meniscus Anatomy: Defining Meniscal Ramp Lesions. Am J Sports Med 2019;47:372-8. [Crossref] [PubMed]
- Aman ZS, DePhillipo NN, Storaci HW, et al. Quantitative and Qualitative Assessment of Posterolateral Meniscal Anatomy: Defining the Popliteal Hiatus, Popliteomeniscal Fascicles, and the Lateral Meniscotibial Ligament. Am J Sports Med 2019;47:1797-803. [Crossref] [PubMed]
- Cohn AK, Mains DB. Popliteal hiatus of the lateral meniscus. Anatomy and measurement at dissection of 10 specimens. Am J Sports Med 1979;7:221-6. [Crossref] [PubMed]
- Terry GC, LaPrade RF. The posterolateral aspect of the knee: Anatomy and surgical approach. Am J Sports Med 1996;24:732-9. [Crossref] [PubMed]
- Moorman CT, LaPrade RF. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg 2005;18:137-45. [Crossref] [PubMed]
- Van Steyn MO, Mariscalco MW, Pedroza AD, et al. The hypermobile lateral meniscus: a retrospective review of presentation, imaging, treatment, and results. Knee Surg Sports Traumatol Arthrosc 2016;24:1555-9. [Crossref] [PubMed]
- Steinbacher G, Alentorn-Geli E, Alvarado-Calderón M, et al. Meniscal fixation is a successful treatment for hypermobile lateral meniscus in soccer players. Knee Surg Sports Traumatol Arthrosc 2019;27:354-60. [Crossref] [PubMed]
- Simonian PT, Sussmann PS, Van Trommel M, et al. Popliteomeniscal fasciculi and lateral meniscal stability. Am J Sports Med 1997;25:849-53. [Crossref] [PubMed]
- Stäubli HU, Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: Gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy 1990;6:209-20. [Crossref] [PubMed]
- Guimaraes JB, Facchetti L, Schwaiger BJ, et al. Natural evolution of popliteomeniscal fascicle tears over 2 years and its association with lateral articular knee cartilage degeneration in patients with traumatic anterior cruciate ligament tear. Eur Radiol 2018;28:3542-9. [Crossref] [PubMed]
- Simonian PT, Sussmann PS, Wickiewicz TL, et al. Popliteomeniscal fasciculi and the unstable lateral meniscus: Clinical correlation and magnetic resonance diagnosis. Arthroscopy 1997;13:590-6. [Crossref] [PubMed]
- Moser MW, Dugas J, Hartzell J, et al. A hypermobile Wrisberg variant lateral discoid meniscus seen on MRI. Clin Orthop Relat Res 2007;264-7. [Crossref] [PubMed]
- Lee SY, Choi YJ, Park HJ, et al. Types of posterolateral corner injury associated with both bundle and selective-bundle ACL tears. Acta Radiol 2019; Epub ahead of print. [Crossref] [PubMed]
- Shin HK, Lee HS, Lee YK, et al. Popliteomeniscal fascicle tear: diagnosis and operative technique. Arthrosc Tech 2012;1:e101-6. [Crossref] [PubMed]
- LaPrade RF, Konowalchuk BK. Popliteomeniscal fascicle tears causing symptomatic lateral compartment knee pain: Diagnosis by the figure-4 test and treatment by open repair. Am J Sports Med 2005;33:1231-6. [Crossref] [PubMed]
- Garofalo R, Kombot C, Borens O, et al. Locking knee caused by subluxation of the posterior horn of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2005;13:569-71. [Crossref] [PubMed]
- Arendt EA, Fontboté CA, Rohr SR. Displacing lateral meniscus masquerading as patella dislocation. Knee Surg Sports Traumatol Arthrosc 2014;22:2315-9. [Crossref] [PubMed]
- Ahn JH, Lee SH, Kim KI, et al. Arthroscopic meniscus repair for recurrent subluxation of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2018;26:787-92. [Crossref] [PubMed]
- Temponi EF, de Carvalho Júnior LH, Saithna A, et al. Incidence and MRI characterization of the spectrum of posterolateral corner injuries occurring in association with ACL rupture. Skeletal Radiol 2017;46:1063-70. [Crossref] [PubMed]
- LaPrade RF. Arthroscopic evaluation of the lateral compartment of knees with grade 3 posterolateral knee complex injuries. Am J Sports Med 1997;25:596-602. [Crossref] [PubMed]
- Musahl V, Citak M, O’Loughlin PF, et al. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med 2010;38:1591-7. [Crossref] [PubMed]
- Domnick C, Frosch KH, Raschke MJ, et al. Kinematics of Different Components of the Posterolateral Corner of the Knee in the Lateral Collateral Ligament-intact State: A Human Cadaveric Study. Arthroscopy 2017;33:1821-1830.e1. [Crossref] [PubMed]
- Sakai H, Sasho T, Wada YI, et al. MRI of the popliteomeniscal fasciculi. AJR Am J Roentgenol 2006;186:460-6. [Crossref] [PubMed]
- Suganuma J, Mochizuki R, Inoue Y, et al. Magnetic resonance imaging and arthroscopic findings of the popliteomeniscal fascicles with and without recurrent subluxation of the lateral meniscus. Arthroscopy 2012;28:507-16. [Crossref] [PubMed]
- Goto K, Duthon V, Menetrey J. An isolated Posterolateral corner injury with rotational instability and hypermobile lateral meniscus: a novel entity. J Exp Orthop 2020;7:95. [Crossref] [PubMed]
- Jacquet C, Magosch A, Mouton C, et al. The aspiration test: an arthroscopic sign of lateral meniscus posterior horn instability. J Exp Orthop 2021;8:17. [Crossref] [PubMed]
- Diamantopoulos A, Tokis A, Tzurbakis M, et al. The posterolateral corner of the knee: Evaluation under microsurgical dissection. Arthroscopy 2005;21:826-33. [Crossref] [PubMed]
- Sussmann PS, Simonian PT, Wickiewicz TL, et al. Development of the popliteomeniscal fasciculi in the fetal human knee joint. Arthroscopy 2001;17:14-8. [Crossref] [PubMed]
- Masferrer-Pino A, Saenz-Navarro I, Rojas G, et al. The Menisco-Tibio-Popliteus-Fibular Complex: Anatomic Description of the Structures That Could Avoid Lateral Meniscal Extrusion. Arthroscopy 2020;36:1917-25. [Crossref] [PubMed]
- Feipel V, Simonnet ML, Rooze M. The proximal attachments of the popliteus muscle: A quantitative study and clinical significance. Surg Radiol Anat 2003;25:58-63. [Crossref] [PubMed]
- Johnson RL, De Smet AA. MR visualization of the popliteomeniscal fascicles. Skeletal Radiol 1999;28:561-6. [Crossref] [PubMed]
- Zheng J, Xiao Q, Wu Q, et al. Tears of the Popliteomeniscal Fascicles of the Lateral Meniscus: An Arthroscopic Classification. Cartilage 2020; Epub ahead of print. [Crossref] [PubMed]
- Bozkurt M, Elhan A, Tekdemir I, et al. An anatomical study of the meniscofibular ligament. Knee Surg Sports Traumatol Arthrosc 2004;12:429-33. [Crossref] [PubMed]
- Gupte CM, Smith A, McDermott ID, et al. Meniscofemoral ligaments revisited. Anatomical study, age correlation and clinical implications. J Bone Joint Surg Br 2002;84:846-51. [Crossref] [PubMed]
- Amis AA, Gupte CM, Bull AMJ, et al. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 2006;14:257-63. [Crossref] [PubMed]
- Kimura M, Shirakura K, Hasegawa A, et al. Anatomy and pathophysiology of the popliteal tendon area in the lateral meniscus: 1. Arthroscopic and anatomical investigation. Arthroscopy 1992;8:419-23. [Crossref] [PubMed]
- Neuschwander DC, Drez DJ, Finney TP. Lateral meniscal variant with absence of the posterior coronary ligament. J Bone Joint Surg Am 1992;74:1186-90. [Crossref] [PubMed]
- Last RJ. The Popliteus Muscle and the Lateral Meniscus: With a Note on the Attachment of the Medial Meniscus. The Journal of Bone and Joint Surgery 1950;32-B:93-9. [Crossref]
- Yamamoto M, Hirohata K. Anatomical study on the menisco-femoral ligaments of the knee. Kobe J Med Sci 1991;37:209-26. [PubMed]
- Gupte CM, Bull AM, Thomas RD, et al. The meniscofemoral ligaments: secondary restraints to the posterior drawer. Analysis of anteroposterior and rotary laxity in the intact and posterior-cruciate-deficient knee. J Bone Joint Surg Br 2003;85:765-73. [Crossref] [PubMed]
- Lertwanich P, Martins CAQ, Kato Y, et al. Contribution of the meniscofemoral ligament as a restraint to the posterior tibial translation in a porcine knee. Knee Surg Sports Traumatol Arthrosc 2010;18:1277-81. [Crossref] [PubMed]
- Knapik DM, Salata MJ, Voos JE, et al. Role of the Meniscofemoral Ligaments in the Stability of the Posterior Lateral Meniscus Root After Injury in the ACL-Deficient Knee. JBJS Rev 2020;8:e0071. [Crossref] [PubMed]
- Frank JM, Moatshe G, Brady AW, et al. Lateral Meniscus Posterior Root and Meniscofemoral Ligaments as Stabilizing Structures in the ACL-Deficient Knee: A Biomechanical Study. Orthop J Sports Med 2017;5:2325967117695756. [Crossref] [PubMed]
- Zappia M, Reginelli A, Chianca V, et al. MRI of popliteo-meniscal fasciculi of the knee: a pictorial review. Acta Biomed 2018;89:7-17. [PubMed]
- Park JH, Ro KH, Lee DH. Snapping knee caused by a popliteomeniscal fascicle tear of the lateral meniscus in a professional Taekwondo athlete. Orthopedics 2012;35:e1104-7. [Crossref] [PubMed]
- Schlumberger M, Schuster P, Eichinger M, et al. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surg Sports Traumatol Arthrosc 2020;28:2091-8. [Crossref] [PubMed]
- Magosch A, Mouton C, Nührenbörger C, et al. Medial meniscus ramp and lateral meniscus posterior root lesions are present in more than a third of primary and revision ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 2020; Epub ahead of print. [Crossref] [PubMed]
- Peduto AJ, Nguyen A, Trudell DJ, et al. Popliteomeniscal fascicles: Anatomic considerations using MR arthrography in cadavers. AJR Am J Roentgenol 2008;190:442-8. [Crossref] [PubMed]
- Li Z, Zhao H, Dai Z, et al. Widening of the popliteal hiatus on magnetic resonance imaging leads to recurrent subluxation of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc 2020;28:3532-8. [Crossref] [PubMed]
- George M, Wall EJ. Locked knee caused by meniscal subluxation: magnetic resonance imaging and arthroscopic verification. Arthroscopy 2003;19:885-8. [Crossref] [PubMed]
- Nair R, Dubey N. MR Imaging of the Hypermobile Lateral Meniscus of the Knee: A Case Report. Acta Med Acad 2019;48:225-9. [Crossref] [PubMed]
- Lyle NJ, Sampson MA, Barrett DS. MRI of intermittent meniscal dislocation in the knee. Br J Radiol 2009;82:374-9. [Crossref] [PubMed]
- Ebrecht J, Krasny A, Hartmann DM, et al. 3-Tesla MRI: Beneficial visualization of the meniscofemoral ligaments? Knee 2017;24:1090-8. [Crossref] [PubMed]
- Laver L, Hoffmann A, Spalding T, et al. Hypermobiler lateraler Meniskus: Anatomie, Diagnose und Behandlungsoptionen. Arthroskopie 2017;30:100-7. [Crossref]
- Feng H, Zhang H, Hong L, et al. The "lateral gutter drive-through" sign: an arthroscopic indicator of acute femoral avulsion of the popliteus tendon in knee joints. Arthroscopy 2009;25:1496-9. [Crossref] [PubMed]
- Higuchi H, Kimura M, Kobayashi A, et al. A novel treatment of hypermobile lateral meniscus with monopolar radiofrequency energy. Arthroscopy 2004;20:1-5. [Crossref] [PubMed]
- Ohtoshi K, Kimura M, Kobayashi Y, et al. Arthroscopic thermal shrinkage for hypermobile lateral meniscus. Am J Sports Med 2004;32:1297-301. [Crossref] [PubMed]
- Suganuma J, Inoue Y, Tani H, et al. Reconstruction of the Popliteomeniscal Fascicles for Treatment of Recurrent Subluxation of the Lateral Meniscus. Arthrosc Tech 2017;6:e283-90. [Crossref] [PubMed]
- Kamiya T, Suzuki T, Otsubo H, et al. Midterm outcomes after arthroscopic surgery for hypermobile lateral meniscus in adults: Restriction of paradoxical motion. J Orthop Sci 2018;23:1000-4. [Crossref] [PubMed]
- Sonnery-Cottet B, Conteduca J, Thaunat M, et al. Hidden lesions of the posterior horn of the medial meniscus: A systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med 2014;42:921-6. [Crossref] [PubMed]
- Ouanezar H, Blakeney WG, Latrobe C, et al. The popliteus tendon provides a safe and reliable location for all-inside meniscal repair device placement. Knee Surg Sports Traumatol Arthrosc 2018;26:3611-9. [Crossref] [PubMed]
Cite this article as: Beel W, Macchiarola L, Mouton C, Laver L, Seil R. The hypermobile and unstable lateral meniscus: a narrative review of the anatomy, biomechanics, diagnosis and treatment options. Ann Joint 2022;7:14.


