
Concurrent medial and lateral bucket handle meniscal tear repair in a chronic anterior cruciate ligament-deficient knee: a case report
Introduction
Bucket handle meniscus tear (BHMT) can cause symptoms such as knee pain, locking, instability, joint swelling and reduced range of motion (1-3). The incidence of meniscus injuries in patients with anterior cruciate ligament (ACL) tears is as high as 63%, with higher incidence rates in the young, active population (4,5). The evidence suggests that acute ACL tears are associated with lateral meniscus injury, while chronic ACL tears are associated with medial meniscal injury (5). The goal of meniscus repair is to improve symptoms and restore the biomechanics of the knee joint with preservation of the native meniscus (6). As BHMTs tend to occur in young athletes, it is imperative that meniscus repair should be attempted for joint preservation.
We report a case of a young, retired competitive soccer player who had undergone all-inside repair of bicompartmental BHMT and concomitant ACL reconstruction. We show her radiological imaging pre-operatively and 6 years post-operatively. We present the following case in accordance with the CARE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-20/rc).
Case presentation
A 25-year-old female retired soccer player initially presented with right knee pain, swelling and instability. The patient mentioned that her right knee had multiple episodes of giving way and locking over three years but she had not sought treatment and continued playing soccer. Her symptoms worsened with increasing frequency of knee pain and instability over the previous few months.
On physical examination, she had full knee extension. The Lachman test and anterior drawer test were grade 2+ and there was an explosive pivot shift, indicating significant knee laxity (7,8). The examination of the knee collateral ligaments was normal. The pre-surgery Lysholm score was 45 and the subjective IKDC was 40.2.
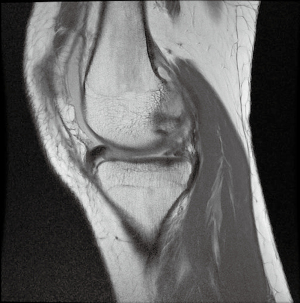
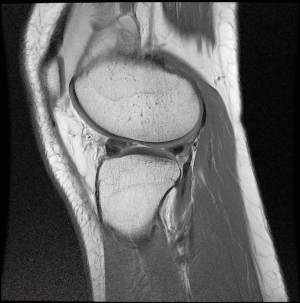
The pre-operative magnetic resonance imaging (MRI) of the right knee revealed bucket handle tears of both menisci. The extensive medial meniscus tear was displaced in the intercondylar notch. The lateral meniscus body and posterior horn tear yielded a displaced meniscus fragment that flipped over its anterior horn. There was an associated complete tear of the ACL (Figures 1,2).
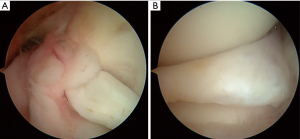
The patient underwent medial and lateral meniscus repair with concomitant ACL reconstruction. The complete ACL tear and displaced medial and lateral bucket handle tears was confirmed on arthroscopy (Figure 3). The medial and lateral meniscus tears had features of chronicity with rolled up meniscus edges. There was scar tissue present in the gutter between the displaced fragment and the peripheral capsular tissue that prevented reduction of the meniscus fragment. This scar tissue required release prior to reduction. The quality of both menisci tissue was good and amenable to repair sutures.
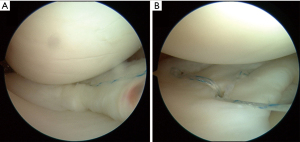
Both medial and lateral BHMT were reduced and repaired using an all-inside repair with FAST-FIX 360 (Smith & Nephew, London, UK) (Figure 4). Six all-inside devices were used to repair the medial meniscus and another six all-inside devices were used to repair the lateral meniscus. The ACL was a four-strand hamstring ACL reconstruction with transportal femoral tunnel drilling. The graft was fixed on a femoral cortical button and a tibia interference screw and backed up with a washer screw.
After surgery, the patient was placed on non-weight bearing for 3 weeks, then touch down weight bearing for 3–6 weeks. She was allowed full weight bearing after 6 weeks. The patient was placed in a knee brace that limited the knee range of motion from 0–90 degrees for 6 weeks postoperatively. She was allowed full range of knee motion after 6 weeks. Stationary bicycle and elliptical machine exercises were commenced after 8 weeks from surgery. Jogging was allowed only 6 months after the surgery when strength symmetry was recovered. She was followed up in our outpatient clinic with good recovery of range of motion and lower limb strength. The patient was able to return to playing soccer at a recreational level after 18 months.
At 2 years post-operatively, follow-up MRI showed an intact ACL graft as well as stable repair with no interval displaced re-tear of the medial and lateral menisci. The patient was asymptomatic and able to continue recreational soccer. The 2-year postoperative Lysholm score was 88 and the subjective IKDC score was 92.
At 6 years after surgery, on physical examination, the patient had full range of knee motion. Her knee anterior drawer test, Lachman test and pivot shift test were negative. The 6-year postoperative Lysholm score was 85 and subjective IKDC score was 88.
The MRI of the right knee at 6 years shows that the ACL graft was intact, and the repaired medial and lateral menisci were stable (Figures 5-7). The meniscus fissures and post-surgical scarring in the menisci were noted, with no re-displacement of the repaired fragment. The cartilage surfaces in both compartments of the knee were preserved. The 6-year repeat knee radiograph also showed minimal progression to knee osteoarthritis (Figure 8).




All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Simultaneous bicompartmental BHMTs were first described by Brammer et al. in 1999 as the “Jack and Jill lesion” (9). They remain a rare entity within the literature (1-3,6,9-15). The average age of the patients was 27.6 years old.
The MRI plays a crucial role in pre-operative evaluation and diagnosis of BHMTs. Radiological signs of BHMTs include: absent bow tie sign (3), double posterior cruciate ligament (PCL) sign (1,3,12), fragment-in-notch sign (1,3,13,16), coronal truncation sign (3,13), anterior flipped fragment sign (17), double delta sign (1,3,12,16), quadruple cruciate sign (3,12,16,18). MRIs are accurate in diagnosing BHMTs when two or more of the first five signs are present (17). In nine previous bicompartmental BHMT reports with pre-operative MRIs performed (1-3,10,12), all cases demonstrated at least one established radiological sign of BHMT. Bugnone et al. defined the “quadruple cruciate sign” to describe the appearance of the ACL and PCL and the displaced medial and lateral BHMT fragments seen in the intercondylar notch on coronal images (1). The pre-operative MRIs of our patient were positive for fragment-in-notch sign and anterior flipped fragment sign (Figures 1,2).
To our knowledge, this case report is the first to report on mid-term results after bicompartmental BHMT repairs with clinical outcomes and a 6-year post-operative MRI. The follow-up for previous bicompartmental BHMT case reports were up to 2 years post-surgery, with results based on clinical symptoms (3,10,13-15). In our patient, there was a 47% improvement in Lysholm score and a 54% improvement in subjective IKDC score 6 years post-surgery.
In terms of the duration from injury to surgical treatment, Zabrzyński et al. and Shepherd et al. both reported patients with BHMT treated 2–3 years after their injuries (2,6). Our patient presented with a three-year history of occasional knee instability and locking. She had sustained the ACL injury and probably sustained the medial BHMT first. The rolled-up appearance of the medial BHMT displaced fragment suggests significant chronicity and made the reduction of the meniscus fragment challenging. A new injury a few months prior could have caused the lateral BHMT. Chronic BHMT results in difficulties in meniscus reduction due to tissue scarring and these have to be addressed prior to reduction. Anatomical reduction of the meniscus fragment has to be followed by good and stable fixation with meniscus sutures, using inside-out, outside-in techniques or all-inside meniscus repair devices.
The meniscus repair in our case report was performed using FAST-FIX 360 (Smith & Nephew, London, UK), an all-inside meniscal repair device. Compared to current gold-standard inside-out meniscus repair, all-inside meniscus repair has the advantages of reduced surgical time, requires less assistance during surgery and lower risk to neurovascular structures (18). Various studies have concluded that all-inside meniscus repair is effective for meniscal repairs, with high success and low complication rates (16,18).
An important predictive criterion for successful repair of BHMT is the rim width. A rim width of 3 mm or less in the red-red zone has the highest healing rate after repair due to the greater vascularity (19). Other factors that can influence success include the location, length and chronicity of tear, fragment reducibility and age of the patient (18). Our patient was young, and tears in both menisci were in the peripheral vascular zones. Despite the chronicity of the injury, with adequate reduction and good fixation, a successful result was achieved.
The functions of the menisci are for load transmission, providing joint stability (both in anterior-posterior and rotational stability) and joint lubrication. These functions will be compromised after partial meniscectomy and can contribute to accelerated knee degeneration (20). The bicompartmental meniscus repair in our patient has helped to preserve the cartilage status in her knee at six years after surgery as seen on MRI and no knee osteoarthritis changes seen on radiograph. Another important learning point is that the finding of high-grade knee laxity on examination should raise the suspicion of BHMT in conjunction with an ACL injury. This has been shown where high grade knee laxity on physical examination is associated with large significant meniscus tears (7,8).
In conclusion, we report a case of a young retired soccer player who had undergone ACL reconstruction and all-inside repair of bicompartmental bucket handle meniscal tears. We present her functional outcomes and radiological imaging pre-operatively, at 2 years and 6 years post-operatively, which show intact and stable ACL graft and repaired menisci. This case report shows that with good reduction and fixation, all-inside meniscus repair can achieve good mid-term results for the repair of bicompartmental chronic bucket handle tears.
Acknowledgments
The authors would like to thank the patient for selflessly allowing us to share her case for the benefit of other patients and their surgeons.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-20/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-20/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-20/coif). YHDL reports receiving speaker fees from Smith & Nephew, Depuy Mitek, Arthrex and educational grants from Smith & Nephew, Depuy Mitek, Zimmer Biomet. YHDL is on ISKOAS Newsletter Committee and APKASS Council Board. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bugnone AN, Ramnath RR, Davis SB, et al. The quadruple cruciate sign of simultaneous bicompartmental medial and lateral bucket-handle meniscal tears. Skeletal Radiol 2005;34:740-4. [Crossref] [PubMed]
- Shepherd J, Abdul-Jabar HB, Kumar A. Locked bucket handle tears of the medial and lateral menisci with associated chronic ACL deficiency. J R Army Med Corps 2012;158:335-7. [Crossref] [PubMed]
- Yoon JR, Kim TS, Yang JH, et al. Simultaneous Bucket-handle Tears of both Medial and Lateral Meniscus - A Case Report -. Journal of the Korean Arthroscopy Society 2010;14:25-8.
- Keyhani S, Esmailiejah AA, Mirhoseini MS, et al. The Prevalence, Zone, and Type of the Meniscus Tear in Patients with Anterior Cruciate Ligament (ACL) Injury; Does Delayed ACL Reconstruction Affects the Meniscal Injury? Arch Bone Jt Surg 2020;8:432-8. [PubMed]
- Gadeyne S, Besse JL, Galand-Desme S, et al. Analysis of meniscal lesions accompanying anterior cruciate ligament tears: A retrospective analysis of 156 patients. Rev Chir Orthop Reparatrice Appar Mot 2006;92:448-54. [Crossref] [PubMed]
- Zabrzyński J, Szwedowski D, Zabrzyńska A, et al. Bicompartmental locked bucket-handle tears of menisci concealing the concomitant anterior cruciate ligament injury for 2 years - a case report. Journal of the Medical Sciences 2019;87:225-8. [Crossref]
- Song GY, Zhang H, Wang QQ, et al. Risk Factors Associated With Grade 3 Pivot Shift After Acute Anterior Cruciate Ligament Injuries. Am J Sports Med 2016;44:362-9. [Crossref] [PubMed]
- Magnussen RA, Reinke EK, Huston LJ, et al. Factors Associated With High-Grade Lachman, Pivot Shift, and Anterior Drawer at the Time of Anterior Cruciate Ligament Reconstruction. Arthroscopy 2016;32:1080-5. [Crossref] [PubMed]
- Brammer H, Sover E, Erickson S, et al. Simultaneous identification of medial and lateral bucket-handle tears: the Jack and Jill lesion. AJR Am J Roentgenol 1999;173:860-1. [Crossref] [PubMed]
- Bosch U. Combined injury of the medial and lateral meniscus and the anterior cruciate ligament. Oper Orthop Traumatol 2006;18:485-9. [Crossref] [PubMed]
- Cetik O, Cirpar M, Eksioglu F, et al. Simultaneous bucket handle tear of both medial and lateral menisci of a knee with chronic anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc 2006;14:356-9. [Crossref] [PubMed]
- Kakel R, Russell R, VanHeerden P. The triple PCL sign: bucket handle tears of both medial and lateral menisci in a chronically ACL-deficient knee. Orthopedics 2010;33:772. [Crossref] [PubMed]
- Koukoulias NE, Kyparlis D, Koumis P, et al. Locked bucket-handle tears of both medial and lateral menisci with simultaneous anterior cruciate and medial collateral ligaments injury. BMJ Case Rep 2011;2011:bcr0320114046. [Crossref] [PubMed]
- Tecklenburg K, Schoepf D, Hoser C, et al. Anterior cruciate ligament injury with simultaneous locked bucket-handle tears of both medial and lateral meniscus in a 19-year-old female professional ski racer: a case report. Knee Surg Sports Traumatol Arthrosc 2007;15:1125-9. [Crossref] [PubMed]
- Wright J, Tamura C, Findlay I, et al. Simultaneous bicompartmental bucket handle meniscal tears with a clinically competent Anterior Cruciate Ligament. J Orthop Surg Res 2010;5:68. [Crossref] [PubMed]
- Haas AL, Schepsis AA, Hornstein J, et al. Meniscal repair using the FasT-Fix all-inside meniscal repair device. Arthroscopy 2005;21:167-75. [Crossref] [PubMed]
- Dorsay TA, Helms CA. Bucket-handle meniscal tears of the knee: sensitivity and specificity of MRI signs. Skeletal Radiol 2003;32:266-72. [Crossref] [PubMed]
- Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res 2014;26:68-76. [Crossref] [PubMed]
- Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med 1982;10:90-5. [Crossref] [PubMed]
- Masouros SD, McDermott ID, Amis AA, et al. Biomechanics of the meniscus-meniscal ligament construct of the knee. Knee Surg Sports Traumatol Arthrosc 2008;16:1121-32. [Crossref] [PubMed]
Cite this article as: Bong GSY, Lee YHD. Concurrent medial and lateral bucket handle meniscal tear repair in a chronic anterior cruciate ligament-deficient knee: a case report. Ann Joint 2022;7:29.


