Lateral meniscus allograft transplantation without bone plugs: technique and outcomes
Introduction
Once considered a non-fundamental structure, the menisci are now known to provide several functions within the knee, including protection of articular cartilage, load-bearing, shock absorption, joint stability, joint lubrification and joint congruity functions (1,2).
Partial or total meniscectomy are commonly performed procedures. Despite providing an important role in pain relief, meniscectomies have been related to early onset of osteoarthritis due to an increase in tibiofemoral contact pressures. This phenomenon has been demonstrated to be true especially for active people (3,4). A meniscectomy will have several effects on the structure of the knee, it will be possible to observe narrowing of the joint space, flattening of femoral condyles and ridge formation. This change will lead to an alteration of the biomechanics of the knee joint and early degeneration of articular cartilage. This degeneration often manifests with pain and functional limitations, with an important impact in patient’s quality of life (5).
For all the reasons mentioned above it is recommended to preserve as much of the meniscus as possible.
Meniscal allograft transplantation has become a viable option for patients that have undergone total or near total meniscectomy and are in a painful state. Because of its minimal immune response, the meniscus is an optimal tissue to transplant. Several studies have demonstrated that peripheral vascularization of menisci is able to produce a significant repair response, producing matter similar to connective tissue (6,7). This allows the integration of an allograft implant to the capsular red zone.
The key to ensure a successful meniscal transplant includes patient selection and appropriate preoperative evaluation. The ideal candidate should be a young (<55 years) patient who has undergone a subtotal or total meniscectomy and develops knee pain and partial loss of function (8).
Previous infection in the knee, inflammatory arthritis, neuropathy, and evidence of osteonecrosis along with uncorrected malalignment or instability are considered contraindications to meniscal transplantation (9).
It is important to remember that each meniscal graft should be correctly sized based on the patient’s knee, in order to reduce the contact pressure (10). An incorrectly sized graft will lead to uneven contact forces. An oversized lateral meniscus allografts will lead to greater forces across the articular cartilage, whereas an undersized one will lead to greater forces across the meniscus (11).
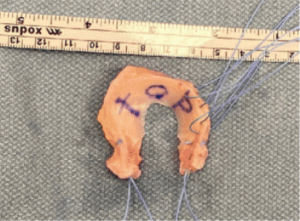
The transplantation can be performed using an open technique, an arthroscopically assisted procedures or a combination of these (12). The use of bone plugs is still controversial because of the fact that some studies support good clinical and biomechanical results (13), whereas other papers reported good clinical results with only suture fixation, without bone plugs (14,15). Even though it is not evident that fixation obtained using bone plugs versus sutures leads to improved outcomes, it must be taken into account that this technique requires a more exact size match between the graft and the host, henceforth increasing the risk of incorrect positioning that could lead to cartilage degeneration (16). Suture fixation without bone plugs (Figure 1), allows to reduce morbidity of the procedure and can be performed arthroscopically.
Surgical technique
The transplantation can be performed arthroscopically using a single tunnel. A standard diagnostic arthroscopic procedure is performed. The remnant of the native meniscus is removed to reach the meniscus-capsular zone. A bleeding bed is created at the periphery using a Steadman awl multiple times.
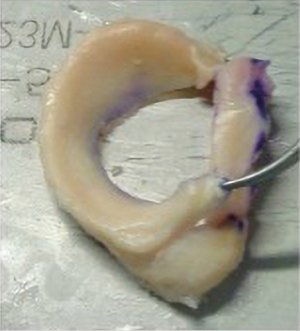
The appropriate size and direction of the graft should be confirmed before preparing the meniscal allograft through radiographic measurement and anthropometric parameters. The allograft will be presented as a meniscus with a portion of tibial plateau.
The first step is to remove all tissue ligaments from the periphery of the graft and bone plugs (Figure 2). Anterior and posterior horns are then fixed using a non-absorbable suture. The superior side of the meniscus is then marked to prevent mismatching during arthroscopic insertion.
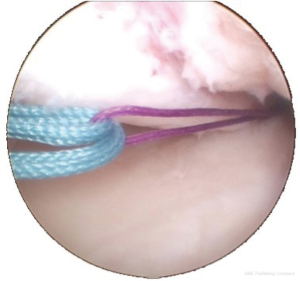
A 3-mm drill is used to create a tibial tunnel using the outside-in guide needed to secure the suture which matches the posterior meniscal horn to the anterior tibial cortex. The posterior tibial tunnel is created to pull the graft into the joint. For lateral meniscal transplantation the tunnel is performed behind the anterior cruciate ligament (ACL) tibial insertion. The tibial entrance of the tunnel is created on the medial side of the tibia. Then a non-absorbable shuttle suture is passed through the tibial tunnel, it is tied to the posterior horn suture and it is then passed through the posterior tunnel, working as a transport suture from inside to outside (Figure 3).
The graft is then introduced into the joint through the arthroscopic portal by pulling the suture fixed to the posterior meniscal horn (Figure 4). Ultimately the graft is fixed to the capsule with all-inside stitches, a mean of five stitches is used. Sometimes accessory portals could be required to place the stitches in the anterior third of the meniscus. Because of the fact that the load is shared between the sutures and the other all-inside stitches (8), there is only one suture required for each horn of the meniscus.
As a last step the transplanted meniscus is checked for stability and matching.
Outcomes
Results of meniscal allograft transplantation reported in the literature are difficult to interpret because of the small number of patients included in the studies, the heterogeneous population of patients studied, lack of outcome measures for evaluation of the allograft, and validity of methods used.
Meniscal extrusion is one of the most common problems that can effect both normal and osteoarthritic knee (17). Verdonk et al. (18) reported 70% partial extruded graft after a minimum follow up (FU) of 10 years, Lee et al. (19) fund 40% extruded grafts, but they also reported that the extruded allografts tend to stabilize in the long term.
Extrusion could be caused by several reasons, such as preoperative size mismatch, over-tensioning of the meniscal suture (20), loss of fixation of meniscal horns or insertion of the graft in an incorrect site. However is described in literature that there is no correlation between extrusion and clinical outcomes (18,21), but it can compromise long-term outcomes. Wang et al. (22) found that the possibility of meniscal extrusion increases in subchondral bone lesions and tibial plateau bone expansion in patients with knee osteoarthritis.
The most important aspect required to obtain good clinical results are graft size, anatomic placement and fixation (23). Alhalki et al. (24) demonstrated superiority of graft fixation with bone plug versus without plug in vitro, but the study doesn’t consider the biological healing capacity of the allograft to the meniscal rim and bone tunnels (8). Rodeo et al. (25) showed higher histological score in meniscal allografts transplanted without bone plug versus with bone plug. In addition, the presence of bone plug rises the immunological risk and incorrect graft-positioning risk, which could lead to cartilage damage (26). Despite using the bone plug or not, Wirth et al. (27) and van Arkel et al. (28) described good results both in pain relief and increased knee functionality. Long-term chondroprotective effect of meniscal allograft transplantation techniques are still not well known (29).
Complication
Complication rate associated with lateral meniscal transplantation ranges from to 10% to 50% in the literature. Graft tearing is the most common complication. Tears of meniscal allograft are treated the same way as tears of native meniscus, including meniscal repair or partial meniscectomy. Infection and immune reactions are uncommon complications following meniscal transplantation. No report of human immunodeficiency virus transmission has been described in the literature from the use of allografts. Other complications that may occur with meniscal transplantation includes loss of graft fixation, hemarthrosis, synovitis, and arthrofibrosis.
Our experience (8,30,31)
In our experience, lateral meniscus transplantation demonstrated significantly reduced pain, improved knee function, and increased patient physical activity: 94% of the patients benefited from this procedure at a minimum 3-year FU, representing an effective treatment for those patients treated with partial or total meniscectomy.
The results obtained confirm the success of meniscal transplantation procedure as a minimally invasive arthroscopic technique and graft fixation without bone blocks, although long-term reports are scarce. Among our studies, a significant improvement was reported in 10-year FU after transplantation with better post-operative clinical scores compared to the pre-operative scores, and highly satisfaction of the patients with good percentage of them (around 75%) involved in sports activity after surgery.
It is possible combining lateral meniscus transplantation with other surgical procedure without affecting long-terms outcomes; in the senior author experience, a closing wedge lateral high tibial osteotomy in case of varus deformity and a medial closing wedge distal femoral osteotomy in case of valgus deformity can be performed in the same surgical stage within the allograft transplantation as correction of deformity and resolution of post-meniscectomy syndrome. It could be associated with other procedures as ACL or posterior cruciate ligament (PCL) reconstruction, microfractures, osteochondral scaffolds, with good surgical and clinical results.
It still remains a surgical procedure with inferior surgical results and worse clinical outcomes compared to the medial meniscus transplantation in which the posterior tunnel was placed behind the medial tibial spine and in front of the PCL tibial insertion site (8), with a higher percentage of failure.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Alberto Grassi and Stefano Zaffagnini) for the series “The Lateral Meniscus” published in Annals of Joint. The article has undergone external peer review.
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-108/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-20-108/coif). The series “The Lateral Meniscus” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Allen D, Beaulé PE, Ramadan O, et al. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br 2009;91:589-94. [Crossref] [PubMed]
- Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br 1948;30B:664-70. [Crossref] [PubMed]
- King D. The function of semilunar cartilages. J Bone Joint Surg 1936;18:1069-76.
- Ahmed AM, Burke DL. In-vitro measurement of static pressure distribution in synovial joints--Part I: Tibial surface of the knee. J Biomech Eng 1983;105:216-25. [Crossref] [PubMed]
- Fabricant PD, Jokl P. Surgical outcomes after arthroscopic partial meniscectomy. J Am Acad Orthop Surg 2007;15:647-53. [Crossref] [PubMed]
- DeHaven KE. Peripheral meniscus repair: an alternative to meniscectomy. J Bone Joint Surg 1981;63:463.
- Arnoczky SP, Warren RF. The microvasculature of the meniscus and its response to injury. An experimental study in the dog. Am J Sports Med 1983;11:131-41. [Crossref] [PubMed]
- Marcacci M, Zaffagnini S, Marcheggiani Muccioli GM, et al. Meniscal allograft transplantation without bone plugs: a 3-year minimum follow-up study. Am J Sports Med 2012;40:395-403. [Crossref] [PubMed]
- Myers P, Tudor F. Meniscal allograft transplantation: how should we be doing it? A systematic review. Arthroscopy 2015;31:911-25. [Crossref] [PubMed]
- Lazović D, Wirth CJ, Knösel T, et al. Meniscus replacement using incongruent transplants--an experimental study. Z Orthop Ihre Grenzgeb 1997;135:131-7. [PubMed]
- Dienst M, Greis PE, Ellis BJ, et al. Effect of lateral meniscal allograft sizing on contact mechanics of the lateral tibial plateau: an experimental study in human cadaveric knee joints. Am J Sports Med 2007;35:34-42. [Crossref] [PubMed]
- Lubowitz JH, Verdonk PC, Reid JB 3rd, et al. Meniscus allograft transplantation: a current concepts review. Knee Surg Sports Traumatol Arthrosc 2007;15:476-92. [Crossref] [PubMed]
- Paletta GA Jr, Manning T, Snell E, et al. The effect of allograft meniscal replacement on intraarticular contact area and pressures in the human knee. A biomechanical study. Am J Sports Med 1997;25:692-8. [Crossref] [PubMed]
- Boss A, Klimkiewicz J, Fu FH. Technical innovation: creation of a peripheral vascularized trough to enhance healing in cryopreserved meniscal allograft reconstruction. Knee Surg Sports Traumatol Arthrosc 2000;8:159-62. [Crossref] [PubMed]
- González-Lucena G, Gelber PE, Pelfort X, et al. Meniscal allograft transplantation without bone blocks: a 5- to 8-year follow-up of 33 patients. Arthroscopy 2010;26:1633-40. [Crossref] [PubMed]
- Sekaran SV, Hull ML, Howell SM. Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med 2002;30:74-82. [Crossref] [PubMed]
- Zhang F, Bierma-Zeinstra SM, Oei EHG, et al. Factors associated with meniscal body extrusion on knee MRI in overweight and obese women. Osteoarthritis Cartilage 2017;25:694-9. [Crossref] [PubMed]
- Verdonk PC, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc 2006;14:694-706. [Crossref] [PubMed]
- Lee DH, Kim TH, Lee SH, et al. Evaluation of meniscus allograft transplantation with serial magnetic resonance imaging during the first postoperative year: focus on graft extrusion. Arthroscopy 2008;24:1115-21. [Crossref] [PubMed]
- Lee DH, Kim SB, Kim TH, et al. Midterm outcomes after meniscal allograft transplantation: comparison of cases with extrusion versus without extrusion. Am J Sports Med 2010;38:247-54. [Crossref] [PubMed]
- Ha JK, Shim JC, Kim DW, et al. Relationship between meniscal extrusion and various clinical findings after meniscus allograft transplantation. Am J Sports Med 2010;38:2448-55. [Crossref] [PubMed]
- Wang Y, Wluka AE, Pelletier JP, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford) 2010;49:997-1004. [Crossref] [PubMed]
- Alentorn-Geli E, Seijas Vázquez R, García Balletbó M, et al. Arthroscopic meniscal allograft transplantation without bone plugs. Knee Surg Sports Traumatol Arthrosc 2011;19:174-82. [Crossref] [PubMed]
- Alhalki MM, Howell SM, Hull ML. How three methods for fixing a medial meniscal autograft affect tibial contact mechanics. Am J Sports Med 1999;27:320-8. [Crossref] [PubMed]
- Rodeo SA, Seneviratne A, Suzuki K, et al. Histological analysis of human meniscal allografts. A preliminary report. J Bone Joint Surg Am 2000;82:1071-82. [Crossref] [PubMed]
- Sekiya JK, West RV, Groff YJ, et al. Clinical outcomes following isolated lateral meniscal allograft transplantation. Arthroscopy 2006;22:771-80. [Crossref] [PubMed]
- Wirth CJ, Peters G, Milachowski KA, et al. Long-term results of meniscal allograft transplantation. Am J Sports Med 2002;30:174-81. [Crossref] [PubMed]
- van Arkel ER, de Boer HH. Survival analysis of human meniscal transplantations. J Bone Joint Surg Br 2002;84:227-31. [Crossref] [PubMed]
- Matava MJ. Meniscal allograft transplantation: a systematic review. Clin Orthop Relat Res 2007;142-57. [Crossref] [PubMed]
- Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Survivorship and clinical outcomes of 147 consecutive isolated or combined arthroscopic bone plug free meniscal allograft transplantation. Knee Surg Sports Traumatol Arthrosc 2016;24:1432-9. [Crossref] [PubMed]
- Grassi A, Macchiarola L, Lucidi GA, et al. Long-term outcomes and survivorship of fresh-frozen meniscal allograft transplant with soft tissue fixation: minimum 10-year follow-up study. Am J Sports Med 2020;48:2360-9. [Crossref] [PubMed]
Cite this article as: Bonanzinga T, Doro GL, Dorotei A, Marcacci M. Lateral meniscus allograft transplantation without bone plugs: technique and outcomes. Ann Joint 2022;7:30.