
Intra-articular osteoid osteoma at the elbow mimicking arthritis: a case report
Introduction
Osteoid osteoma is a benign osteoblastic tumor characterized by a well-demarcated core and a distinctive surrounding zone of reactive bone formation. The tumor develops in the first to third decades of life and occur most commonly in the diaphysis or metaphysis of the femur and tibia; occurrence in the humerus is relatively rare (1). Nocturnal pain and characteristic symptoms that are relieved by administration of non-steroidal anti-inflammatory drugs (NSAIDs) are present and can help in the diagnosis of osteoid osteoma.
Intra-articular osteoid osteoma is rare and has a variety of clinical presentations. Approximately 5% of osteoid osteoma develops at intra-articular sites with severe mono-articular pain (2). In addition, intra-articular osteoid osteoma is sometimes misdiagnosed as synovitis, rheumatological diseases, or osteomyelitis because the imaging appearance of intra-articular tumor can be less classic than that of diaphyseal or metaphyseal tumor. Although the nidus can be detected with computed tomography (CT) or magnetic resonance imaging (MRI), clinical diagnosis is often delayed (3).
The lower extremities are a relatively common site for the development of intra-articular osteoid osteoma (2). In contrast, development in the elbow joint is extremely rare, and only a few reports have been published (4-8). Due to the rarity itself, osteoid osteoma in the elbow exhibits a variety of clinical manifestations.
Recently, we encountered an unusual case of an osteoid osteoma in the olecranon fossa. The patient exhibited motion pain rather than nocturnal pain, and notably, NSAIDs were not effective at all for relieving his symptoms. He also showed limited range of motion (ROM) and was initially treated for inflammatory arthritis such as rheumatoid arthritis by his previous doctor. The combination of imaging findings successfully led to a diagnosis of osteoid osteoma, and surgical resection was performed. To our knowledge, this is the first report of intra-articular osteoid osteoma in the olecranon fossa that mimicked arthritis. We present the following case in accordance with the CARE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-27/rc).
Case presentation
Five months before surgical therapy at our hospital, an 18-year-old male presented to our affiliate hospital with swelling and pain in the left elbow joint. He noticed difficulty with motion in his elbow joint 1 year before, and the symptom gradually worsened. Physical examination revealed elbow swelling with local heat and limited ROM. Plain radiographs were inconclusive, and MRI showed bone marrow edema around the elbow joint. Although inflammatory arthritis was thought to be the differential diagnosis, his symptoms were not relieved by conservative treatment such as rest, ice packs and NSAIDs administration, and he was referred to our hospital.
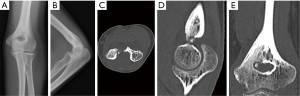
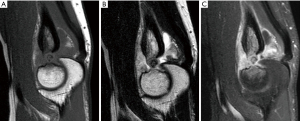
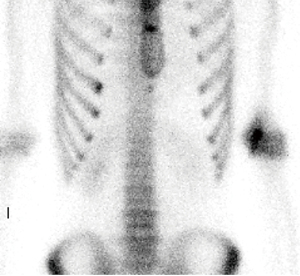
Three months after first presentation to our affiliate hospital, at the time of the first visit to our hospital, the symptoms were motion pain rather than pain at rest, and swelling and local heat were present in the entire left elbow joint. A physical examination revealed limited ROM (extension: −10 degrees and flexion: 120 degrees, Figure 1). Laboratory data showed negative C-reactive protein and rheumatoid factor. Although plain radiographs were still inconclusive, CT detected a so-called nidus lesion showing osteolytic changes (φ1 cm) with bony tissue-like structures in the center at the olecranon fossa of the distal humerus (Figure 2). MRI with gadolinium contrast agent showed hyperintense signals surrounding the nidus lesion (Figure 3). Technetium-99m bone scintigraphy showed strong accumulation and a double density sign (9) at the olecranon fossa, which corresponded to the nidus lesion (Figure 4). Considering the combination of these imaging findings, osteoid osteoma was thought to be the diagnosis. The patient received conservative treatment including rest and administration of NSAIDs, but the symptoms were not relieved at all.

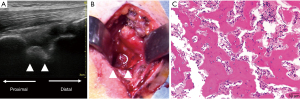
Two months later, he underwent an operation. Under general anesthesia, the patient was placed in a right lateral decubitus position. With echography guidance to minimize the burden to the joint, a skin incision was made (Figure 5A). Through a posterior approach to the elbow joint, the triceps was split, and the tumor at the olecranon fossa was exposed. The tumor was a circular red nodule with an elevated margin (Figure 5B). Because preoperative imaging showed that the tumor communicated to the anterior cortex of the humerus, we carefully resect entire tumor with a bone curette and confirmed the complete excision visually and postoperative plain radiograph (Figure S1). Histopathological examination showed that the lesion consisted of woven bones and osteoid tissues that anastomosed with each other (Figure 5C). Combined with a tumor size that was less than 2 cm, clinicopathologically, the tumor was diagnosed as an osteoid osteoma. Postoperatively, we immobilized the elbow at 90° of elbow flexion for a week. Then, gradual passive and active motion exercise was started. The pain was immediately relieved after the operation. No swelling was present, and ROM recovered at 2 months postoperatively. At 1 year after the surgery, the patient did not exhibit recurrence of the tumor or exacerbation of elbow pain and had a full range of elbow motion (extension: 0 degrees and flexion: 140 degrees, Figure 6). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.

Discussion
We reported a case of an osteoid osteoma in the olecranon fossa. The initial manifestation was arthritis-like symptoms such as local heat, motion pain, and limited ROM. The symptoms were resistant to conservative treatments, and thus, surgical resection was required. Because the symptoms were quite atypical, open resection was performed to confirm the pathological diagnosis. To minimize the burden to the elbow joint and to detect the tumor location, we employed echography guidance to precisely locate the tumor because the swelling was present in the entire left elbow joint.
The classic presentation of osteoid osteoma is pain at rest that is exacerbated at night and reduced by NSAIDs. Localized tenderness and swelling may be present in patients with bone involvement that is close to the skin (10). These signs and symptoms are usually secondary and can be confirmed by CT, MRI, and bone scintigraphy (9,11-14). In contrast, intra-articular osteoid osteoma sometimes has an unusual clinical presentation with atypical imaging findings. The clinical symptoms include joint tenderness, stiffness, swelling, and effusion, which are sometimes misdiagnosed as an infection or arthritis. Reactive cortical thickening and sclerosis may be absent or minimal due to the lack of the cambium in the inner layer of the periosteum (15).
Three cases of osteoid osteoma in the olecranon fossa have been reported in the literature (4,7,8). All three cases presented with limited ROM and local manifestations such as local pain or heat. In one case (8), NSAIDs were effective to relieve the pain; the effect of NSAIDs was not described for the other cases (4,7). All three cases showed pain at rest. One case showed mainly daytime pain (7), one case showed night pain (8), and the details of pain were not reported for the last case (4). Motion pain was not described in any of the three cases. In all three cases, symptoms including ROM improved after resection surgery, and no local recurrence was present. None of these cases had motion pain rather than pain at rest and resistance to NSAID treatment, which is usually effective for osteoid osteoma. In addition to reporting an atypical clinical presentation of osteoid osteoma in the elbow, our report is significant because it adds another item (osteoid osteoma) to the differential diagnosis of arthritis of the elbow if the patients are in the second and third decade of their life.
In conclusion, we experienced a case of an intra-articular osteoid osteoma of the elbow joint with atypical clinical presentations. Intra-articular osteoid osteoma in olecranon fossa may exhibit nonspecific clinical symptoms such as arthralgia and limited ROM, but clinical symptoms alone are poor indicators for suspicion of osteoid osteoma. Because lesions can be detected on CT and bone scintigraphy, osteoid osteoma should be considered for the differential diagnosis of arthritis of the elbow in patients who are adolescents and young adults, which is the peak age of onset for osteoid osteoma.
Acknowledgments
Special thanks to Ryota Kuzuhara for his advice and expertise.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-27/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-21-27/coif). NI serves as an unpaid editorial board member of Annals of Joint from December 2020 to November 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Healey JH, Ghelman B. Osteoid osteoma and osteoblastoma. Current concepts and recent advances. Clin Orthop Relat Res 1986;76-85. [Crossref] [PubMed]
- Rolvien T, Zustin J, Mussawy H, et al. Intra-articular osteoid osteoma as a differential diagnosis of diffuse mono-articular joint pain. BMC Musculoskelet Disord 2016;17:455. [Crossref] [PubMed]
- Mavrogenis AF, Dimitriou R, Benetos IS, et al. Juxta-articular osteoid osteoma of the talar neck: a case report. Clin Podiatr Med Surg 2010;27:629-34. [Crossref] [PubMed]
- Challawar NS, Shah HH. Intra-articular osteoid osteoma of the distal humerus: a diagnostic challenge. BMJ Case Rep 2014;2014:bcr2013202943. [Crossref] [PubMed]
- Bhatia DN. Arthroscopic Excision of Osteoid Osteoma of the Elbow. Arthrosc Tech 2017;6:e543-8. [Crossref] [PubMed]
- Goyal T, Pandita N, Paul S. Arthroscopic excision of intra-articular sub-periosteal osteoid osteoma of elbow: a case report. SICOT J 2018;4:25. [Crossref] [PubMed]
- Hatta T, Hosaka M, Watanuki M, et al. Arthroscopic Excision of Intra-Articular Osteoid Osteoma at the Elbow. Case Rep Orthop 2019;2019:8505382. [Crossref] [PubMed]
- Heybeli N, Babacan M. Intraarticular osteoid osteoma of the distal humerus. J Shoulder Elbow Surg 1997;6:311-3. [Crossref] [PubMed]
- Helms CA, Hattner RS, Vogler JB 3rd. Osteoid osteoma: radionuclide diagnosis. Radiology 1984;151:779-84. [Crossref] [PubMed]
- Swee RG, McLeod RA, Beabout JW. Osteoid osteoma. Detection, diagnosis, and localization. Radiology 1979;130:117-23. [Crossref] [PubMed]
- LINDBOM A. Angiography in osteoid osteoma. Acta radiol 1960;54:327-33. [Crossref] [PubMed]
- Gil S, Marco SF, Arenas J, et al. Doppler duplex color localization of osteoid osteomas. Skeletal Radiol 1999;28:107-10. [Crossref] [PubMed]
- Ebrahim FS, Jacobson JA, Lin J, et al. Intraarticular osteoid osteoma: sonographic findings in three patients with radiographic, CT, and MR imaging correlation. AJR Am J Roentgenol 2001;177:1391-5. [Crossref] [PubMed]
- von Kalle T, Langendörfer M, Fernandez FF, et al. Combined dynamic contrast-enhancement and serial 3D-subtraction analysis in magnetic resonance imaging of osteoid osteomas. Eur Radiol 2009;19:2508-17. [Crossref] [PubMed]
- Chai JW, Hong SH, Choi JY, et al. Radiologic diagnosis of osteoid osteoma: from simple to challenging findings. Radiographics 2010;30:737-49. [Crossref] [PubMed]
Cite this article as: Fukuda R, Matsuoka M, Kawamura D, Endo T, Kanno-Okada H, Urita A, Matsui Y, Onodera T, Iwasaki N. Intra-articular osteoid osteoma at the elbow mimicking arthritis: a case report. Ann Joint 2022;7:20.


