
This article has an erratum available at: http://dx.doi.org/10.21037/aoj-2023-01 the article has been update on 2023-10-10 at here.
Fixed distal femoral resection with a valgus cutting angle of 3° is more appropriate in intra-articular valgus deformity than juxta-articular valgus deformity in total knee arthroplasty: a retrospective single center study
Introduction
Restoration of the neutral mechanical axis of the lower extremity is a critical goal in mechanically aligned total knee arthroplasty (TKA) (1) and is important for the longevity of prostheses as well as favorable functional outcomes (2). This can be achieved by making coronal bone cuts perpendicular to the mechanical axes of the femur and tibia (3). The primary origin of valgus deformity is mostly present on the femur (4,5); therefore, while correcting the valgus deformity, it is important to perform a precise distal femoral resection with an accurate valgus cutting angle (VCA).
Several studies have suggested methods for accurate femoral cutting in valgus knees with arthritis, including the use of the anatomical-mechanical axis angle (AMA-A) with medialized entry for the intramedullary rod, intraoperative navigation, or patient-specific guide (4). These methods had limitations that make clinical application difficult. Bone defect on the medial condyle was a limitation for the use of the AMA-A with medialized entry for the rod (4). High costs and long learning curve limited the use of the navigation (6). There was no evidence demonstrating improvement in coronal alignment when using the patient-specific guide (7). Therefore, the traditionally recommended fixed VCA of 3° is still used as the standard method in valgus deformity, with its use supported by the successful outcomes of a long-term clinical study (8,9). However, in certain cases, occurrence of unsatisfactory femoral component alignment when using a fixed VCA of 3° can be a matter of concern because this method is not customized according to the different femoral anatomies.
Knees with valgus deformity can be classified into intra-articular (IA) and juxta-articular (JA) types according to the level of the origin of the femoral deformity (10). They are characterized by hypoplasia of the lateral femoral condyle or metaphyseal valgus deformity, respectively (2,10). The accuracy of distal femur cutting can be affected by the type of valgus deformity because the intramedullary rod for distal femoral resection can become impinged on the femoral cortex (4). No studies have compared the accuracy and precision of a fixed VCA of 3° between the different types of valgus deformity.
The purpose of the present study is to analyze the accuracy and precision of a fixed VCA of 3° in mechanical alignment in TKAs for valgus deformity, based on the type of the deformity. We hypothesized that this traditional standard concept for the VCA is more appropriate in JA deformity than in IA deformity because of the impingement of the intramedullary rod on the femoral cortex. Our study will help clinicians determine the appropriate VCA for satisfactory alignment of the femoral component in valgus deformities. The study was presented following the STROBE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-8/rc).
Methods
Patients
Between March 2001 and February 2016, 339 TKAs were performed in knees with valgus deformity by two senior surgeons at our institution. Patients undergoing (I) primary TKA for osteoarthritis or inflammatory arthritis (including rheumatoid or hemophilic arthritis) with Kellgren-Lawrence grade 4 and hip-knee-ankle (HKA) angle > valgus 5° and (II) those with available appropriate full-length standing anteroposterior (AP) radiographs were included. Exclusion criteria were (I) a history of knee infection, fracture, dislocation, or ligament injury (54 cases), (II) knee instability (28 cases), (III) a history of reconstructive ligament surgery or high-tibial osteotomy (8 cases), and (IV) obvious deformity of the proximal or mid-shaft of the femur (36 cases).
According to the criteria, 212 TKA cases were included and retrospectively analyzed in the present study. The overall mean age of the patients was 65.9 years [standard deviation (SD): 11.2 years)], and there were 148 female and 64 male patients, respectively. The mean body mass index was 26.0 kg/m2 (SD: 2.9). There were 168 knees with degenerative osteoarthritis, 26 knees with rheumatoid arthritis, and 18 knees with hemophilic arthritis. The mean degree of valgus deformity was 12.3° (SD: 5.4°; range: valgus 5.3 to valgus 29.6).
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of Kyung Hee University Hospital (No. KHUH 2020-09-040). Informed consent was obtained from all patients prior to review.
Surgical techniques
Press Fit Condylar (PFC) Sigma® or Attune® prostheses (Depuy Synthes, Warsaw, IN, USA) were implanted using posterior stabilized (PS) or constrained condylar knee (CCK) inserts. A tourniquet was applied during the procedures. All procedures were performed using a modified measured resection technique to restore the mechanical alignment. In all the cases, the medial parapatellar approach was used with a midline skin, which is used by majority of the orthopedic surgeons; the anterolateral approach was not used, considering the difficulty of closing the lateral compartment after the correction of the deformity (11). An intramedullary guide was used for femoral resection. The conventional central entry was used for the intramedullary rod, which was placed at the center of the femoral trochlea and 7–10 mm anterior to the top of the intercondylar notch. A fixed VCA of 3° was used. The thickness of distal femoral resection was typically 9 mm, as maintained by the standard technique of the implant systems; additional resection was performed in case of flexion contracture ≥15 degrees, and less resection was performed in case of hyperextension. The transepicondylar axis was used for femoral component rotation. The size of the femoral component was selected using the anterior-referencing method. An extramedullary guide was used for tibial resection. The posterior tibial slope was set to be 2°–3° of the posterior slope in the sagittal plane. The reference line for tibial rotation was accurately aimed at a line passing through the medial third of the tibial tubercle and the second metatarsal or the middle of the talus. All osteophytes were removed. Any contracted soft tissue was carefully examined and selectively released when required. The iliotibial band or the posterolateral capsule was mainly released; while the medial soft tissues were minimally released (2). All patellae were resurfaced. Patellofemoral articulation was carefully evaluated using the “no thumb” technique. All components were implanted on cleaned and dried cut surfaces using a full cementation technique. The level of constraint of the polyethylene insert was decided intraoperatively by the surgeons. The PS insert was used in 196 (92.5%) TKA cases with well-balanced flexion-extension and medio-lateral gaps, while the CCK insert was used in 16 (7.5%) TKA cases with insufficient medio-lateral stability.
Isometric exercises using the extensor and flexor muscles were initiated shortly after surgery. The drain was removed on the second postoperative day, and active and assisted range of motion (ROM) exercises were initiated. Full weight-bearing ambulation was started after 3 days according to the patient’s condition.
Clinical evaluation
Clinically, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores and ROM were evaluated preoperatively and at 5 years after TKA (last follow-up) (12). The ROM was measured using a long-armed goniometer.
Radiographic evaluation
Radiographic parameters were measured preoperatively, at 3 months after TKA (postoperative), and at the last follow-up. Full-length AP radiographs were obtained under weight-bearing conditions. The quality of the radiographs was improved using the radiographic protocol of standardization for the position of the knee and using an identical distance between the X-ray beam and cassette (13). The radiographs were taken with the patient standing with the knee fully extended and the feet slightly internally rotated to ensure forward placement of the knees (14).
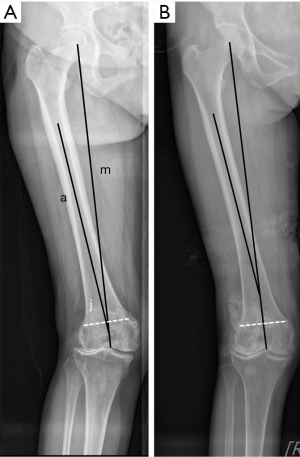
The type of valgus deformity was determined based on the mechanical and anatomical axes of the femur. The mechanical axis of the femur was defined as a line between the center of the femoral head and the center of the intercondylar notch of the native femur or implant. The anatomical axis of the femur was defined as the central line along the intramedullary canal of the middle of the femur (4). The anatomical axis usually crosses at the midpoint of the femoral notch in the femurs without any deformity (4). IA deformity was determined when the point of crossing between the femoral mechanical and anatomical axes was below the tangent line of the superior borders of the medial and lateral femoral condyles (Figure 1A). JA deformity was determined when the point was above the tangent line (Figure 1B) (10). The tangent line of the femoral condyles indicates the boundary of the knee joint because an anatomical projection of the posterior superior knee joint capsule is around this line and the area of the articular cartilage of the posterior condyle lies below it (10).
The HKA angle was defined as the angle between the femoral and tibial mechanical axes on orthoroentgenograms (15). The mechanical axis of the femur was defined as described above, and the mechanical axis of the tibia was defined as a line connecting the center of the tips of the spines of the native tibial plateau or tibial base plate with the center of the talus. Valgus alignment was denoted with a positive value and varus alignment was denoted with a negative value. The mechanical-lateral-distal-femoral angle (mLDFA) was defined as the lateral angle between the femoral mechanical axis and a tangent line of the most distal points of the femoral condyles in the native knee or implant (4). The mechanical-medial-proximal-tibial angle (mMPTA) was defined as the medial angle between the tibial mechanical axis and a tangent line of the native proximal tibial plateau or the tibial base plate (3).
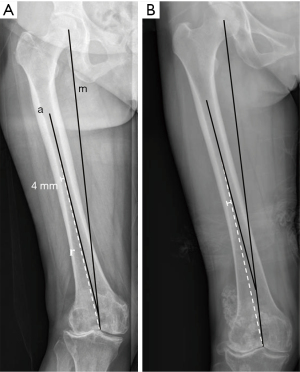
The AMA-A was measured preoperatively as the acute angle between the mechanical and anatomical axes of the femur (Figure 2) (4). The adjusted-VCA (aVCA) was measured considering impingement of the intramedullary rod on the inner femoral cortex and the radius of the rod. A reference intramedullary line was drawn from the center of the intercondylar notch (central entry point), and this line was at least 4 mm away from the femoral inner cortex (Figure 2). The reason for the distance of 4 mm is that the radius of the intramedullary rod of the PFC® and Attune® prostheses is 4 mm (16,17). This reference line implements an intraoperative situation in which the rod is forced away by the inner femoral cortex when it enters from the central entry in a valgus knee. The aVCA was measured as the acute angle between the reference line and the femoral mechanical axis, which indicates the maximum angle within the range without impingement of the intramedullary rod by the inner femoral cortex (Figure 2).
The images were transferred digitally to a picture archiving and communication system (PACS). Radiographic magnification of all measurements was corrected using the PACS ruler. Assessments were performed on a 61-cm (24-inch) monitor (SyncMaster 2494HMN; Samsung, Seoul, South Korea) in portrait mode using PACS software. The minimum differences that the software could detect were 0.1° and 0.1 mm (18). Two orthopedic surgeons measured all the radiographic parameters to reduce observation bias. The inter-observer agreement for determining valgus type was assessed, and all of the determination was consistent. The inter-observer reliability of other radiographic measurements was assessed using an intraclass correlation coefficient. The intraclass correlation coefficient for all measurements was >0.8, and the average values were used in the study.
Complications
Any complications and additional surgeries were investigated with reference to the standardized list and definitions of complications in TKA suggested by the Knee Society (19).
Statistical analysis
Preoperative clinical data were compared with last follow-up data using the paired t-test. Preoperative radiographic data were compared with postoperative radiographic data, and postoperative radiographic data were compared with last follow-up radiographic data to evaluate radiographic changes over time (paired t-test). The AMA-A and aVCA were compared using the paired t-test. The clinical and radiographic results were compared between the IA and JA groups using the independent t-test. The proportions of well-aligned femoral component (postoperative mLDFA <90°±3°) and well-aligned knee (postoperative HKA angle <0°±3°) were compared between the IA and JA groups using Chi-square or Fisher’s exact test (1,20). The correlation between AMA-A-3° or aVCA-3° (defined as the difference between a fixed VCA of 3° and the AMA-A or aVCA) and postoperative LDFA-90° (defined as the degree of varus or valgus of the femoral component in compared to the femoral mechanical axis) were analyzed using Pearson correlation analysis. Correlation analysis was performed to determine the parameter that is closely related to the coronal alignment of the femoral component. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA), and a P value of <0.05 was considered statistically significant.
A power analysis was performed to determine the minimum sample size affording sufficient power, with the aVCA, postoperative mLDFA, and proportion of well-aligned femoral component as the important outcomes. The power and alpha level were set to 0.8 and 0.05, respectively. As a result, the appropriate sample sizes for the aVCA, postoperative mLDFA, and proportion of well aligned femoral component were 18, 40, and 91 cases in each group, respectively. Therefore, it was determined that our sample size was adequately powered.
Results
General clinical and radiographic results
Clinically, the average WOMAC score was 66.4 (SD: 4.9) preoperatively and 10.9 (SD: 5.1) at the last follow-up (P<0.001). The ROM improved from 124.0° (SD: 19.1°) preoperatively to 134.3° (SD: 13.3) at the last follow-up (P<0.001).
Radiographically, the HKA angle was corrected from valgus 12.3° (SD: 5.4°) to varus 0.7° (SD: 2.5°) (P<0.001). The mLDFA was 83.9° (SD: 3.3°) preoperatively and 91.2° (SD: 2.1°) postoperatively (P<0.001). The mMPTA was 90.9° (SD: 3.0°) preoperatively and 90.4° (SD: 2.0°) postoperatively (P=0.019). There were no significant changes in the HKA angle [varus 0.7° (SD: 2.5°) vs. varus 0.9° (SD: 2.8°), P=0.109), mLDFA (91.2° vs. 91.3° (SD: 2.4°), P=0.231), and mMPTA [90.4° (SD: 2.0°) vs. 90.4° (SD: 2.0°), P=0.772] at the last follow-up compared to the postoperative values.
The AMA-A was 6.5° (SD: 1.1°) and the aVCA was 4.8° (SD: 1.2°) preoperatively (P<0.001).
Clinical and radiographic results between knees with IA and JA deformities
There were 110 knees with IA deformity and 102 knees with JA deformity. There were no significant differences in age, sex, body mass index, and preoperative diagnosis between the groups (Table 1). The proportion of IA or JA deformity was not significantly different between the patients with osteoarthritis (IA =51.2%; JA =48.8%) and rheumatoid arthritis (IA =46.2%; JA =53.8%) (P=0.678) (Table 1).
Table 1
| Demographics | Intra-articular deformity | Juxta-articular deformity | P value |
|---|---|---|---|
| Number of knees | 110 | 102 | |
| Age (years)† | 65.8±10.9 | 66.1±11.6 | 0.810 |
| Females/males | 78/32 | 70/32 | 0.766 |
| Body mass index (kg/m2) † | 26.0±2.8 | 26.0±3.0 | 0.878 |
| Preoperative diagnosis (OA, RA, HA) | 86/12/12 | 82/14/6 | 0.389 |
†, continuous variables are presented as mean ± standard deviation. OA, osteoarthritis; RA, rheumatoid arthritis; HA, hemophilic arthritis
Clinically, the WOMAC score and ROM were not significantly different between the IA and JA groups preoperatively and at the last follow-up (Table 2). Radiographically, there were no significant differences in the HKA angle, mLDFA, and mMPTA preoperatively between the groups (Table 3). The aVCA was significantly lesser than the AMA-A in both groups (P<0.001 for each). Although the AMA-A was significantly larger in the JA group than in the IA group (6.8° vs. 6.2°, P<0.001), the aVCA was significantly lesser in the JA group than in the IA group (4.1° vs. 5.4°, P<0.001) (Table 3). The difference between the AMA-A and aVCA was greater in the JA group than in the IA group (2.7° vs. 0.8°, P<0.001) (Table 3).
Table 2
| Clinical results | Evaluation time | Intra-articular deformity | Juxta-articular deformity | P value |
|---|---|---|---|---|
| WOMAC score | Preoperative | 66.4±4.7 (55–75) | 66.3±5.1 (58–74) | 0.888 |
| Last follow-up | 11.0±5.0 (0–24) | 10.7±5.2 (0–23) | 0.670 | |
| Range of motion (°) | Preoperative | 125.1±18.6 (100–150) | 122.9±19.7 (100–145) | 0.395 |
| Last follow-up | 135.3±12.3 (100–150) | 133.2±14.3 (100–150) | 0.247 |
Continuous variables are presented as mean ± standard deviation (range). WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Table 3
| Radiographic parameters | Intra-articular deformity | Juxta-articular deformity | P value |
|---|---|---|---|
| Hip-knee-ankle angle (°) | |||
| Preoperative | Valgus 12.1±5.5 (5.3–27.3) | Valgus 12.5±5.2 (6.1–29.6) | 0.647 |
| Postoperative | Varus 1.0±2.5 (6.4–5.1) | Varus 0.3±2.5 (5.4–5.8) | 0.027 |
| mLDFA (°) | |||
| Preoperative | 84.3±2.5 (77.9–89.3) | 83.5±3.9 (74.7–91.0) | 0.083 |
| Postoperative | 91.7±2.0 (85.7–96.3) | 90.6±1.9 (85.8–94.3) | <0.001 |
| Mechanical-medial-proximal-tibial angle (°) | |||
| Preoperative | 91.2±3.3 (84.8–100.6) | 90.6±2.4 (83.3–97.0) | 0.205 |
| Postoperative | 90.6±2.1 (85.2–96.2) | 90.1±1.9 (86.3–93.7) | 0.069 |
| AMA-A (°) | 6.2±1.3 (3.2–9.1) | 6.8±1.1 (4.9–9.3) | <0.001 |
| aVCA (°) | 5.4±1.0 (2.7–8.3) | 4.1±1.0 (1.9–6.9) | <0.001 |
| Difference between AMA-A and aVCA (°) | 0.8±0.8 (−0.9 to 4.5) | 2.7±1.3 (−0.3 to 6.4) | <0.001 |
Continuous variables are presented as mean ± standard deviation (range). mLDFA, mechanical-lateral-distal-femoral angle; AMA-A, Anatomical-mechanical-axis angle; aVCA, adjusted valgus cutting angle.
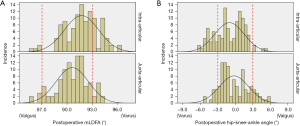
When using a fixed VCA of 3°, the postoperative HKA angle demonstrated more varus alignment in the IA group than in the JA group (varus 1.0° vs. varus 0.3°, P=0.027) (Table 3). The mLDFA was also demonstrated more varus alignment in the IA group than in the JA group (91.7° vs. 90.6°, P<0.001). The mMPTA was not different between the groups postoperatively (90.6 vs. 90.1, P=0.069) (Table 3). The postoperative proportion of the well-aligned femoral component was 70% in the IA group and 85.3% in the JA group (P=0.009) (Figure 3A). Postoperatively, the proportion of well aligned knees showed no significant difference (72.7% vs. 76.5%, P=0.636) (Figure 3B).
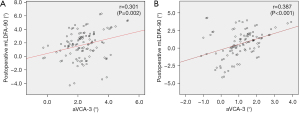
Correlation between the AMA-A or aVCA and the postoperative mLDFA
There was weak positive correlation between AMA-A-3° and postoperative mLDFA-90° (r=0.197, P=0.004) (Figure 4A) and moderate positive correlation between aVCA-3° and postoperative mLDFA-90° (r=0.406, P<0.001) (Figure 4B) (Table 4). This finding implies that the alignment of the femoral component became more varus when the difference between the AMA-A or aVCA and a fixed VCA of 3°increased.
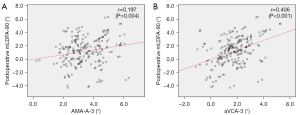
Table 4
| Parameters | Total | Intra-articular deformity | Juxta-articular deformity |
|---|---|---|---|
| AMA-A-3° and postoperative mLDFA-90° (°) | 0.197 (P=0.004) | 0.274 (P=0.004) | 0.294 (P=0.002) |
| aVCA-3° and postoperative mLDFA-90° (°) | 0.406 (P<0.001) | 0.301 (P=0.002) | 0.387 (P<0.001) |
Continuous variables are presented as mean ± standard deviation. AMA-A, anatomical-mechanical-axis angle; aVCA, adjusted valgus cutting angle; mLDFA, mechanical-lateral-distal-femoral angle.
This trend was also observed in correlation analysis conducted separately for each group (Table 4). Weak correlation was observed between AMA-A-3° and postoperative mLDFA-90° in both groups, and moderate correlation was observed between aVCA-3° and postoperative mLDFA-90° in both groups (Figure 5).
Complications
No complications, such as loosening of the components, instability, and patellofemoral dislocation, were recorded.
Discussion
The most important finding of the present study was that the accuracy and precision of a fixed VCA of 3° was better for mechanical alignment in valgus knees with JA deformity than those with IA deformity. The aVCA is a more reliable parameter that is moderately correlated to the alignment of the postoperative femoral component than the AMA-A, considering the impingement of the intramedullary rod on the femoral cortex in valgus deformity.
Valgus knee arthritis is a complex deformity characterized by a hypoplastic lateral femoral condyle, femoral and tibial metaphyseal valgus remodeling, and medial soft tissue laxity (4,10). Thienpoint et al. (5) have reported that a valgus arthritic knee has a substantial distal femoral valgus anatomy with an average mLDFA of 85°, tibial extra-articular deformity with an average mMPTA of 90°, and medial soft laxity of a joint line convergence angle of 2°. They suggested that the valgus deformity should be corrected mainly on the femoral side. Therefore, the VCA in distal femoral resection is critical in restoring the mechanical alignment of the lower extremity in TKA for valgus arthritis.
A fixed VCA of 3° has been the standard in TKAs for valgus knee arthritis (2,21). However, the exact rationale for this traditional concept has not been described. Although this concept has been described as being used to avoid under-correction of underlying deformity and residual valgus deformity (2,8), it has not been explained why the valgus deformity remains when performing TKA with the generally used VCA in reference to the AMA-A. Considering our results, the reliability of a fixed VCA of 3° in the valgus knee can be explained by the change in the direction of the intramedullary rod due to impingement of the femoral cortex and the radius of the rod. In such a situation, the VCA becomes smaller and if the AMA-A is used, the femur will be cut more valgus than expected, which will result in residual valgus.
Such a situation of a decreased VCA in valgus knee was more evident in JA deformity than in IA deformity. Although a change in the direction of the intramedullary rod due to the impingement can also occur in IA deformity (4), it is more significant in JA deformity due to metaphyseal bowing (Figure 2). Therefore, based on the aVCA, the concept of a fixed VCA of 3° appears more suitable for JA valgus deformity with metaphyseal valgus bowing (aVCA: 4.1°). In contrast, it is believed that care should be taken when applying the traditional concept in IA deformity (aVCA: 5.4°). With a fixed VCA of 3°, the femoral component and lower extremity were less mechanically aligned, and the proportion of well-aligned femoral component was significantly lower in the IA group than that in the JA group in our study. The type of deformity should be considered when determining the VCA in TKA for knees with valgus deformity.
Our correlation analysis showed that the aVCA was a more reliable parameter than the AMA-A in predicting postoperative femoral alignment. However, the aVCA demonstrated moderate correlation and not strong correlation. The reason for this is believed to be the fact that the degree of actual valgus cutting is less than the aVCA (indicating the maximum value within the range without cortex impingement) because the intramedullary rod is remarkably smaller than the femoral canal space, which allows more movement of the rod (20,22). Further, the degree of actual valgus cutting can be affected by various factors including the location and size of entry hole, large tolerance of the cutting slot, and bone quality (23).
There has been a concern about the tendency for valgus recurrence over time after TKA (21,24). However, there was no significant change in the alignment of the components and lower extremity up to 5 years postoperatively in this study. In addition to acceptable limb alignment and proper soft tissue balancing, one of the main reasons for no valgus reoccurrence is that the alignment of the femoral component and lower extremity were slightly varus with a fixed VCA of 3°. Another reason is that the follow-up period of 5 years may be too short to observe recurrence.
Considering the femoral impingement and radius of the intramedullary rod, the aVCA is considered a reliable concept to achieve mechanical alignment in valgus knee arthritis. The use of aVCA, being a customized method, can further improve the femoral component alignment of each individual with different anatomy compared to the batch application of a fixed VCA of 3°. A fixed VCA of 3° can be a simple method to achieve acceptable mechanical alignment in JA valgus deformity in which the average of the aVCA is close to 4°. However, it may not be a reliable method in IA deformity.
Although the navigation or patient-specific guide has been used for accurate distal femoral cutting in valgus deformity, there are limitations in terms of the cost-effectiveness and long learning curve (4). Huang et al. showed similar coronal and sagittal femoral component position in TKAs using navigation and conventional instruments in patients with advanced valgus knee arthritis (25). A previous study suggested the use of AMA-A with medialization of entry for the intramedullary rod to achieve proper mechanical alignment in TKA for valgus deformity (4). However, their method also had a limitation in how long the entry point medialized from the knee center intraoperatively; the distance for medialization was determined in a preoperative radiograph, and the radiographic distance might be different with intraoperative distance due to radiographic magnification (26). In addition, there was a bone defect at the medial femoral condyle, which could be a risk factor for postoperative or intraoperative fracture (27). Although the defect could be filled with resected bone, it would be technically demanding and make operative time delay. It is thought that the central entry point for the intramedullary rod with the aVCA will be a convenient, economical, and practical method.
The present study has several limitations. First, this was a retrospective study with low level of evidence. To obtain more robust data, prospective studies are required. Second, the sample size was relatively small despite adequate power. Further studies with larger study cohorts are required for more robust results. Third, all measurements were assessed using radiographs and not three-dimensional computed tomography, which allows for corrections for rotational errors. With a limb rotation of 40°, a VCA can vary by 1°–2.5° and the HKA angle can vary by up to 5° in radiographs (3). It could be argued that the use of a three-dimensional imaging study would be more accurate. However, concerns regarding radiation exposure and imaging costs make such studies difficult to perform. Additionally, special care was taken to control the patient positioning while performing imaging in this study. Fourth, two surgeons performed TKAs with two prostheses, which might be a confounding factor. However, their surgical philosophies and techniques were similar. Additionally, the Attune® (Depuy Synthes) prosthesis is a successor of the PFC® (Depuy Synthes); the concepts of implantation and instrumentation are similar and the diameters of the intramedullary rod are the same for both. Fifth, whether the intramedullary rod was actually impinged during the surgery of the juxta-medullary deformity was not confirmed. It would have been better if the impingement of the intramedullary rod was evaluated using intraoperative fluoroscopy. Lastly, the procedures were performed by two experienced surgeons in a tertiary medical center with only two prostheses. Additionally, the procedures were performed in Asian patients. Therefore, caution should be taken when extrapolating our results to other populations.
Conclusions
Although a fixed VCA of 3° is a reliable method in achieving mechanical alignment in valgus deformity, it can be more appropriate in juxta-articular deformity than in intra-articular deformity. The aVCA is a more reasonable predictor of femoral component alignment than the AMA-A, considering the femoral cortex impingement of the intramedullary rod.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-8/rc
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-8/dss
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-8/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-8/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board of Kyung Hee University Hospital (No. KHUH 2020-09-040). Informed consent was obtained from all patients prior to review.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Andrews SN, Beeler DM, Parke EA, et al. Fixed Distal Femoral Cut of 6 degrees Valgus in Total Knee Arthroplasty: A Radiographic Review of 788 Consecutive Cases. J Arthroplasty 2019;34:755-9. [Crossref] [PubMed]
- Alesi D, Meena A, Fratini S, et al. Total knee arthroplasty in valgus knee deformity: is it still a challenge in 2021? Musculoskelet Surg 2022;106:1-8. [Crossref] [PubMed]
- Davis JA, Hogan C, Dayton M. Postoperative Coronal Alignment After Total Knee Arthroplasty: Does Tailoring the Femoral Valgus Cut Angle Really Matter? J Arthroplasty 2015;30:1444-8. [Crossref] [PubMed]
- Tan H, Wang Y, Long T, et al. How to accurately determine the distal femoral valgus cut angle in the valgus knee arthroplasty. Int Orthop 2018;42:537-42. [Crossref] [PubMed]
- Thienpont E, Schwab PE, Cornu O, et al. Bone morphotypes of the varus and valgus knee. Arch Orthop Trauma Surg 2017;137:393-400. [Crossref] [PubMed]
- Bae DK, Song SJ. Computer assisted navigation in knee arthroplasty. Clin Orthop Surg 2011;3:259-67. [Crossref] [PubMed]
- Victor J, Dujardin J, Vandenneucker H, et al. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 2014;472:263-71. [Crossref] [PubMed]
- Elkus M, Ranawat CS, Rasquinha VJ, et al. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am 2004;86:2671-6. [Crossref] [PubMed]
- Ren J, Zhang X, Wulamu W, Y, et al. Total knee arthroplasty with the least-constrained implant possible for type II valgus knee > 20°: a 3-14 years' follow-up. Arthroplasty 2020;2:17. [Crossref] [PubMed]
- Yin X, Yang D, Zhou Y, et al. Different femoral origins of valgus deformity affect aspect ratios of resected distal femurs in total knee arthroplasty. Knee 2019;26:1073-9. [Crossref] [PubMed]
- Rossi R, Rosso F, Cottino U, et al. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273-83. [Crossref] [PubMed]
- Giesinger JM, Hamilton DF, Jost B, et al. WOMAC, EQ-5D and Knee Society Score Thresholds for Treatment Success After Total Knee Arthroplasty. J Arthroplasty 2015;30:2154-8. [Crossref] [PubMed]
- Bae DK, Song SJ, Kim HJ, et al. Change in limb length after high tibial osteotomy using computer-assisted surgery: a comparative study of closed- and open-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc 2013;21:120-6. [Crossref] [PubMed]
- Stickley CD, Wages JJ, Hetzler RK, et al. Standard Radiographs Are Not Sufficient for Assessing Knee Mechanical Axis in Patients With Advanced Osteoarthritis. J Arthroplasty 2017;32:1013-7. [Crossref] [PubMed]
- Lee HW, Song SJ, Bae DK, et al. The influence of computer-assisted surgery experience on the accuracy and precision of the postoperative mechanical axis during computer-assisted lateral closing-wedge high tibial osteotomy. Knee Surg Relat Res 2019;31:15. [Crossref] [PubMed]
- DePuy Synthes. ATTUNE® Knee System 2017 [cited 2017 22 May]. Available online: https://www.depuysynthes.com/hcp/knee/products/qs/ATTUNE-Knee-System
- DePuy Synthes. SIGMA® Total Knee System 2017 [cited 2017 20 June]. Available online: https://www.depuysynthes.com/hcp/knee/products/qs/SIGMA-Total-Knee-System
- Song SJ, Lee HW, Park CH. A Current Prosthesis With a 1-mm Thickness Increment for Polyethylene Insert Could Result in Fewer Adjustments of Posterior Tibial Slope in Cruciate-Retaining Total Knee Arthroplasty. J Arthroplasty 2020;35:3172-9. [Crossref] [PubMed]
- Healy WL, Della Valle CJ, Iorio R, et al. Complications of total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Relat Res 2013;471:215-20. [Crossref] [PubMed]
- Nam D, Maher PA, Robles A, et al. Variability in the relationship between the distal femoral mechanical and anatomical axes in patients undergoing primary total knee arthroplasty. J Arthroplasty 2013;28:798-801. [Crossref] [PubMed]
- Nikolopoulos D, Michos I, Safos G, et al. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop 2015;6:469-82. [Crossref] [PubMed]
- Haruta Y, Kawahara S, Tsuchimochi K, et al. Deviation of femoral intramedullary alignment rod influences coronal and sagittal alignment during total knee arthroplasty. Knee 2018;25:644-9. [Crossref] [PubMed]
- Glasser J, Mariorenzi M, Blood T, et al. Distal femoral valgus cut angles unreliable in total knee arthroplasty. J Orthop 2021;24:29-33. [Crossref] [PubMed]
- Du YQ, Sun JY, Ni M, et al. Re-revision surgery for re-recurrent valgus deformity after revision total knee arthroplasty in a patient with a severe valgus deformity: A case report. World J Clin Cases 2019;7:3562-8. [Crossref] [PubMed]
- Huang TW, Kuo LT, Peng KT, et al. Computed tomography evaluation in total knee arthroplasty: computer-assisted navigation versus conventional instrumentation in patients with advanced valgus arthritic knees. J Arthroplasty 2014;29:2363-8. [Crossref] [PubMed]
- Johal P, Hassaballa MA, Eldridge JD, et al. The Posterior Condylar Offset Ratio. Knee 2012;19:843-5. [Crossref] [PubMed]
- Rhee SJ, Cho JY, Choi YY, et al. Femoral Periprosthetic Fractures after Total Knee Arthroplasty: New Surgically Oriented Classification with a Review of Current Treatments. Knee Surg Relat Res 2018;30:284-92. [Crossref] [PubMed]
Cite this article as: Song SJ, Lee HW, Kim YK, Park CH. Fixed distal femoral resection with a valgus cutting angle of 3° is more appropriate in intra-articular valgus deformity than juxta-articular valgus deformity in total knee arthroplasty: a retrospective single center study. Ann Joint 2022;7:35.


