
Tibial condylar valgus osteotomy for the treatment of intra-articular varus deformity of the knee
Introduction
Osteotomies around the knee are major research topics in orthopaedic surgery. The increasing incidence and distribution of primary and post-traumatic knee osteoarthritis (OA) combined with the variable long-term results of total and partial knee replacement in the young and active population has renewed interest in these joint-preserving procedures (1,2). This surgery’s main indications are (I) unicompartmental knee OA associated with malalignment; (II) correction of post-traumatic or congenital deformities (3,4). Medial knee OA associated with varus deformity is usually treated with a high tibial osteotomy (HTO). This procedure corrects metaphyseal deformity by shifting the mechanical axis and weight-bearing from the medial to the lateral tibial plateau, reducing the medial compartment’s overload. The treatment results in pain relief, OA progression reduction and promotes osteochondral repair. Currently, HTO is considered a safe and effective procedure when performed in selected patients with medial knee OA and metaphyseal varus deformity (5).
Nevertheless, in some patients, the deformity may result from an intra-articular defect instead of the typical metaphyseal deformity of the tibia or the femur. Those situations, such as the medial tibia plateau depression (the so-called “pagoda deformity”) or an OA-related joint narrowing, could not be corrected by an extra-articular surgical procedure (3). Furthermore, performing HTO in intra-articular deformities fail to restore femorotibial joint congruence resulting in joint instability and teeter effect (6). To manage intra-articular deformities, in 1992, Chiba et al. described a new surgical technique for advanced medial knee OA with lateral joint subluxation called tibial condylar valgus osteotomy (TCVO) (7). It consists of a type of open wedge high tibial osteotomy (OWHTO) that aims to restore joint congruence and reduce lateral joint subluxation using an L-shaped osteotomy (8). This surgical technique was slowly spread and is currently performed to treat knee deformities characterized by joint space (JS) narrowing and an increased joint line convergence angle (JLCA). The main indications for intra-articular osteotomies are medial knee OA, complex multiplanar deformity following tibial plateau malunions and post-traumatic or developmental deformities such as Blount disease. Currently, only a few papers in the literature describe the use of TCVO for the treatment of intra-articular deformities and the indications, similarly to the surgical technique, are different and not well defined. This review aims to summarize and discuss the indications, surgical techniques, and outcomes of intra-articular osteotomies to support the orthopaedic surgeon in choosing between the different treatments available.
Surgical indications
The clinical and radiological indications for TCVO have not been standardized yet. However, several authors (8-11) reported many complementary indications summarized and listed in Table 1. Chiba et al. recommended TCVO in patients with advanced medial unicompartmental knee OA, corresponding to a Kellgren-Lawrence (K-L) grade III–IV, with lateral joint line widening and range of motion (ROM) >90° and flexion contracture <10° (8). Furthermore, TCVO could be performed in knees with more severe varus deformity and medial knee OA than HTO (10) since different studies reported poor outcomes for HTO in the setting of severe OA (K-L grade > III) or high degrees of varus deformity (12-14).
Table 1
| Author and publication year | Indications for TCVO |
|---|---|
| Chiba et al. 2017, (8) | Middle-advanced medial unicompartmental knee OA (K-L III–IV) |
| Enlargement of the lateral joint line | |
| Flexion contracture <10° and a flexion >90° | |
| Ji et al. 2019, (9) | Preoperative JLCA >6° |
| Higuchi et al. 2019, (10) | %MA 5–15% |
| FTA 183°–186° | |
| MTPD −10° to −4° | |
| JLCA 4°–6° | |
| Lateral tibial thrust >1 cm | |
| Varus stress angle 6°–8° | |
| Laxity angle 7°–11° | |
| Kuwashima et al. 2020, (11) | Middle-advanced medial knee OA (K-L grade III–IV). |
| Tibial plateau morphology: | |
| Convex-type (“pagoda-type”): major indication | |
| Flat-type: controversial, appropriate in cases of excessive ligamentous laxity | |
| Depression-type: contraindication | |
| Preoperative JLCA >5° | |
| Flexion contracture <10° and a flexion >90° |
TCVO, tibial condylar valgus osteotomy; OA, osteoarthritis; K-L, Kellgren-Lawrence; %MA, percentage of the mechanical axis; FTA, femoro-tibial angle; MTPD, medial tibial plateau depression; JLCA, joint line convergence angle.
Several patients with varus deformity and medial knee OA have a pathological medial tibial plateau depression (MTPD) that result in an increased JLCA, leading to a deformity that HTO could not correct. Higuchi et al. (10) recommended TCVO for a percentage of the mechanical axis (%MA) 5–15%, femorotibial angle (FTA) of 183°–186°, MTPD between −10° and −4°, JLCA from 4° to 6°. Moreover, the authors performed TCVO in patients with lateral tibial thrust >1 cm, considering this procedure suitable for severe coronal ligament laxity. Varus stress angle between 6° and 8° and laxity angle between 7° and 11° are considered indications for TCVO too because it may increase joint stability without any ligaments’ reconstruction (10). Ji et al. identified a preoperative JLCA >6° as a tipping point for unacceptable postoperative JLCA performing HTO, suggesting an intra-articular osteotomy alternatively (9).
Kuwashima et al. (11), in their review, aimed to define indications for TCVO. According to the authors, this surgery should be performed for middle-advanced knee OA (K-L III–IV), as reported in other papers (8,10). Moreover, they identified the convex-type tibial plateau, also known as “pagoda-type”, as the main indication for TCVO because it is commonly characterized by more significant laxity of the lateral compartment. Conversely, the recommendation for the flat-type was controversial and may be suitable in cases of excessive ligamentous laxity. At the same time, depression-type was a contraindication for TCVO. Furthermore, the authors considered a preoperative JLCA greater than 5° as an elective criterion for this procedure suggesting TCVO could be performed in patients with knee flexion contracture <10° and a flexion >90° due to the difficulty of increasing knee flexion with this technique. No upper age limits for TCVO were reported (11).
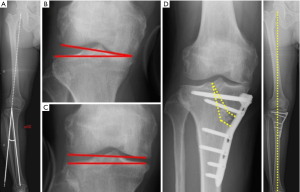
Kuwashima et al. (11), in their preoperative planning, analyzed and compared two angles: α60 and β. Two lines delimit the α60 angle with the Fujisawa point in common. The first line originates from the hip’s centre, while the second one from the ankle’s centre. The β angle is calculated by adding varus and valgus stress JLCA and multiplying the result by 1.5 (Figure 1). An α60 angle greater than the β angle is predictive of postoperative under-correction by performing only TCVO. In these cases, additional extra-articular osteotomies such as HTO or distal femoral osteotomy (DFO) should be considered to obtain the correct alignment.
TCVO may also be recommended for treating degenerative conditions, selected developmental and post-traumatic deformities (4,15,16). Due to incongruity and instability, tibial plateau malunion leads to knee OA, resulting in pain and functional impairment. A closing wedge intra-articular resection of the tibial plateau could be indicated for the tibial plateau widening wider than the contralateral. An open wedge intra-articular osteotomy with medial joint line elevation may be performed in patients with medial plateau malrotation and depression by calculating the correction angle and comparing it to the physiological mechanical medial proximal tibial angle (mMPTA). This procedure, described by Paley, restores joint congruence, and corrects varus thrust (15).
In patients with Blount’s disease, the medial tibial plateau is varus, procurvatum and is often associated with the knee’s coronal instability. Paley performed an intra-articular osteotomy with an elevation of the medial hemiplateau, eventually associated with extra-articular HTO, to restore joint line and stability. Proximal tibial physis should be saved, particularly in girls under eight and boys under 10 years of age (15).
Moreover, some patients combine an intra-articular and a metaphyseal deformity; to manage this situation, Ji et al. (17) proposed a new surgical technique called “combined proximal tibial osteotomy” (CPTO). This procedure combines TCVO, and OWHTO cuts to provide a single surgical treatment for patients who would not be exclusively suitable for OWHTO or TCVO. Currently, only biomechanical studies have been performed. Further clinical studies will be helpful to demonstrate the efficacy and safety of this surgical procedure. Furthermore, Saito et al. described a double-level osteotomy combined with a tibial condylar valgus osteotomy (DLOTO) for intra- and extra-articular knee deformities (18). This procedure aims to obtain a correct limb alignment by restoring a normal mMPTA and mechanical lateral distal femoral angle (mLDFA), avoiding pathological joint line obliquity. According to the authors, two elements should be taken into account to consider DLOTO: the JLCA and the total tibial plateau inclination (TTPI). The latter is obtained by adding medial tibial plateau inclination (MTPI) and lateral tibial plateau inclination (LTPI). Therefore, DLOTO should be considered when the JLCA is greater than 6°, and the TTPI is lower than −10° with an LTPI greater than 5° (18).
Surgical technique
Preoperative planning
A complete clinical and radiological examination before intra-articular osteotomies is mandatory to analyze alignment defects, functional impairment, ROM, and lower limbs’ stability. Full-length leg X-rays in a standing position are performed to calculate leg alignment, considering the %MA, FTA, mLDFA and mMPTA. JLCA and JS width are evaluated to analyze joint deformity, while the difference in JLCA under varus and valgus stress is calculated for stability evaluation (8). Initially, preoperative planning was based on the correction of joint congruence and the lower limb alignment at the Fujisawa point using the static JLCA as a reference. The achieved intra-articular correction could be verified intraoperatively under X-ray control (7). Several authors (11,19) recently suggested that a JLCA evaluation under varus-valgus stress helped avoid an alignment under-correction performing TCVO.
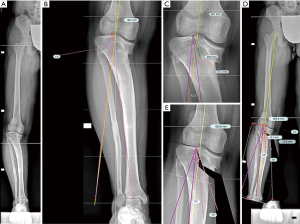
Nowadays, there is no unique, standardized preoperative planning for performing TCVO. In our institute, we usually plan the tibial correction angle according to the Miniaci method as the first step. The hinge point is centred on the lateral tibial spine and not on the lateral cortex as in OWHTO to plan the correction angle. This point corresponds to the apex of the vertical arm of the osteotomy. The horizontal arm is represented by a line that originates from the medial cortex of the tibia (about 4 cm from the joint line) and is projected to the apex of the fibular head; It intersects the vertical arm at the metaphyseal level. It is necessary to use dedicated software to simulate the TCVO cuts, mobilize the fragment to achieve the desired correction, and evaluate the opening gap in millimetres at the vertical and horizontal arms to obtain more accurate planning (Figure 2). In the preoperative planning, to avoid overcorrection due to the pathological JLCA (>2°), a well-established and simple formula is used: “the thumb rule”. It subtracts the resulting degrees of the following formula from the planned correction: (JLCA − 2°)/2° (20). Thus, for example, if the JLCA results of 8°, applying the described formula, a 3° of compensation should be considered. Otherwise, it is necessary to add one millimetre of correction to the planned clefts to restore the gap generated by the saw in the cuts. It is necessary to accurately reproduce intra-operatively the osteotomies because variations in the cuts or the angle subtended between them could reduce the reliability of the planning.
Intra-articular osteotomies for post-traumatic disorders cannot be standardized due to the wide variability of the malunions. X-ray evaluation is often non completely explanatory of multiplanar deformity, and a further investigation with computed tomography (CT) is required. A valuable resource for selected patients is three-dimensional (3D) virtual planning and patient-specific guides (16).
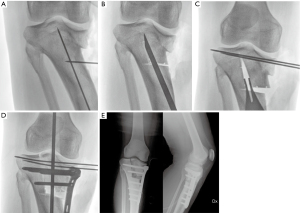
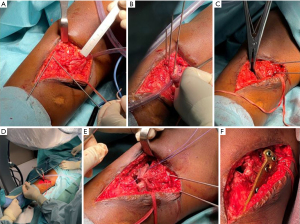
Surgical procedure for medial knee OA and Blount’s disease
An oblique skin incision is made on the medial side of the proximal tibia to perform TCVO. The anterior half pes anserinus and the superficial layer of the medial collateral ligament (MCL) are mobilized. The two arms of the “L-shaped” osteotomy are drawn on the tibia. The horizontal one is located about 4 cm from the tibia’s medial joint line, on a line connecting this point to the fibular head’s apex. The vertical arm connects the medial border of the patellar insertion on the tibial tuberosity and the intercondylar eminence.
The osteotomy of the vertical arm is performed with a saw and a chisel under fluoroscopic control. Next, it is recommended to cut the posterior cortex under a lateral fluoroscopic view to avoid damaging the popliteal vessels. Afterwards, the horizontal osteotomy arm is executed. Most authors suggest performing a valgus correction to achieve a 60–65% of the mechanical axis (7,11,18). A spreader should be inserted into the posterior cortical bone to avoid variations in the tibial slope. Before valgus correction is performed, two K-wires can be inserted parallel to the tibial plateau to avoid hinge instability. Finally, a T-shaped locking plate can be used for fixation (Figures 3,4).
Paley describes a similar Chiba technique for treating Blount’s disease or degenerative OA with medial plateau depression and knee subluxation. He performed an elevation of the medial tibial plateau to the same level as the lateral plateau, in both the sagittal and coronal plane, and a fixation with three 7.0 mm cannulated screws on the lateral side (15).
Cheng et al. (21) analyzed the biomechanical effects of screw orientation and plate profile on TCVO. A comparison between divergent and convergent screw positions and a comparison between straight and countered plate was performed. The authors reported that a divergent screw distribution resulted in greater stability to compressive and torsional loads, reducing the risk of implant failure, although the divergent distribution increased the risk of posterior cortex penetration and neurovascular injury. Furthermore, the same authors observed that a countered plate reduced the ability to stabilize the gap created and increased the risk of failure of the entire implant. The best choice to improve the construction’s stability while reducing the risk of implant failure was the combination of divergent screws and a straight plate (21). There is currently no standardized postoperative program in the literature that brings the different authors into an agreement. Chiba et al. (8) allow both full weight-bearing and ROM exercise from the postoperative day. According to Kuwashima et al. (11), active and passive ROM exercises can begin from the first postoperative day, but full weight-bearing is generally allowed at 1 week postoperatively. Patients undergoing additional osteotomies are generally assigned to a variable period of partial weight-bearing depending on the type of surgery performed. Saito et al. (18) also promote full recovery of knee ROM from the first day after the procedure; however, they recommend using two crutches for the first 6 postoperative weeks. Instead, athletic activities are allowed after the osteotomy gap has been filled.
Surgical procedure for post-traumatic proximal tibial plateau malunion with varus deformity
Post-traumatic fractures of the tibial plateau with varus deformities are challenging to treat. Wang et al. (22) described a standard approach to the proximal medial tibia using two types of patient-related 3D-printed guides. The first was an osteotomy guide shaped to the tibial cortical surface and temporally fixed with k-wires allowing to perform a multiplanar osteotomy. After that, the reduction guide was used to mobilize the osteotomy fragment and relocate it in the planned position mirrored on the contralateral knee. Finally, a bone graft was inserted into the open wedge, and the osteotomy was fixed with a T-plate. A postoperative program was not reported (22).
Pagkalos et al. (23), in their case report, described the treatment of a post-traumatic tibial malunion with bone projection into the intercondylar notch in a 19-year-old man. Firstly, the authors performed an arthroscopy to remove intra-articular bone excess. A posteromedial approach was used for osteotomies with a specific 3D-printed guide. Subsequently to the bone cuts, a T plate’s distal holes were used as a reference point to guide the osteotomy gap. Once the tibial plateau was restored, the gap was filled with a bone graft from the iliac crest. The postoperative program was no weight-bearing for 6 weeks, with no flexion restriction. At the 6-month follow-up, the authors reported an excellent outcome about pain and function.
Results
Chiba et al. (8) analyzed the clinical and radiological results of 10 patients who underwent TCVO after 5 years of follow-up. In the early postoperative months, patients reported a reduction in pain and stiffness and improved Visual Analogue Scale (VAS) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores. These results improved during follow-up. Radiological evaluations reported a reduction of JLCA from 6° preoperatively to 1° postoperatively, which demonstrated intra-articular correction. The preoperative value of JLCA in varus stress was 8°; in valgus stress, it was 0°. Postoperatively, JLCA in varus stress was reduced to 4°, while in valgus stress, it remained unchanged. The reduction of this angle difference demonstrated that greater joint stability was obtained.
In their retrospective study, Higuchi et al. (10) compared radiological parameters in 32 cases involving 35 knees who underwent HTO and the same numbers who underwent TCVO.
In the TCVO group, there was a more advanced knee OA, a significantly higher varus stress angle and laxity angle and a lower MTPD than in the HTO group. The postoperative evaluation demonstrated reliable results of TCVO with a reduction in JLCA and joint instability and an improvement in MTPD being maintained at 1 year of follow-up, similarly to HTO. Ji et al. (9) analyzed 66 patients who underwent HTO for medial knee OA. The lower extremities’ mechanical alignment was obtained because the average %MA increased from 5.5% to 60%, and mechanical femoro-tibial angle (mFTA) improved from 190.2° to 176.4°. The tibia was also corrected to the valgus, mMPTA shifted from 80.3° to 91.8° in the postoperative evaluation. There was a partial correction of intra-articular varus, and JLCA only changed from 4.2° to 2.7°. The authors demonstrated by multiple linear regression analysis that preoperative JLCA had a higher effect on the postoperative JLCA than mechanical alignment correction. Ji et al. (9) reported that patients with preoperative JLCA >6° were frequently associated with an unacceptable postoperative JLCA and a permanent femoro-tibial subluxation. Therefore, they considered patients with JLCA higher than 6° suitable for TCVO rather than HTO. Recently, Teramoto et al. (24) performed TCVOs on 145 patients and 171 knees with a mean follow-up of 5.4 years. Significant results were obtained regarding the alignment of the affected limb and the restoration of joint congruence. Such results were also confirmed by the positive clinical outcomes assessed by the Japanese Orthopaedic Association score (JOA score). The evaluation of stability to varus-valgus stress also provided satisfactory data, confirming the usefulness of TCVO in restoring joint stability. Paley (15) described the intra-articular osteotomy technique to treat post-traumatic malunion of the tibial plateau and developmental hypoplasia of the proximal tibia. The author performed nine intra-articular osteotomies to treat proximal tibia malunions with a follow-up between 28 and 108 months. Correct alignment, good ROM (average 105°) and knee stability were achieved. Patients had no pain during the follow-up. Paley performed 20 medial plateau elevations, some of them associated with an extra-articular osteotomy to treat Blount’s disease. Good knee stability and ROM was observed during the entire follow-up (from 2 to 20 years) without OA degeneration of the joint.
Discussion
Intra-articular knee osteotomies are a reasonable choice for treating some kinds of varus deformities of the lower limb, although the indications and surgical techniques are varied and not yet standardized.
TCVO is an intra-articular osteotomy that has become common, especially in Japan, and the developer of TCVO, Chiba et al. (7,8), reported that TCVO has never been an HTO. The main purpose of TCVO is to correct intra-articular deformities by restoring joint congruence and stability. Instead, HTO is performed in patients with extra-articular deformities to change the mechanical axis by shifting the load from the medial to the lateral side. Therefore, TCVO should not be considered a subtype of HTO. Teramoto, the greatest disciple of Chiba, followed this philosophy and reported good clinical results in many cases (6,24). Teramoto’s osteotomy could be called a “classic TVCO”. Nakayama et al. introduced the concept of lower limb alignment in TCVO. This concept is similar to traditional HTO, which could be called “advanced TCVO”, and consider the alignment’s correction as “an accessory benefit” that can be achieved (25). It is important to note that “classic TCVO” and “advanced TCVO” may look similar after performing the osteotomy, but their treatment philosophies are completely different. Furthermore, advanced TCVO is not always better than classic TCVO, so the correct choice of TVCO type depends on the underlying deformity.
HTO is a surgical technique that may correct the proximal tibia restoring the physiological values of the MPTA, but a complete correction of the JLCA and MTPD is not always achieved. TCVO, working intra-articularly, could correct the tibial plateau’s shape, improve the femorotibial congruence, and achieve normal values of JLCA, MPTA and MTPD. This procedure’s benefits are related to the increase in joint stability by realigning the lower limb axis, reducing the joint’s lateral subluxation, and redistributing the load towards the lateral compartment (8). Furthermore, TCVO increases femorotibial joint congruence and, making the tibial surface concave, increases cruciate ligament tension without additional surgical treatments (10). This aspect, still poorly discussed in the current literature, could reduce the invasiveness of surgery, and allow a faster functional recovery (26-28).
Moreover, in TCVO, limiting the osteotomy to the medial condyle provides some advantages, including reduced lateral hinge fracture and neurovascular injuries because long screw insertion with a higher risk of posterior cortical penetration is not required. In addition, the increased valgisation and lateralization of the mechanical axis result in better load distribution on the lateral compartment that is not involved in the osteotomy (8,10,11). This condition allows early weight-bearing and, consequently, a faster full recovery.
Recent studies have reported progressive degeneration of the patellofemoral joint (PFJ) after OWHTO (29-31). This condition is related to the change in patellofemoral alignment after the procedure. In TCVO, the variation in height’s tibial tuberosity is lesser than in OWHTO. Therefore, the impact on PFJ should be minimal (32). Nevertheless, few clinical studies in the literature evaluate this effect in the medium to long term.
The main aim of TCVO is to restore femorotibial congruence and, secondarily, to correct lower limb alignment. Patients without lateral joint subluxation should not undergo this type of surgery (8). Therefore, several authors observed that this surgical procedure’s main limitation is its limited effectiveness in correcting the varus mFTA (8-11). In addition, when the lateral joint is reduced, the mechanical axis cannot be shifted more towards the lateral compartment (8,10).
In those patients who require further valgus correction, additional procedures such as OWHTO and DFO should be considered to achieve the desired coronal alignment (11). Additionally, to the limited correction of the lower limb alignment, another problem of TCVO is related to the impossibility of directly modifying the soft tissue balance leading to a possible residual increase in medial tightness and lateral laxity (8,10).
Osteotomies and unicompartmental knee arthroplasty (UKA) are two surgical treatments with different indications. Several authors (33,34) reported that UKA might be an equally effective treatment with faster recovery for isolated medial compartment OA. UKA may undercorrect the mechanical axis in patients with a preoperative limb alignment with more than 10° in varus (35). Moreover, residual varus increases the implant’s overload, with potential failure due to polyethylene wear or aseptic loosening (36,37).
The limitations of this review on TCVO are related to the few papers in the literature with small sample size and limited follow-up. The patients included in the studies were not homogeneous because they were affected by intra-articular and metaphyseal deformities. Intra-articular osteotomies were not performed with the same surgical technique, and different plates were used to fix the osteotomy. Further studies with a larger and more homogeneous sample size with a longer follow-up will be needed to standardize TCVO indications and surgical techniques.
Conclusions
The main aim of tibial intra-articular osteotomies is to restore femorotibial joint congruency and joint stability. It represents an efficient alternative to OWHTO and DFO for the most frequent medial unicompartmental OA degeneration. It has an elective indication for rare post-traumatic injuries and congenital and developmental diseases. More studies with longer radiological and clinical follow-up are required to prove this surgical technique’s efficacy and safety.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-19/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wallace IJ, Worthington S, Felson DT, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A 2017;114:9332-6. [Crossref] [PubMed]
- Rathbun AM, Shardell MD, Ryan AS, et al. Association between disease progression and depression onset in persons with radiographic knee osteoarthritis. Rheumatology (Oxford) 2020;59:3390-9. [Crossref] [PubMed]
- Lobenhoffer P. Indication for Unicompartmental Knee Replacement versus Osteotomy around the Knee. J Knee Surg 2017;30:769-73. [Crossref] [PubMed]
- Lamm BM, Paley D. Deformity correction planning for hindfoot, ankle, and lower limb. Clin Podiatr Med Surg 2004;21:305-26. v. [Crossref] [PubMed]
- Day M, Wolf BR. Medial Opening-Wedge High Tibial Osteotomy for Medial Compartment Arthrosis/Overload. Clin Sports Med 2019;38:331-49. [Crossref] [PubMed]
- Watanabe Y, Takenaka N, Kinugasa K, et al. Intra- and Extra-Articular Deformity of Lower Limb: Tibial Condylar Valgus Osteotomy (TCVO) and Distal Tibial Oblique Osteotomy (DTOO) for Reconstruction of Joint Congruency. Adv Orthop 2019;2019:8605674. [Crossref] [PubMed]
- Chiba G. New tibial osteotomy for severe osteoarthritis of the knee with teeter effect. J Jpn Orthop Assoc 1992;66:798.
- Chiba K, Yonekura A, Miyamoto T, et al. Tibial condylar valgus osteotomy (TCVO) for osteoarthritis of the knee: 5-year clinical and radiological results. Arch Orthop Trauma Surg 2017;137:303-10. [Crossref] [PubMed]
- Ji W, Luo C, Zhan Y, et al. A residual intra-articular varus after medial opening wedge high tibial osteotomy (HTO) for varus osteoarthritis of the knee. Arch Orthop Trauma Surg 2019;139:743-50. [Crossref] [PubMed]
- Higuchi T, Koseki H, Yonekura A, et al. Comparison of radiological features of high tibial osteotomy and tibial condylar valgus osteotomy. BMC Musculoskelet Disord 2019;20:409. [Crossref] [PubMed]
- Kuwashima U, Yonekura A, Itoh M, et al. Tibial condylar valgus osteotomy - indications and technique. J Exp Orthop 2020;7:30. [Crossref] [PubMed]
- Efe T, Ahmed G, Heyse TJ, et al. Closing-wedge high tibial osteotomy: survival and risk factor analysis at long-term follow up. BMC Musculoskelet Disord 2011;12:46. [Crossref] [PubMed]
- Kamada S, Shiota E, Saeki K, et al. Severe varus knees result in a high rate of undercorrection of lower limb alignment after opening wedge high tibial osteotomy. J Orthop Surg (Hong Kong) 2019;27:2309499019846660. [Crossref] [PubMed]
- Orban H, Mares E, Dragusanu M, et al. Total knee arthroplasty following high tibial osteotomy - a radiological evaluation. Maedica (Bucur) 2011;6:23-7. [PubMed]
- Paley D. Intra-articular osteotomies of the hip, knee, and ankle. Oper Tech Orthop 2011;21:184-96. [Crossref]
- Kfuri M, Schatzker J. Corrective Intra-articular Osteotomies for Tibial Plateau Malunion. J Knee Surg 2017;30:784-92. [Crossref] [PubMed]
- Ji W, Luo C, Zhan S, et al. Combined proximal tibial osteotomy for varus osteoarthritis of the knee: Biomechanical tests and finite-element analyses. Knee 2020;27:863-70. [Crossref] [PubMed]
- Saito H, Yonekura A, Saito K, et al. A new double level osteotomy procedure to restore a joint line and joint angles in severe varus osteoarthritis. - Double level osteotomy associated with tibial condylar valgus osteotomy (DLOTO). Asia Pac J Sports Med Arthrosc Rehabil Technol 2020;24:9-13. [Crossref] [PubMed]
- Ogawa H, Matsumoto K, Ogawa T, et al. Preoperative varus laxity correlates with overcorrection in medial opening wedge high tibial osteotomy. Arch Orthop Trauma Surg 2016;136:1337-42. [Crossref] [PubMed]
- Micicoi G, Khakha R, Kley K, et al. Managing intra-articular deformity in high Tibial osteotomy: a narrative review. J Exp Orthop 2020;7:65. [Crossref] [PubMed]
- Cheng CT, Luo CA, Chen YC. Biomechanical effects of screw orientation and plate profile on tibial condylar valgus osteotomy - Finite-element analysis. Comput Methods Biomech Biomed Engin 2020;23:906-13. [Crossref] [PubMed]
- Wang H, Newman S, Wang J, et al. Corrective Osteotomies for Complex Intra-Articular Tibial Plateau Malunions using Three-Dimensional Virtual Planning and Novel Patient-Specific Guides. J Knee Surg 2018;31:642-8. [Crossref] [PubMed]
- Pagkalos J, Molloy R, Snow M. Bi-planar intra-articular deformity following malunion of a Schatzker V tibial plateau fracture: Correction with intra-articular osteotomy using patient-specific guides and arthroscopic resection of the tibial spine bone block. Knee 2018;25:959-65. [Crossref] [PubMed]
- Teramoto T, Harada S, Takenaka N, et al. Tibial condylar valgus osteotomy (TCVO): Surgical technique and clinical results for knee osteoarthritis with varus deformity. J Clin Orthop Trauma 2021;22:101589. [Crossref] [PubMed]
- Nakayama H, Akiyama T, Kondo E, et al. Tibial Condylar Valgus Osteotomy Combined With Medial Open-Wedge Distal Tuberosity Tibial Osteotomy. Arthrosc Tech 2022;11:e569-75. [Crossref] [PubMed]
- Li Y, Zhang H, Zhang J, et al. Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: a systematic review. Arthroscopy 2015;31:507-19. [Crossref] [PubMed]
- Naudie DD, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med 2004;32:60-70. [Crossref] [PubMed]
- Dean CS, Liechti DJ, Chahla J, et al. Clinical Outcomes of High Tibial Osteotomy for Knee Instability: A Systematic Review. Orthop J Sports Med 2016;4:2325967116633419. [Crossref] [PubMed]
- Goshima K, Sawaguchi T, Shigemoto K, et al. Patellofemoral Osteoarthritis Progression and Alignment Changes after Open-Wedge High Tibial Osteotomy Do Not Affect Clinical Outcomes at Mid-term Follow-up. Arthroscopy 2017;33:1832-9. [Crossref] [PubMed]
- Kim KI, Kim DK, Song SJ, et al. Medial Open-Wedge High Tibial Osteotomy May Adversely Affect the Patellofemoral Joint. Arthroscopy 2017;33:811-6. [Crossref] [PubMed]
- Tanaka T, Matsushita T, Miyaji N, et al. Deterioration of patellofemoral cartilage status after medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2019;27:1347-54. [Crossref] [PubMed]
- Koseki H, Yonekura A, Horiuchi H, et al. L-shaped tibial condylar valgus osteotomy for advanced medial knee osteoarthritis: a case report. Biomed Res 2017;28:4878-82.
- Kleeblad LJ, Zuiderbaan HA, Hooper GJ, et al. Unicompartmental knee arthroplasty: state of the art. J ISAKOS 2017;2:97-107. [Crossref]
- Mootanah R, Imhauser CW, Reisse F, et al. Development and validation of a computational model of the knee joint for the evaluation of surgical treatments for osteoarthritis. Comput Methods Biomech Biomed Engin 2014;17:1502-17. [Crossref] [PubMed]
- Heijens E, Kornherr P, Meister C. The coronal hypomochlion: a tipping point of clinical relevance when planning valgus producing high tibial osteotomies. Bone Joint J 2016;98-B:628-33. [Crossref] [PubMed]
- Raja Izaham RM, Abdul Kadir MR, Abdul Rashid AH, et al. Finite element analysis of Puddu and Tomofix plate fixation for open wedge high tibial osteotomy. Injury 2012;43:898-902. [Crossref] [PubMed]
- Amis AA. Biomechanics of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:197-205. [Crossref] [PubMed]
Cite this article as: Capella M, Risitano S, Sabatini L, Faccenda C, Barberis L, Camazzola D, Bosco F, Giustra F, Massè A. Tibial condylar valgus osteotomy for the treatment of intra-articular varus deformity of the knee. Ann Joint 2022;7:37.


