
Morphologic analysis of the sublime tubercle: considerations in the approach to ulnar collateral ligament reconstruction
Introduction
Elbow injuries in baseball players, especially involving the ulnar collateral ligament (UCL), have been increasing over the last two decades (1,2). Hallmarked by medial elbow pain and decreased velocity, UCL injuries significantly affect the performance and career of athletes (3,4). Much research has been performed on the excessive amount of competitive throwing, year-round baseball, throwing breaking pitches (especially before age 14), high fastball velocity (over 80 mph), showcase events, and inadequate warm-ups, as well as reconstruction techniques and outcomes (2,5-7).
The soft tissue attachment and relationship of the anterior bundle of the UCL to the sublime tubercle is important for successful operative treatment (2). However, to our knowledge, no research has been published to date specifically evaluating the morphology of the sublime tubercle of the proximal ulna in an anterior-to-posterior plane. Given the increased incidence of UCL injuries and the projected increase in reconstruction procedures, a robust understanding of the morphologic nature of the UCL and sublime tubercle is crucial (5,8).
The purpose of this morphologic analysis is to examine the anatomic variations of the sublime tubercle relative to the ulna. Knowledge of this location plays an integral role in surgical planning. We present the following article in accordance with the STROBE reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-20/rc).
Methods
Selection process
The University of South Florida, Department of Radiology maintains an anonymized research database of medical image data. This data was collected under IRB approval for Human Subject Research following all ethical policies for patient data research. All scans were clinically ordered for diagnostic imaging as part of the patient’s standard of clinical care and therefore, no individuals were subjected to any radiation for research purposes. These computed tomography (CT) scans were then extracted without any patient health information (PHI), including age and sex, that were sourced from the hospital picture archiving and communication system (PACS) in Digital Imaging and Communications in Medicine (DICOM) format. Each CT scan was given a unique alphanumerical identity (ID) of 6 letters and/or numbers. A total of 91 CT scans were identified that included the anatomy of interest. Each dataset was screened for inclusion/exclusion criteria. Studies were included if the entirety of the proximal ulna was captured in the scan field of view (FOV). Scans were excluded if the ulna was only partially captured, if there was evidence of an unhealed or healed fracture, any surgical intervention, or identifiable pathology, including but not limited to arthritis, congenital malformation, or osteosarcoma. Sixty-six CT scans were excluded, and 25 elbows met criteria for analysis. These CT images were then imported into the Mimics Innovation Suite 24.0 (Leuven, Belgium) for morphologic analysis. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Twenty-five de-identified CT scans were obtained for morphological analysis of the sublime tubercle at our University’s Department of Radiology. Informed consent was waived due to the de-identified nature of this study. IRB determined the study was exempt due to the de-identified nature of this study.
Morphologic analysis
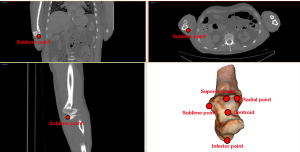
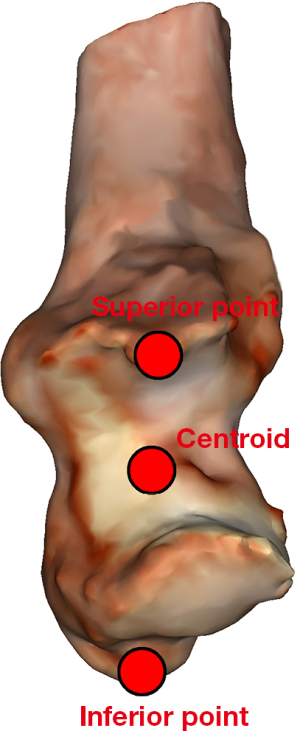
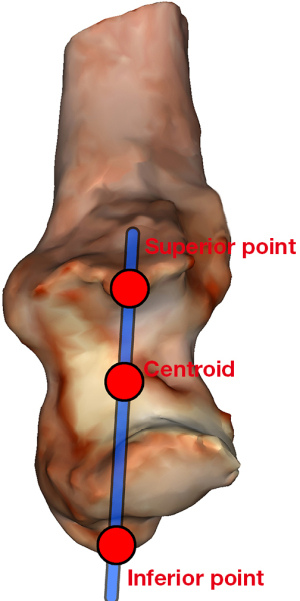
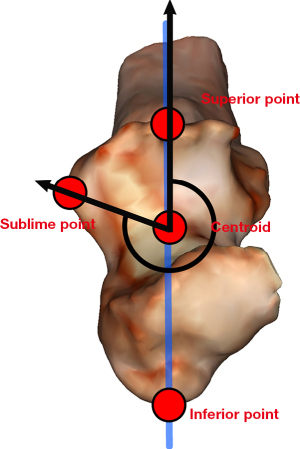
The following analytic procedure was conducted for each elbow. The proximal ulna was initially segmented using a bone threshold (≥226 Hounsfield units). Hand-segmentation was used to separate the ulna from the humerus and radius and subsequent 3D models were generated of the proximal ulna (Figure 1). The central line of the proximal ulna was measured by placing a landmark on three locations: the midpoint of the trochlear notch, the most superior point of the trochlear notch, and the most inferior point of the olecranon (Figure 2). A central line intersecting the midpoint of the trochlear notch was then created from the superior to inferior landmarks and used as a point of reference for the sublime angle (Figure 3). The length of this central line was also measured. The sublime tubercle was then marked and a line was formed from the sublime tubercle to the midpoint of the trochlear notch. This distance was also captured. The sublime angle, produced from the central line and the line from the midpoint of the trochlear notch to the sublime tubercle, was then measured (Figure 4). For left ulnae, the inverse of this angle was calculated by using the following formula: 360˚ − measured sublime angle (°) = true sublime angle (°).
Statistical analysis
Measurements of central tendency were calculated for the distance of the sublime tubercle to the midpoint of the trochlear notch, the maximum distance of the central line, and the sublime angle. The sublime angle was also converted to an o’clock format in which the “hour” signified the location of the sublime tubercle in relation to the central line. After the conversion, the hour was rounded up or down to the nearest hundredth of an hour. Microsoft ExcelTM 2022 was used to calculate mean values, standard deviations, and ranges for continuous variables.
Results
The sublime tubercle of the ulna was identified in all 25 CT scans. Due to the use of a de-identified database, no demographic data was available. The average maximum distance of the proximal ulnae in the anteroposterior plane, or the most superior to most inferior landmarks intersecting the midpoint of the trochlear notch, was 42.27±4.09 mm (range, 36.31–49.73 mm). The average distance of the most medial aspect of the sublime tubercle from the midpoint of the trochlear notch was 15.18±3.67 mm (range, 5.57–22.55 mm). All left elbow angle and clock-face values were converted to right elbow values for analysis.
The average sublime tubercle angle from the midpoint of the trochlear notch was 282.53°±8.8° (range, 271.19°–305.04°). There was only one sublime tubercle angle over 300°. The sublime tubercle angle was then equated to a clock face to provide a vernacular descriptor commonly used by surgeons to localize direction of structures. The 12, 3, 6, and 9 o’clock positions correlate to 0°, 90°, 180°, and 270°, respectively. The conversion placed the sublime tubercle at 9.42°±0.29° (range, 9.04°–10.17°), roughly half past 9 (Figure 5). Results can be seen in Table 1.
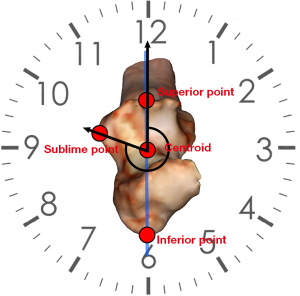
Table 1
| Descriptive statistics | Sublime distance (mm) | Central line length (mm) | Sublime angle (°) | O’clock angle (°) |
|---|---|---|---|---|
| Mean | 15.18 | 42.27 | 282.53 | 9.42 |
| SD | 3.67 | 4.09 | 8.80 | 0.29 |
| Min | 5.57 | 36.31 | 271.19 | 9.04 |
| Max | 22.55 | 49.73 | 305.04 | 10.17 |
SD, standard deviation; Min, minimum; Max, maximum.
Discussion
This study examined the osseous morphology of the sublime tubercle as it relates to the anterior-to-posterior plane of the proximal ulna. We determined the mean distance from the sublime tubercle to the midpoint of the trochlear notch to be approximately 15.2 mm in an anterior-to-posterior plane. UCL injuries have increased over the last two decades in overhead throwers, especially baseball players (2,5,7,9). Ciccotti et al. found that the overall return to play is relatively strong at 79.9% of professional pitchers returning with 71.2% returning to the same level of performance (2). The financial and time-related costs associated with UCL injuries in professional baseball are significant (10). A robust knowledge of proximal ulnar anatomy is required for the development of novel reconstruction techniques to continue to improve the surgical treatment of UCL injuries.
The validity of our results is strengthened by similar findings utilizing different methodologies. Cage et al. used digital calipers to measure the insertion of the anterior bundle of the UCL from the coronoid tip while Rausch et al. used individually calibrated images of cadaveric dissections to standardize measurements from the lesser sigmoid notch (8,11). Using these methods, the ventral aspect of the anterior bundle of the UCL and coronoid tip were a mean distance of 18.4 mm dorsal to the coronoid tip as described by Cage et al. and 7.8 mm from the coronoid tip in a sagittal line as described by Rausch et al (8,11). Farrow et al. found a mean distance between the sublime tubercle to the posterior articular margin of the lesser sigmoid notch to be 5.5±1.0 mm with digital calipers and 5.8±1.3 mm using CT scans with 3D reconstructions and digital measuring tools (12). Although these methods cannot be directly compared due to the differences in techniques, they provide various reference points for accurately determining the sublime tubercle landmark. The mean distance from the midpoint of the trochlear notch to the sublime tubercle was 15.18±3.67 mm (range, 5.57–22.55 mm). This distance is congruent in magnitude with the other studies measuring the sublime tubercle from both the coronoid tip and the posterior articular margin of the lesser sigmoid notch (8,11).
Variations in previously described UCL anterior bundle insertions have been reported with insertions 1–4 mm from the articular surface on the sublime tubercle (8,13-16). These variations, albeit small, may show a relationship with any morphologic variations of the sublime tubercle itself. Rausch et al. evaluated the relationship of the anterior bundle of the UCL to the coronoid tip and reported high variance (11). However, they did not examine the relationship to the sublime tubercle or evaluate any variations in the osseous morphology of the sublime tubercle. Ikezu et al. and Hoshika et al. have demonstrated variations in not only the relationship between the tendinous structures of the medial elbow and the UCL but also the relationship between their insertion on the sublime tubercle (14,17). Hoshika et al. suggested reconsideration of the anterior bundle of the UCL given their findings and the shared insertions related to the sublime tubercle (14). We believe that the various medial elbow anatomical descriptions and variations demonstrate the importance of characterizing the morphology of the sublime tubercle since this osseous landmark is frequently discussed and referenced. This relationship is vital to UCL reconstruction techniques which anchor the grafts around the sublime tubercle (18,19). Multiple studies have examined the medial elbow anatomy, but to our knowledge none have specifically examined the osseous morphology of the sublime tubercle in anterior-to-posterior plane described in this study (8,11,13-17).
This study has several limitations. CT was the only modality used to evaluate the osseous morphology of the sublime tubercle. However, the consistency of this method has been verified in previous similar work analyzing the sublime tubercle (12). Another limitation is the small sample size, although we believe that this study should be assessed in conjunction with other CT-based morphologic studies, which provide further evidence of this technique as a viable means of evaluating osseous morphology. The use of a de-identified database potentially introduces inadvertent selection bias and limits the applicability to throwers. Since there was a relatively wide range of sublime tubercle positions in our cohort of 25 elbows, there may be larger variance found in the population at large. Future studies could address the position of the sublime tubercle in larger populations as well as throwers in particular.
Conclusions
In conclusion, the importance of understanding any anatomic variations of the sublime tubercle is paramount in properly restoring the kinematics of UCL reconstruction. We analyzed the morphology of the sublime tubercle in the anterior-to-posterior plane to evaluate variations in the anatomy of this integral structure. Our findings demonstrate that the bony morphology of the sublime tubercle can be expected to have a consistent medial location between 9 and 10 o’clock on a right elbow (2 and 3 o’clock on the contralateral elbow).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-20/rc
Data Sharing Statement: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-20/dss
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-20/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-20/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rothermich MA, Fleisig GS, Conte SA, et al. Short-Term Trends in Elbow Ulnar Collateral Ligament Surgery in Collegiate Baseball Players: An Analysis of 25,587 Player-Years. Orthop J Sports Med 2021;9:23259671211016846. [Crossref] [PubMed]
- Ciccotti MG, Pollack KM, Ciccotti MC, et al. Elbow Injuries in Professional Baseball: Epidemiological Findings From the Major League Baseball Injury Surveillance System. Am J Sports Med 2017;45:2319-28. [Crossref] [PubMed]
- Solomito MJ, Garibay EJ, Nissen CW. Deceleration phase elbow varus moments: a potential injury mechanism for collegiate baseball pitchers. Sports Biomech 2021;20:629-38. [Crossref] [PubMed]
- Bullock GS, Menon G, Nicholson K, et al. Baseball pitching biomechanics in relation to pain, injury, and surgery: A systematic review. J Sci Med Sport 2021;24:13-20. [Crossref] [PubMed]
- Griffith TB, Ahmad CS, Gorroochurn P, et al. Comparison of Outcomes Based on Graft Type and Tunnel Configuration for Primary Ulnar Collateral Ligament Reconstruction in Professional Baseball Pitchers. Am J Sports Med 2019;47:1103-10. [Crossref] [PubMed]
- Petty DH, Andrews JR, Fleisig GS, et al. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med 2004;32:1158-64. [Crossref] [PubMed]
- Zaremski JL, Vincent KR, Vincent HK. Elbow Ulnar Collateral Ligament: Injury, Treatment Options, and Recovery in Overhead Throwing Athletes. Curr Sports Med Rep 2019;18:338-45. [Crossref] [PubMed]
- Cage DJ, Abrams RA, Callahan JJ, et al. Soft tissue attachments of the ulnar coronoid process. An anatomic study with radiographic correlation. Clin Orthop Relat Res 1995;154-8. [PubMed]
- Conway JE, Jobe FW, Glousman RE, et al. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am 1992;74:67-83. [Crossref] [PubMed]
- Conte S, Camp CL, Dines JS. Injury Trends in Major League Baseball Over 18 Seasons: 1998-2015. Am J Orthop (Belle Mead NJ) 2016;45:116-23. [PubMed]
- Rausch V, Wegmann S, Hackl M, et al. Insertional anatomy of the anterior medial collateral ligament on the sublime tubercle of the elbow. J Shoulder Elbow Surg 2019;28:555-60. [Crossref] [PubMed]
- Farrow LD, Mahoney AJ, Stefancin JJ, et al. Quantitative analysis of the medial ulnar collateral ligament ulnar footprint and its relationship to the ulnar sublime tubercle. Am J Sports Med 2011;39:1936-41. [Crossref] [PubMed]
- Dugas JR, Ostrander RV, Cain EL, et al. Anatomy of the anterior bundle of the ulnar collateral ligament. J Shoulder Elbow Surg 2007;16:657-60. [Crossref] [PubMed]
- Hoshika S, Nimura A, Yamaguchi R, et al. Medial elbow anatomy: A paradigm shift for UCL injury prevention and management. Clin Anat 2019;32:379-89. [Crossref] [PubMed]
- Munshi M, Pretterklieber ML, Chung CB, et al. Anterior bundle of ulnar collateral ligament: evaluation of anatomic relationships by using MR imaging, MR arthrography, and gross anatomic and histologic analysis. Radiology 2004;231:797-803. [Crossref] [PubMed]
- Timmerman LA, Schwartz ML, Andrews JR. Preoperative evaluation of the ulnar collateral ligament by magnetic resonance imaging and computed tomography arthrography. Evaluation in 25 baseball players with surgical confirmation. Am J Sports Med 1994;22:26-31; discussion 32. [Crossref] [PubMed]
- Ikezu M, Edama M, Matsuzawa K, et al. Morphological Features of the Ulnar Collateral Ligament of the Elbow and Common Tendon of Flexor-Pronator Muscles. Orthop J Sports Med 2020;8:2325967120952415. [Crossref] [PubMed]
- Meyers KN, Middleton KK, Fu MC, et al. Comparison of a Novel Anatomic Technique and the Docking Technique for Medial Ulnar Collateral Ligament Reconstruction. Am J Sports Med 2022;50:1061-5. [Crossref] [PubMed]
- Chang ES, Le AH, Looney AM, et al. Biomechanical Comparison of Anatomic Restoration of the Ulnar Footprint vs Traditional Ulnar Tunnels in Ulnar Collateral Ligament Reconstruction. Am J Sports Med 2022;50:1375-81. [Crossref] [PubMed]
Cite this article as: Phillips J, Martin D, Ford J, Panas K, Bauer A, Salomon K, Albers J, Decker S, Nofsinger C. Morphologic analysis of the sublime tubercle: considerations in the approach to ulnar collateral ligament reconstruction. Ann Joint 2022;7:31.


