Do meniscal repairs with meniscus cyst do better than meniscectomy?—a systematic review of meniscal cyst treatment
Highlight box
Key findings
• Both arthroscopic decompression and open cystectomy are viable options for dealing with a meniscal cyst.
• Open cystectomy appears to be associated with lower cyst recurrences and complications.
• There is inconclusive evidence to determine if treatment of the meniscal tear, repair or debridement, affects the outcomes of the meniscal cyst.
What is known and what is new?
• Meniscal tears have been found to be commonly associated with a meniscal cyst, especially in horizontal meniscal tears.
• This systematic review looks at the various types of treatment of the meniscal tear and how it affects outcomes and recurrence of the meniscal cyst.
What is the implication, and what should change now?
• More high-quality studies should be done to determine how repairs or debridements of the associated meniscal tears affect the outcomes and recurrence of meniscal cysts.
Introduction
Meniscal cysts have gained attention due to the complexity of surgical management, especially with the additional component of the corresponding meniscal tear. Most commonly, horizontal meniscal tears have been implicated in the formation of meniscal cysts (1), with varying rates of incidence reported. Wroblewski reported 50% (2) incidence of meniscal tears while Reagan et al had 84% (3) and some others were even able to show 100% association with meniscal tears (1,4,5). Various theories have been put forth to account for the development of meniscal cysts, attributing it to myxoid degeneration of collagen (6), while others have also postulated that they develop from an inflow of synovial fluid resulting from a meniscal tear instead. The meniscal cysts may result from the dual pathways of synovial fluid inflow and myxoid degeneration (6).
The recent advent of horizontal meniscus tear repair and the improved techniques to repair them have also increased the interest in repairs of this tear pattern (7). Previously what was considered as a meniscus tear pattern not amenable to repair, there is now data to show that such tears when repaired can achieve good clinical outcomes on par with other tear patterns (8).
Lateral meniscal cysts have been found to be more common than that on the medial side and predominantly affecting men. Seger et al. reported a ratio of 10:1 (4) favouring the lateral meniscus as compared the medial side. However, newer studies using MRI as a main modality of investigation (9-11), as compared to previous arthroscopic or surgical methods, have shown that medial meniscal cysts are more common than previously thought (10,11). Campbell et al. showed a 2:1 ratio of medial meniscal as compared to lateral meniscal cysts (10).
Previously, most meniscal cysts were treated surgically with open cystectomy and total meniscectomy (12). However, that led to inevitable degenerative changes in the long term. Flynn and Kelly (13) were able to achieve good results with local excision of meniscal cyst with an attempt to preserve the meniscus as far as possible if no meniscal tears were found intraoperatively. They reported no recurrences and showed earlier return to work (13). As arthroscopy and surgical techniques improved, treatment now involves arthroscopic management of the meniscal lesion with decompression of the cyst (14) or open cystectomy. Co-existing meniscal tears, if found, were mostly debrided until a stable rim was achieved (4,15-17). A recent systematic review by Haratian et al. (18) showed that arthroscopic management of cysts can provide satisfactory outcomes for patients with good return to sport. However, it is not clear whether the treatment of the co-existing meniscal tears can affect the outcomes achieved.
This paper aims to review current literature available to compare the outcomes between arthroscopic and open surgeries for treatment of the meniscal cyst, as well as the clinical outcomes for meniscal repair in contrast to meniscal debridement, focusing on literature in the last 10 years and only studies of Level IV evidence and above. We present the following article in accordance with the PRISMA reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-29/rc). This systematic review is not registered.
Methods
Literature search
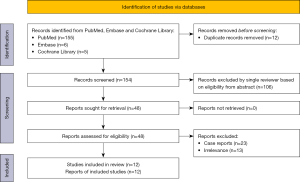
A literature search of PubMed, Embase and Cochrane was carried out by a single reviewer using the following keywords in combination: meniscal, meniscus, cyst, treatment. If the abstract matched the topic, the full article was assessed by a single reviewer. Of which, the studies were then shortlisted and evaluated for the following: (I) journal of publication; (II) year of publication; (III) country and language; (IV) level of evidence; (V) whether arthroscopic treatment or open treatment was adopted; (VI) number of cases of meniscal cysts that are associated with meniscal tears; (VII) treatment of meniscal cyst.
Thereafter, the articles were screened based on their titles and abstract for relevance. The full texts of the remaining articles were retrieved and assessed for inclusion into this systematic review. All articles were reviewed by a senior author.
Eligibility criteria
All clinical studies investigating treatment of meniscal cysts were considered for inclusion. Only articles with the following are included:
- Papers published from year 2000–2020;
- Level of evidence IV and above according to the Journal of Bone and Joint Surgery were included (19);
- Papers that were in English and involving human studies;
- Minimum duration of follow-up of at least 12 months.
Outcomes of interest
Study generalities (author, year, journal), surgical technique and related patient baseline data (type of procedures, mean age, gender proportion, duration of follow-up, complications) were recorded. Data concerning the satisfaction and different clinical scores were collected. For example, the Lysholm Knee Scoring Scale, Visual Analogue Scale (VAS) and the categorical scores.
Methodological quality assessment
The Coleman methodology score (CMS) was used to assess the quality of the studies, accounting for chance, biases, and confounding factors. Even though the CMS was initially developed for use in patella tendinopathy, modifications have been allowed for other trial designs due to the similarities in the subsections of the CMS as well as the Consolidated Standards of Reporting Trials (CONSORT) statement. The CMS comprises of a score ranging from 0 to 100, a higher score indicates a lower probability of various biases, confounding factors, and chance (20).
Results
Search result
The initial literature search produced a total of 166 articles across PubMed, EMBASE and Cochrane with 12 duplicates. The literature search from EMBASE resulted in 6 papers, and that of the Cochrane library resulted in 5 papers. Of these 6 papers from EMBASE, 1 was included in this study after assessing relevance of the abstract. Finally, there were a total of 12 studies included in this review (Figure 1). We have included Tudisco et al. (21) and Haklar et al. (22) in our review for further analysis; where the number of meniscal tears in their cohort was not documented, but they recorded details of meniscal tear treatment.
Patient demographics
From the 12 studies (6,21-31) included in this systematic review, the weighted mean follow-up duration was 41.4 months, and the weighted mean age of the patients was 35.1 years. Meniscal cysts mostly affected men, with 334 male patients (63.74%) and 190 female patients (36.26%), agreeing with a generally male predominant population as compared to other studies.
The details and characteristics of all 12 studies included in this systematic review have been summarised in Table 1 and Table 2.
Table 1
| Author | Year | Journal published | Level of evidence | Modified CMS | Surgical method(s) | Number of patients | Number of meniscal cysts | Number of meniscal tears | Mean age, in years [range] | Mean follow-up in months [range] | Clinical outcome scoring system | Number of cyst recurrences | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tudisco et al. (21) | 2000 | American Journal of sports medicine | IV | 39 | Arthroscopy | 19 | 19 | – | 33.5 [20–53] | 39.6 [24–60] | Cerullo evaluation scale | 0 | – |
| Sarimo et al. (23) | 2002 | American journal of sports medicine | III | 42 | Arthroscopy: 19; Open: 16 | 35 | 35 | 33 | 33 [16–83] | 33 [6–120] | Categorical | 1 | – |
| El-Assal et al. (24) | 2003 | KSSTA | IV | 29 | Arthroscopy: 22; Open: 5 | 26 | 27 | 27 | 29 [12–40] | 58 [9–110] | Categorical | 4 | 1 revision arthroscopic excision and debridement of cyst due to incomplete removal |
| Hulet et al. (25) | 2004 | Arthroscopy | IV | 40 | Arthroscopy | 103 | 105 | 105 | 33 [12–69] | 60 [12–144] | Categorical | 7 | 1 septic arthritis; 1 recurrent hydrarthrosis; 1 reflex dystrophy |
| Howe and Koh (6) | 2007 | The Knee | IV | 32 | Arthroscopy | 8 | 8 | 6 | 37.2 [18–49] | 39.1 [12-94] | Lysholm and Tegner | 0 | – |
| Pujol et al. (26) | 2013 | KSSTA | IV | 27 | Open | 19 | 15 | 21 | 25 [16–44]* | 40 [24–101]* | KOOS 86.1; IKDC 84.0 | 0 | 4 secondary meniscectomies for recurrence of symptoms |
| Kumar et al. (27) | 2014 | The Knee | IV | 39 | Arthroscopy | 14 | 14 | 14 | 40 [21–56] | 61.2 [38–94] | Lysholm | 0 | – |
| Haklar et al. (22) | 2014 | The Knee | IV | 52 | Arthroscopy | 20 | 20 | – | 41 [17–68] | 37.5 [12–70] | Lysholm and modified Dorfmann clinical outcome scale | 0 | – |
| Chang et al. (28) | 2015 | KSSTA | III | 58 | Arthroscopy | 241 | 241 | 241 | 36.8 | 26 [7–36] | Lysholm and VAS | 32 | – |
| Bombaci, et al. (29) | 2016 | SICOT-J | IV | 46 | Arthroscopy | 8 | 8 | 7 | 36.13 [19–63] | 27.3 [12–47] | Lysholm and VAS | 2 | – |
| Iorio et al. (30) | 2020 | International orthopaedics | IV | 53 | Arthroscopy | 18 | 18 | 21 | 40 [15–60] | 139.2 [84–180] | Lysholm, IKDC and Tegner | 0 | – |
| Orsini et al. (31) | 2020 | International Orthopaedics | IV | 44 | Open | 13 | 13 | 13 | 33 [18–56] | 32 [24–27] | Lysholm and VAS | 0 | – |
*, median value. CMS, Coleman methodology score; IKDC score, International Knee Documentation Committee score; KOOS, The Knee injury and Osteoarthritis Outcome Score; KSSTA, Knee Surgery, Sports Traumatology, Arthroscopy; SICOT-J, journal of the Société Internationale de Chirurgie Orthopédique et de Traumatologie; VAS, visual analogue scale.
Table 2
| Author | Year | Method | Gender | Number of meniscus tears | Meniscal tear patterns | Treatment of meniscal tear | Number of meniscal cysts | Distribution of meniscal cysts | Treatment of meniscal cyst |
|---|---|---|---|---|---|---|---|---|---|
| Tudisco et al. (21) | 2000 | Arthroscopy | Males: 10; Females: 9 | – | Horizontal or radial lesion (or both) | Arthroscopic partial meniscectomy | 19 | 19 lateral | Arthroscopic decompression |
| Sarimo et al. (23) | 2002 | Arthroscopy: 19; Open: 16 | Males: 23; Females: 12 | 33 | Radial: 8; Flap: 7; Complex: 11; Bucket handle: 5; Meniscocapsular tears: 2 | Arthroscopic partial meniscectomy | 35 | 17 lateral; 18 medial | Arthroscopic decompression: 19; Open cystectomy: 16 |
| El-Assal et al. (24) | 2003 | Arthroscopy: 22; Open: 5 | Males: 21; Females: 5 | 27 | Horizontal: 12; Complex with peripheral horizontal component: 8; Transverse: 7 | Arthroscopic partial meniscectomy: 24; Open repair: 3 | 27 | 27 lateral | Arthroscopic decompression: 22; Open cystectomy: 5 |
| Hulet et al. (25) | 2004 | Arthroscopy | Males: 80; Females: 23 | 105 | Horizontal: 30; Horizontal with radial split: 30; Radial: 31; Complex: 10; Vertical: 4 | Arthroscopic partial meniscectomy: 104; Repair: 1 | 105 | 105 lateral | Arthroscopic decompression: 91; Additional percutaneous drainage: 14 |
| Howe and Koh (6) | 2007 | Arthroscopy | Males: 4; Females: 4 | 6 | – | Arthroscopic partial meniscectomy: 4; Left alone: 2 | 8 | 6 lateral; 2 medial | Arthroscopic decompression |
| Pujol et al. (26) | 2013 | Open | Males: 13; Females: 6 | 21 | Horizontal: 21 | Arthroscopic partial meniscectomy: 5; Open repair with vertical sutures: 16 | 15 | 6 lateral; 9 medial | Open cystectomy |
| Kumar et al. (27) | 2013 | Arthroscopy | Males: 7; Females: 7 | 14 | Horizontal: 8; Complex with horizontal component: 6 | Arthroscopic partial meniscectomy | 14 | 8 lateral; 6 medial | Arthroscopic partial meniscectomy without cyst decompression |
| Haklar et al. (22) | 2014 | Arthroscopy | Males: 13; Female: 7 | – | – | Arthroscopic partial meniscectomy | 20 | 20 lateral | Arthroscopic decompression |
| Chang et al. (28) | 2015 | Arthroscopy | Males: 135; Females: 106 | 241 | Horizontal: 167; Complex: 51; Vertical: 13; Bucket handle: 7; Radial: 3 | Arthroscopic repair (inside out): 14; Arthroscopic partial meniscectomy: 227 | 241 | 136 lateral; 105 medial | Arthroscopic treatment of meniscal lesion with open cystectomy: 112 (6 repair); Arthroscopic decompression: 129 (8 repair) |
| Bombaci et al. (29) | 2016 | Arthroscopy | Males: 6; Females: 2 | 7 | Horizontal: 7 | Arthroscopic partial meniscectomy: 7 | 8 | 7 lateral; 1 medial | Mini-open decompression: 1; Arthroscopic decompression: 7 (3 with extra-articular portal) |
| Iorio et al. (30) | 2020 | Arthroscopy | Males: 13; Females: 5 | 21 | Horizontal: 13; Radial: 2; Complex: 4; Discoid associated: 2 | Arthroscopic partial meniscectomy | 18 | 18 lateral | Percutaneous decompression with needle: 18 |
| Orsini et al. (31) | 2020 | Open | Males: 9; Females: 4 | 13 | Horizontal: 13 | Open repair: 13 | 13 | 9 lateral; 4 medial | Open cystectomy |
Despite variations in techniques as described by the different authors in the studies above, it can be broadly classified into open or arthroscopic/percutaneous decompression of the meniscal cyst (cyst decompression) versus open cystectomy. This is matched against the management of the meniscus tear i.e., meniscus repair versus partial meniscectomy/meniscal debridement and is represented in Table 3.
Table 3
| Different combinations of meniscal cyst and tear management | Partial meniscectomy/meniscal debridement | Meniscal repair |
|---|---|---|
| Cystectomy | Chang et al. (28); Pujol et al. (26); Sarimo et al. (23) | Orsini et al. (31); Chang et al. (28); Pujol et al. (26); El-Assal et al. (24) |
| Cyst Decompression | Iorio et al. (30); Bombaci et al. (29); Chang et al. (28); Haklar et al. (22); Howe et al. (6); Tudisco et al. (21); Sarimo et al. (23); El-Assal et al. (24) | Chang et al. (28); Hulet et al. (23) |
A total of 523 cases of meniscal cysts were included in this systematic review, amongst 524 patients. Three hundred seventy-eight cysts (72.28%) involved the lateral and 145 cysts (27.72%) involved the medial meniscus.
One hundred and seventy-six patients underwent open cystectomy, 14 patients underwent arthroscopic partial meniscectomy alone without any cyst manipulation, 18 had percutaneous decompression of the cyst and 315 underwent arthroscopic decompression of the meniscal cyst.
While some studies did not mention the prevalence and/or types of meniscal tears in their patient population, there were at least 488 meniscal tears recorded, with the following broadly classified proportion of the different meniscal tear patterns: 90 complex tears, 301 horizontal tears, 44 radial tears, 7 transverse tears, 17 vertical tears, 7 flap tears, 2 discoid associated, 2 meniscocapsular tears and 12 bucket handle tears. Of the meniscal tears, 2 were left alone, 439 arthroscopic partial meniscectomies or debridement were performed, 1 repair (not specified if open or arthroscopic method used), and 14 arthroscopic repairs and 32 open repairs were done. This data is represented in Table 4 and Table 5 below.
Table 4
| Meniscal tear patterns | Number (%) |
|---|---|
| Complex | 90 (18.4) |
| Horizontal | 301 (61.7) |
| Radial | 44 (9.0) |
| Transverse | 7 (1.4) |
| Vertical | 17 (3.5) |
| Flap | 7 (1.4) |
| Discoid associated | 2 (0.4) |
| Bucket handle | 12 (2.5) |
| Meniscocapsular | 2 (0.4) |
| Not described | 6 (1.2) |
Table 5
| Treatment of meniscal tears | Number (%) |
|---|---|
| Arthroscopic partial meniscectomy/debridement | 439 (90.0) |
| Repairs, total | 47 (9.6) |
| Arthroscopic repair | 14 (2.9) |
| Open repairs | 32 (6.7) |
| Unclear method | 1 (0.2) |
| Left alone | 2 (0.4) |
Complications
Hulet et al. (25) reported 3 post-operative complications: 1 patient who developed knee septic arthritis, 1 patient who developed reflex sympathetic dystrophy, and 1 patient with recurrent effusions. No major complications were reported from the other 11 remaining studies.
Outcomes of interest
The outcomes of interest in this paper are measured via the following means: (I) Recurrences of meniscal cysts looking at—(i) treatment of meniscal cyst; (ii) treatment of meniscal tear and (II) Outcome scores: categorical or Lysholm score.
Recurrences
Treatment of meniscal cyst
Forty-six meniscal cysts recurred (8.63%), with at least 34 recurrences after decompression (10.2%) and 6 recurrences (3.41%) after open cystectomy. This is illustrated in Table 6 below. However, both Bombaci et al. (29) and El-Assal et al. (24) did not report recurrences separately in the groups of patients who underwent different index surgeries, whether it was via the arthroscopic decompression, using the extra-articular portal, or open cystectomy. This brings about ambiguity to the recurrence rates for either surgical technique in their cohort, and their recurrence rates were included in the total numbers but excluded from the treatment specific results.
Table 6
| Meniscal cyst treatment | Total number | Recurrence after treatment |
|---|---|---|
| Decompression | 333 (18 percutaneous decompression, 315 arthroscopic decompression) | 34 (10.21%) |
| Cystectomy | 176 | 6 (3.41%) |
Four cysts recurred following arthroscopic decompression in the study by El-Assal et al. (24), while 1 cyst recurred following open cystectomy in the study by Sarimo et al. (23). Chang et al. (28) had 5 out of 112 (4.46%) meniscal cysts that underwent open cystectomy recurred, while 27 out of 129 (20.93%) meniscal cysts that underwent arthroscopic decompression recurred.
Treatment of meniscal tears
There were a total of 47 meniscal repairs across these 12 studies, with 14 all-inside repairs and 32 open repairs. However, in these studies, clinical outcomes, and recurrences of cysts in the patients who underwent meniscal repair were not reported separately to allow for further scrutiny as to whether the management of the meniscal tear had any impact on the recurrence of the meniscal cyst.
Kumar et al. (27) did not report any manipulation of the cyst and yet was able to achieve good pre and post-operative Lysholm scores with partial meniscectomy alone.
Outcome scores
Of all the 12 studies included, there were mainly 2 predominant clinical outcome measures used, the Lysholm score (32) as well as the categorical scale. The Lysholm score is a 100-point patient reported score initially used to assess outcomes after knee ligament surgery, first published in 1982. A higher score is indicative of a better outcome with fewer symptoms or disability.
The categorical scale adopted by most of the papers used excellent/good/fair/poor, with fairly similar clinical endpoints across the board. The “excellent/good/fair/poor” score was adopted from the Raegan scoring system (3) and is defined below:
- Excellent: no pain, no swelling, full range of motion, full return to athletics of choice;
- Good: occasional discomfort, no swelling, full range of motion, return to athletics of choice but not at same level;
- Fair: pain with strenuous activity with or without occasional swelling and return to modified athletics;
- Poor: pain with activities of daily living, locking, painful catching, cessation of athletics/interference with activities of daily living.
To allow for comparison between outcomes, papers that adopted the Lysholm Scoring system will be assessed together, while papers that adopted the “excellent/good/fair/poor” scoring system will be assessed together. The other papers were not considered for outcomes.
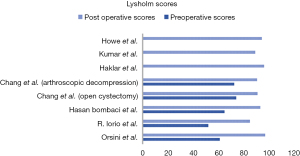
Comparing outcomes with Lysholm score
Seven of the 12 included studies used the Lysholm score to quantify clinical outcomes. These studies and the various scores have been included in Figure 2.
Despite having incomplete data regarding the preoperative Lysholm scores, a good outcome was achieved across these studies, with an average score of 92.1 regardless of surgical method. Post operatively, arthroscopic, mini-open and percutaneous meniscal decompression averaged a Lysholm score of 91.9 as compared to 93.8 in open cystectomy.
When considering the outcome scores in relation to meniscal tear management, only Orsini et al. (31) and Chang et al. (28) performed meniscal repairs. Orsini et al. (31) showed improvement in Lysholm scores with the open meniscal repair method, from 61 to 97. However, Chang et al. (28) did not report results for patients who underwent meniscal repair separately, rendering further analysis impossible. In addition, only 27 of patients underwent meniscal repair while 286 underwent meniscal debridement/partial meniscectomy, with an evidently large disparity in proportion. The average post-operative Lysholm score following meniscal debridement or partial meniscectomy, excluding data from Chang et al. due to lack of separate reporting, is 91.6.
Kumar et al. (27) studied the clinical outcomes in patients with meniscal cysts simply by debriding the concomitant meniscal tear instead of decompressing or excising the meniscal cyst. He reported a mean post-operative Lysholm score of 89.1, which is lower than both the decompression and cystectomy group.
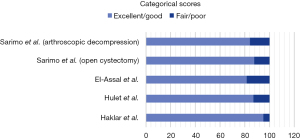
Comparing outcomes with categorical scores
4 studies were included for comparison using the categorical outcome scales, including that of Haklar et al. (22), due to the similarity in the modified Dorfmann clinical outcome score. This data is represented in Figure 3.
Arthroscopic cyst decompression showed an average of 86.9% with excellent/good outcomes, and 13.1% with fair/poor outcomes. The only study with open cystectomy done was that by Sarimo et al. (23), with 87.5% excellent/good and 12.5% fair/poor.
The outcomes from both the Lysholm score and the categorical scale showed significant improvement. In addition, the data from the included studies appear to be encouraging, with good Lysholm scores and at least 80% of patients having excellent/good outcomes with either arthroscopic decompression or open cystectomy.
Only 1 of the 4 studies included meniscal repair, with Hulet et al. (25) reporting 1 case of meniscal repair. There was no separate reporting of the data and more information regarding meniscal treatment outcomes cannot be obtained.
Discussion
In 2016, Chang et al. (28) did a comparison of arthroscopic cyst decompression compared to arthroscopic cyst excision, where it was found that open cystectomy showed significantly better results with lower recurrence risk than arthroscopic decompression. There was an increased risk of cyst recurrence associated with decompression compared with excision for patients with symptomatic meniscal cysts during an average 26-month follow-up period. 20.9% of meniscus cysts (27/129) that were decompressed recurred, only 4% (5/112) of excised meniscus cysts recurred They suggested that cyst volume and meniscal tear circumference were associated with disease recurrence. This opinion is echoed in the study by El-Assal et al. (24) who described 3 of 4 recurrences secondary to a large cyst which could not be properly addressed arthroscopically. Similarly, Bombaci et al. (29) also reported an increased risk of recurrence in the event of a large meniscal cyst.
In our review, decompression of the meniscal cyst appears to have a higher rate of recurrence as compared to cystectomy. However, it may not be completely accurate to simply conclude that open cystectomy is the surgery of choice when it comes to meniscal cyst. This review suggests a relationship between size of meniscal cyst and rate of recurrence, as well as the choice to manage them with decompression or excision. This is prior to taking the meniscus tear management into consideration as well.
Barrie (1) in 1979 postulated that the horizontal meniscal tear was paramount in the development of meniscal cysts, with all 112 surgical specimens demonstrating a horizontal tear in relation with a meniscal cyst. Today, new advancements in horizontal meniscus repair may herald a new option for meniscal cysts, with the aim to preserve meniscus as far as possible. Pujol et al. (26) did not experience any meniscal cyst recurrences when the horizontal meniscal tears were repaired.
In this review, there were 523 meniscal cysts, associated with 488 meniscal tears. Haklar et al. (22) and Tudisco et al. (21) were excluded in the tally for the meniscal tears as they did not record the number of meniscal tears associated with the cysts. Almost all the cysts were noted to be associated with meniscal tears, some cysts even had more than 1 meniscal tear involved, as noted by Pujol et al. (26). The presence of meniscal tear may explain why some meniscal cysts that were decompressed without addressing the meniscus tear might have increased risk of recurrence. Kumar et al. (27) reported medium-term outcomes with post-operative Lysholm score of 89.1, from an initial score of 94.1. This could be attributed to perhaps the lack of meniscal cyst management and degenerative changes following meniscal debridement/meniscectomy.
Cowden et al. (9) proposed an algorithm suggesting for meniscectomy and cystectomy in symptomatic patients with meniscal cysts and meniscal tears not amenable to repair.
Similarly, Pedowitz et al. (33) previously recommended partial meniscectomy for meniscal tears associated with meniscal cysts in a surgical algorithm for treatment of meniscal cysts and associated meniscal tears. The recognition of the importance of treating horizontal meniscus tears and avoiding resection of either leaves of the horizontal tear given that the loss of meniscus leads to degenerative changes; has seen the increased repairs of such tears.
With further improvement in meniscal repair techniques, further consideration should be given to meniscal repairs in the presence of meniscal cysts. Hence these algorithms require thought now as the indications for meniscal repairs have been pushed further to include horizontal meniscus tears. Other parameters including size of meniscal cyst should also be taken into consideration when dealing with a meniscal tear with a concomitant cyst.
Due to the lack of separately reported outcomes and recurrences in the patients who underwent meniscal repair, open or arthroscopic, it is difficult to determine if the meniscal repair could have also contributed to improved outcomes or the recurrences of meniscal cyst treatment with our review cohort.
Limitations
This systematic review of the literature presents several limitations. The overall retrospective nature of the included papers means that most of the studies were non-randomised clinical trials, thus predisposing to allocation bias. The lack of high-quality level I or II studies prevents a surgical recommendation to be made in the algorithm of management of meniscal cysts. While the methods were generally the same throughout all the papers, there are minor technique variations evidenced. The papers also had different markers of clinical success—some used the Lysholm scoring system, while others used the “excellent/good/fair/poor” system which then made it difficult to accurately assess the level of improvement for all the patients involved. Further studies should improve these limitations, providing prospective analyses involving more patients, using common yardsticks of measures of success or common scoring systems, including general health measures as well. Recurrence of cysts should also be stated clearly, especially if there are none involved.
The points of strength of this paper included comprehensive nature of the literature search, the strict eligibility criteria and adequate follow up duration.
Conclusions
According to the main findings of this systemic review, both arthroscopic and open methods can be used for meniscal cysts treatment. Open cystectomy, rather than decompression of the meniscal cyst appear to confer lower recurrence rates, with reasonable clinical outcomes. However, a recommendation for surgical repair of meniscus tears associated with meniscus cysts cannot be made at this time due to insufficient high-quality level I or II trials and separate outcome reporting. Previously proposed algorithms may require reconsideration as the boundaries of meniscal tear repairs are pushed further today.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-29/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-29/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barrie HJ. The pathogenesis and significance of menisceal cysts. J Bone Joint Surg Br 1979;61-B:184-9. [Crossref] [PubMed]
- Wroblewski BM. Trauma and the cystic meniscus: review of 500 cases. Injury 1973;4:319-21. [Crossref] [PubMed]
- Reagan WD, McConkey JP, Loomer RL, et al. Cysts of the lateral meniscus: arthroscopy versus arthroscopy plus open cystectomy. Arthroscopy 1989;5:274-81. [Crossref] [PubMed]
- Seger BM, Woods GW. Arthroscopic management of lateral meniscal cysts. Am J Sports Med 1986;14:105-8. [Crossref] [PubMed]
- Lonner JH, Parisien JS. Arthroscopic treatment of meniscal cysts. Oper Tech Orthop 1995;5:72-7.
- Howe TS, Koh JS. Arthroscopic internal marsupialization of meniscal cysts. Knee 2007;14:408-10. [Crossref] [PubMed]
- Kurzweil P, Krych AJ, Anz A, et al. Favorable Reoperation Rate at 2 Years Following Repair of Horizontal Cleavage Tears Using an All Suture-Based Technique: A Prospective, Multicenter Trial. Arthrosc Sports Med Rehabil 2021;3:e773-e780. [Crossref] [PubMed]
- Morris JH, Magnussen RA, DiBartola AC, et al. Patient Outcomes After Horizontal Cleavage Tear Repair: A Systematic Review. Arthroscopy 2020;36:2316-31. [Crossref] [PubMed]
- Cowden CH 3rd, Barber FA. Meniscal cysts: treatment options and algorithm. J Knee Surg 2014;27:105-11. [Crossref] [PubMed]
- Campbell SE, Sanders TG, Morrison WB. MR imaging of meniscal cysts: incidence, location, and clinical significance. AJR Am J Roentgenol 2001;177:409-13. [Crossref] [PubMed]
- De Smet AA, Graf BK, del Rio AM. Association of parameniscal cysts with underlying meniscal tears as identified on MRI and arthroscopy. AJR Am J Roentgenol 2011;196:W180-6. [Crossref] [PubMed]
- BONNIN JG. Cysts of the semilunar cartilages of the knee-joint. Br J Surg 1953;40:558-65. [Crossref] [PubMed]
- Flynn M, Kelly JP. Local excision of cyst of lateral meniscus of knee without recurrence. J Bone Joint Surg Br 1976;58:88-9. [Crossref] [PubMed]
- Lu KH. Arthroscopic meniscal repair and needle aspiration for meniscal tear with meniscal cyst. Arthroscopy 2006;22:1367.e1-4. [Crossref] [PubMed]
- Passler JM, Hofer HP, Peicha G, et al. Arthroscopic treatment of meniscal cysts. J Bone Joint Surg Br 1993;75:303-4. [Crossref] [PubMed]
- Parisien JS. Arthroscopic treatment of cysts of the menisci. A preliminary report. Clin Orthop Relat Res 1990;154-8.
- Glasgow MM, Allen PW, Blakeway C. Arthroscopic treatment of cysts of the lateral meniscus. J Bone Joint Surg Br 1993;75:299-302. [Crossref] [PubMed]
- Haratian A, Bolia IK, Hasan LK, et al. Arthroscopic Management of Meniscal Cysts: A Systematic Review. Orthop Res Rev 2021;13:123-39. [Crossref] [PubMed]
- Wright JG, Einhorn TA, Heckman JD. Grades of recommendation. J Bone Joint Surg Am 2005;87:1909-10. [Crossref] [PubMed]
- Coleman BD, Khan KM, Maffulli N, et al. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 2000;10:2-11. [Crossref] [PubMed]
- Tudisco C, Meo A, Blasucci C, et al. Arthroscopic treatment of lateral meniscal cysts using an outside-in technique. Am J Sports Med 2000;28:683-6. [Crossref] [PubMed]
- Haklar U, Ayhan E, Ustundag S, et al. A new arthroscopic technique for lateral parameniscal cyst decompression. Knee 2014;21:126-8. [Crossref] [PubMed]
- Sarimo J, Rainio P, Rantanen J, et al. Comparison of two procedures for meniscal cysts. A report of 35 patients with a mean follow-up of 33 months. Am J Sports Med 2002;30:704-7. [Crossref] [PubMed]
- El-Assal M, Mostafa M, Abdel-Aal A, et al. Arthroscopy alone or in association with open cystectomy: in treatment of lateral meniscal cysts. Knee Surg Sports Traumatol Arthrosc 2003;11:30-2. [Crossref] [PubMed]
- Hulet C, Souquet D, Alexandre P, et al. Arthroscopic treatment of 105 lateral meniscal cysts with 5-year average follow-up. Arthroscopy 2004;20:831-6. [Crossref] [PubMed]
- Pujol N, Bohu Y, Boisrenoult P, et al. Clinical outcomes of open meniscal repair of horizontal meniscal tears in young patients. Knee Surg Sports Traumatol Arthrosc 2013;21:1530-3. [Crossref] [PubMed]
- Kumar NS, Jakoi AM, Swanson CE, et al. Is formal decompression necessary for parameniscal cysts associated with meniscal tears? Knee 2014;21:501-3. [Crossref] [PubMed]
- Chang JJ, Li YH, Lin GM, et al. Comparison of the recurrence risk of parameniscal cysts between patients treated with arthroscopic excision and arthroscopic decompression techniques. Knee Surg Sports Traumatol Arthrosc 2016;24:1547-54. [Crossref] [PubMed]
- Bombaci H, Kuyumcu M, Coskun T, et al. When should the external approach be resorted to in the arthroscopic treatment of perimeniscal cyst? SICOT J 2016;2:19. [Crossref] [PubMed]
- Iorio R, Mazza D, Drogo P, et al. Lateral meniscal cysts: long-term clinical and radiological results of a partial meniscectomy and percutaneous decompressive needling. Int Orthop 2020;44:487-93. [Crossref] [PubMed]
- Orsini NG, Favreau H, Eichler D, et al. Meniscus sutures by arthrotomy for a non-transfixing horizontal lesion associated with a cyst. Int Orthop 2020;44:1071-6. [Crossref] [PubMed]
- Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 1982;10:150-4. [Crossref] [PubMed]
- Pedowitz RA, Feagin JA, Rajagopalan S. A surgical algorithm for treatment of cystic degeneration of the Meniscus. Arthroscopy 1996;12:209-12; discussion, 213-6. [Crossref] [PubMed]
Cite this article as: Thor JEH, Lim GYC, Hui JHP, Lee DYH. Do meniscal repairs with meniscus cyst do better than meniscectomy?—a systematic review of meniscal cyst treatment. Ann Joint 2023;8:8.