
Simultaneous medial unicompartmental knee replacement and anterior cruciate ligament reconstruction: a narrative review and technical note
Introduction
Unicompartmental knee arthroplasty (UKA) is a well-established surgical option in the treatment of compartmental osteoarthritis (OA) in young patients. In the last years UKA has gained interest given its potential benefits with respect to the total knee arthroplasty (TKA). Among these advantages are that it is a less invasive procedure, it has a faster recovery, it provides better knee kinematics, and it preserves a greater bone stock (1). One of the main disadvantages is that it has a higher number of revisions compared to the TKA (2,3). However, this is controversial and recent literature has shown that in high-volume surgeons revision rates would be similar between the two procedures (4).
As UKA is indicated in young, active patients with high functional demand, the biomechanical interaction and biological integration of these implants with the rest of the intra- and extra-articular structures of the knee has been raised as a problem (5,6). This article describes (I) how the function and survival of UKA can be affected by knee ligament insufficiency; (II) how the simultaneous anterior cruciate ligament (ACL) reconstruction is able to restore biomechanics necessary for the success of the arthroplasty; and (III) the surgical technique of UKA and ACL reconstruction. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-7/rc).
Methods
A literature search was performed on PubMed, including articles written in English until June 2021 (Table 1). The articles regarding ACL reconstruction and UKA were reviewed using the narrative approach.
Table 1
| Items | Specification |
|---|---|
| Date of search | July 1st, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | “Anterior Cruciate Ligament Reconstruction”, “Unicompartmental Knee Replacement” |
| Timeframe | From origin until July 1st, 2022 |
| Inclusion and exclusion criteria | Inclusion criteria: (I) original articles about ACL reconstruction and UKA; (II) written in English; (III) involving three or more cases |
| Exclusion criteria: (I) posters or abstracts at annual meetings or masters’ theses without subsequent peer-reviewed publication of an article; (II) articles not written in English; (III) case reports or studies reporting less than 3 cases | |
| Selection process | Two non-blinded authors reviewed the titles and abstracts of each article identified in the literature search. If a study met all the criteria or the abstract did not provide enough information to include or exclude the report, full texts were obtained, reviewed and considered for data extraction. Whenever an agreement about study inclusion could not be resolved by consensus between the two reviewers, a third author decided about the inclusion |
ACL, anterior cruciate ligament; UKA, unicompartmental knee arthroplasty.
Results
ACL role in the kinematics of UKA
As simplified in the well-known four-bar model (7), the main function of the ACL is to prevent the anterior subluxation of the tibia with respect to the femur at all degrees of flexion (8), this model foresees that the ACL maintain a constant length from full extension to full flexion, stabilizing the sliding-rolling of the femur on the tibia in a fixed trajectory; the ACL fibers are in fact arranged in such a way to remain in tension throughout the entire range of movement of the knee (9,10). In the literature it is shown that the ACL insufficiency predisposes to further intra-articular injuries and to an accelerated arthritic degeneration in the native knee (11,12), moreover some authors have shown how the kinematic behavior of the prosthetic components of the UKA is altered in the unstable ACL knee (13,14). In their cadaveric study, Suggs et al. demonstrated that an ACL-deficient knee after UKA presents more anterior tibial translation compared to native knee and to knee after UKA with an intact ACL (13). The same group then analyzed the relative positions of the intra-articular pressure points by simulating the physiological muscle loads and showed how these points were moving posteriorly on the tibial component in the knee after transection of the ACL in UKA, suggesting a possible factor of wear and early failure (15). Furthermore, Citak et al. demonstrated that the ACL reconstruction in the knee with UKA was able to normalize both the Lachman and the pivot-shift tests (16), while Pandit et al. demonstrated in vivo that the ACL reconstruction associated with the medial UKA was able to restore kinematics comparable to those of a UKA with intact ACL or a native knee (17). These studies therefore show how a knee without ACL is not an optimal environment to the correct functioning of UKA. However, recent studies have shown that there are no differences in functional outcomes and survival rate between patients undergoing UKA with ACL-intact or ACL-deficient knees (18).
Indications
Although biomechanical studies suggest that ligamentous instability could represent a contraindication to perform UKA, there is no clear consensus on the subject (13,18). From the first clinical reports it was clear that the UKA in unstable joints had unacceptable failure rates (19,20). However, subsequent studies have shown that some patients with injured ACL, but without subjective symptoms of instability, obtain similar results to patients with intact ACL, suggesting that the overall joint laxity has a greater weight than the only integrity of the ACL in the clinical outcome of the implants (14). Other factors such as the tension of the collateral ligaments and the posterior capsule, muscular state or the presence of intra-articular osteophytes can have a role, even if secondary, in joint stability (21-25). The classic indications for medial UKA are unicompartmental degenerative disease with impaired joint status in the other compartments, a stable knee, correctable (intraarticular) varus deformity, with fixed flexion deformity less than 10–15 degrees, and flexion greater than 100 degrees (14). Based on the experience of the authors and the published literature, in the context of medial compartment OA and ACL deficiency, it is possible to opt for a UKA without the need for ligament reconstruction in those patients without functional instability in their activities or in those with a more advanced biological age and/or low functional demand. On the other hand, if there is functional instability in young and active patients, ACL reconstruction is considered in conjunction with UKA.
Original surgical technique
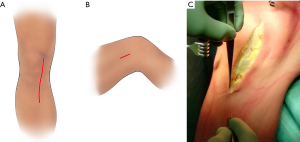
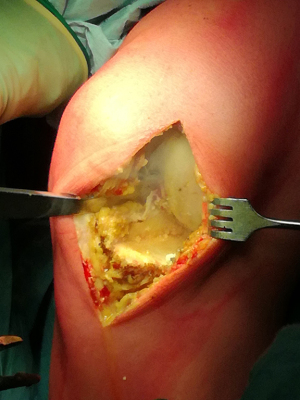
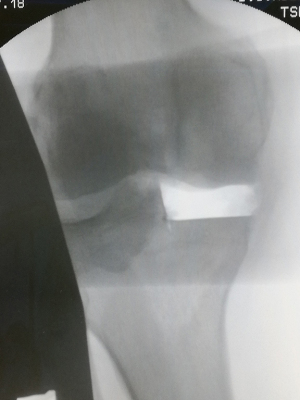
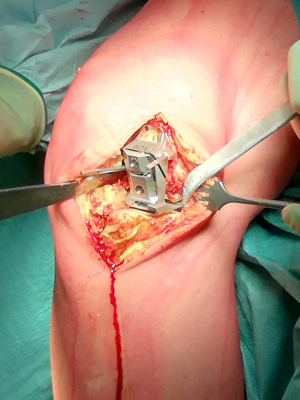
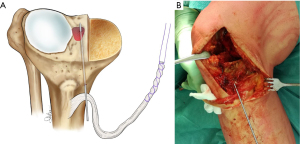
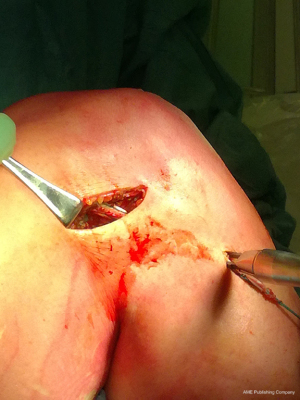
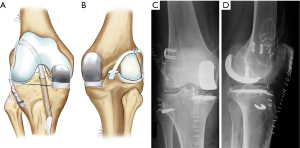
Our preferred surgical technique consists in arthroscopic ACL reconstruction technique described by Marcacci et al. (26) associated with a UKA (De Puy, Preservation Uni with all-poly tibial component), according to a minimally invasive technique that minimizes postoperative complications and improves recovery (27,28). The patient is placed on supine position; the limb is left free in order to perform intraoperative mobilization. A first arthroscopic stage is performed to verify the state of the tibial and femoral cartilage and ACL. Then, with the knee flexed at 90°, an incision of about 10 cm is performed on the skin (Figure 1), whose upper limit is represented by the upper pole of the patella, while the lower is related to the semitendinosus and gracilis tendons (STG) which are harvested leaving intact their insertion on the tibia (thus preserving vascularity and innervation) (29). Then a medial parapatellar incision is performed with a partial excision of the Hoffa fat pad and removal of the osteophytes; after that, assessment of the posterior slope with an oscillating saw blade or a thin chisel resting on the medial plate with a 110° flexion knee is carried out. The tibial cut is performed freehand and with fluoroscopic assistance based on predefined anatomical landmarks (Figure 2): (I) the horizontal cut is made at the insertion line of the synovial membrane to the bone; (II) the vertical cut is made medial to the tibial spine and parallel to the epiphyseal axis (i.e., a line that joins perpendicularly the metaphyseal cartilage residue and the midpoint of the tibial plateau). This ensures a restoration of the axis alignment and avoids overcorrection, which would cause an overload of the lateral compartment (30,31). At this point the resection is checked by fluoroscopic assistance, applying a valgus stress (Figure 3). The horizontal cut is considered acceptable if orthogonal to the axis. The anterior limit of the femoral resection is marked using as a reference the most anterior point of the tibial plate with the knee extended; the first cut is parallel to the tibial resection and perpendicular to the leg axis. Provided guides are used to perform other the femoral cuts (Figure 4); it is important to keep the femoral component as medial as possible to avoid conflict with the patella.
At this point a K-wire is inserted medial to the hamstring’s insertion as a guide for the tibial tunnel and passed towards to the tibial footprint of the ACL; it is possible to correct the position of the K-wire if a conflict between the tunnel and the final component is expected (Figure 5). At the last, the final prosthetic components are cemented and then the tibial tunnel is drilled onto the previously inserted guidewire. With the knee flexed at 90° an incision of about 4 cm is made on the lateral epicondyle, the iliotibial band is incised in its posterior third and with the electrocautery an operculum is made in the intermuscular septum; at this point the capsule is reached with the finger palpating the posterior profile of the condyle. A curved Kelly clamp is passed from the anteromedial portal into the notch, and its tip is placed against the posterior part of the capsule as far proximal as possible. Once the tip of the clamp can be palpated from the lateral side of the femur, just posterior to the intermuscular septum, it is pushed through the thin posterior layer of the knee capsule to reach the posterior space previously prepared. A suture loop is placed into the tip of the clamp, which is then pulled anteriorly through the anteromedial portal and put into the wire loop previously inserted in the portal. Pulling the wire loop from the tibial side, the suture enters the tibial tunnel and exits from the tibial incision, ready to pull the harvested graft. The stitches on the free end of the STG grafts are tied onto the passing suture that is pulled through the knee joint and placed in the “over-the-top” position behind the lateral condyle where it is fixed with two metallic staples, keeping the knee at 70° of flexion and the lower leg at 15° of external rotation. Finally, with the residual graft, a lateral tenodesis is carried out which allows a better control of the rotational instability (32), assing the graft under the iliotibial band and fixing it on the Gerdy tubercle with a metallic staple (Figure 6). Postoperative X-ray control is performed (Figure 7) in order to check tibial tunnel and prosthesis components positioning. The rehabilitation protocol consists of an early active and passive mobilization of the knee with the aim of reaching 90° of flexion after 2–3 days; isometric contractions are encouraged from the first day. Partial weight-bearing without brace is allowed from the first postoperative day and increased full weight-bearing by the 4th week. Differently, when UKA is performed alone, full weight bearing is encouraged form the 1st week.
As regards sport resumption, cycling and swimming are allowed from the 3rd week postoperatively, while running in straight line is allowed from the 12th week. Pivoting sports are allowed not before 6 to 8 months postoperatively.
Discussion
The UKA and ACL reconstruction are considered consolidated, safe and step-by-step surgeries; however, performing both procedures in a single time actually poses greater technical difficulties such as:
- Possible impingement between tunnels and prosthetic components;
- Possible weakening of the medial tibial plateau (risk of fracture);
- Inadequate tensioning of the graft;
- Choice of the optimal type of graft;
- Influence of the tibial slope on joint laxity;
- Choice between mobile or fixed plate systems.
Some modifications and adaptations to the techniques are normally required; for example, the tibial cut is performed before perforating the definitive tibial tunnel, which is moved laterally and vertically with respect to the isolated ACL reconstruction to avoid the conflict with the tibial component and reduce the risk of bone weakening. Moreover, it is preferable to tension and definitively fix the graft only after the assembly of the final components of the UKA in order to restore the correct joint space first (33-35). The choice of the graft is another variable to consider. One of the most used is the bone-patellar tendon bone (BPTB) graft: it is possible to harvest from the same approach of the UKA, gives better initial graft integration (bone/bone) and allows to move the tibial tunnel laterally as mentioned above (24). Another valid option described in the literature is the use of the STG auto or allograft (35,36). As known, the AP laxity is influenced by the tibial slope, whereas a posterior tibial slope has been proposed as a potential risk factor for ACL injury (37,38). Indeed, osteotomies techniques that modify the tibial slope are used as treatment in some cases of ACL injuries (39). In the same way it is possible to modify the tibial slope with the cut of the UKA, changing the polyethylene insert or modifying the tibial cut. Suero et al. demonstrated in a cadaveric study that by decreasing the slope of the tibial component by a few degrees a normalization of the tibial anterior translation is obtained during the Lachman test (40). Hernigou and Deschamps showed that a slope greater than 9° is associated with an increased risk of both ACL injury and aseptic loosening (41). In general, modification of the tibial slope is not performed unless there is a significant alteration of it; according to the author’s preferences when the tibial slope is >12° it is recommended to decrease the slope of the tibial component in order to protect the graft from excessive stress. Tibial slope is calculated on lateral knee X-rays, subtracting from 90° the angle between the tibial axis (defined as the line passing through two points which are both equidistant from the anterior and posterior tibial cortex at 5 and 15 cm respectively distal from the tibial plateau) and the tangent to the anterior and posterior edges of the medial tibial plateau.
Finally, the choice of a mobile or fixed plate depends on the preference of the surgeon; theoretically, fixed plate designs appear to be less concave and allow a greater slippage of the condyle (an amplified effect in an unstable knee) that could lead to premature wear compared to the mobile plate, as demonstrated by Blunn et al. (42). However, it is clear from the literature that fixed plate implants have slightly better results in terms of survival and revision, although based on follow-up too short to accept definitive conclusions (14). In terms of outcomes, excellent results of the association of the two procedures have been described (33-36,43-45). Weston-Simons et al. (43) reported a survival rate of 93% at 5 years of average follow-up while Tinius et al. (34) reported in 27 patients with an average follow-up of 53 months a statistically significant improvement in the Knee Society Score and no revision surgeries or signs of loosening. In 2016, Mancuso et al. (46) published a systematic review involving 106 patients with UKA and ACL reconstruction. They reported a survival rate of 97% at 47 months mean follow-up, compared to a survival rate of 88% in a group of 154 patients with UKA and ACL deficiency at 77 months mean follow-up. Recently, Volpin et al. (47) performed another systematic review of the literature which included 186 patients who were treated with UKA and ACL reconstruction. The average follow-up was 37.6 months, and they reported an improvement in the Oxford score from 27.5 to 36.8. Among the reported complications were the tibial inlay dislocation (n=3), TKA conversion (n=1), infection with revision in two stage (n=2), deep vein thrombosis (n=1), rigidity requiring manipulation under anesthesia (n=1) and retro patellar pain requiring arthroscopic adhesiolysis (n=1).
Finally, there is not much evidence regarding the advantages and disadvantages of performing ACL reconstruction simultaneously with UKA or in stages. Weston and Simons published a series in which they demonstrated good functional results both in patients in whom the procedures were performed in a stage and in those in whom it was performed in two stages (43).
Conclusions
Although there is no unanimous opinion about performing the UKA together with an ACL reconstruction, both biomechanical and clinical studies show that the benefits of restoring good joint stability outweigh the possible risks associated with performing both surgeries at the same time (16,34-36,43,45,47). With this strategy, after an adequate patient selection and correct surgical technique, it is possible to obtain good clinical results with a high survival rate of the implant and patient satisfaction.
Acknowledgments
The authors would like to express special thanks to Ms. Silvia Bassini for the pictures and graphic support.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-7/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-22-7/coif). SZ serves as an unpaid editorial board member of Annals of Joint from March 2021 to February 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Murray DW, Parkinson RW. Usage of unicompartmental knee arthroplasty. Bone Joint J 2018;100-B:432-5. [Crossref] [PubMed]
- Liddle AD, Pandit H, Judge A, et al. Optimal usage of unicompartmental knee arthroplasty: a study of 41,986 cases from the National Joint Registry for England and Wales. Bone Joint J 2015;97-B:1506-11. [Crossref] [PubMed]
- Tay ML, Young SW, Frampton CM, et al. The lifetime revision risk of unicompartmental knee arthroplasty. Bone Joint J 2022;104-B:672-9. [Crossref] [PubMed]
- Mohammad HR, Judge A, Murray DW. A matched comparison of cementless unicompartmental and total knee replacement outcomes based on the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. Acta Orthop 2022;93:478-87. [Crossref] [PubMed]
- Janssen SJ, van Oost I, Breugem SJM, et al. A structured evaluation of the symptomatic medial Oxford unicompartmental knee arthroplasty (UKA). EFORT Open Rev 2021;6:850-60. [Crossref] [PubMed]
- Johal S, Nakano N, Baxter M, et al. Unicompartmental Knee Arthroplasty: The Past, Current Controversies, and Future Perspectives. J Knee Surg 2018;31:992-8. [Crossref] [PubMed]
- O'Connor JJ, Shercliff TL, Biden E, et al. The geometry of the knee in the sagittal plane. Proc Inst Mech Eng H 1989;203:223-33. [Crossref] [PubMed]
- Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am 1980;62:259-70.
- Strocchi R, de Pasquale V, Gubellini P, et al. The human anterior cruciate ligament: histological and ultrastructural observations. J Anat 1992;180:515-9.
- Duthon VB, Barea C, Abrassart S, et al. Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2006;14:204-13. [Crossref] [PubMed]
- Murrell GA, Maddali S, Horovitz L, et al. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med 2001;29:9-14. [Crossref] [PubMed]
- Indelicato PA, Bittar ES. A perspective of lesions associated with ACL insufficiency of the knee. A review of 100 cases. Clin Orthop Relat Res 1985;77-80.
- Suggs JF, Li G, Park SE, et al. Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study. J Arthroplasty 2004;19:224-9. [Crossref] [PubMed]
- Mancuso F, Dodd CA, Murray DW, et al. Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthop Traumatol 2016;17:267-75. [Crossref] [PubMed]
- Suggs JF, Li G, Park SE, et al. Knee biomechanics after UKA and its relation to the ACL--a robotic investigation. J Orthop Res 2006;24:588-94. [Crossref] [PubMed]
- Citak M, Bosscher MR, Citak M, et al. Anterior cruciate ligament reconstruction after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2011;19:1683-8. [Crossref] [PubMed]
- Pandit H, Van Duren BH, Gallagher JA, et al. Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty: in vivo kinematics. Knee 2008;15:101-6. [Crossref] [PubMed]
- Plancher KD, Brite JE, Briggs KK, et al. Patient-acceptable symptom state for reporting outcomes following unicompartmental knee arthroplasty: a matched pair analysis comparing UKA in ACL-deficient versus ACL-intact knees. Bone Joint J 2021;103-B:1367-72. [Crossref] [PubMed]
- Deschamps G, Lapeyre B. Rupture of the anterior cruciate ligament: a frequently unrecognized cause of failure of unicompartmental knee prostheses. Apropos of a series of 79 Lotus prostheses with a follow-up of more than 5 years. Rev Chir Orthop Reparatrice Appar Mot 1987;73:544-51.
- Goodfellow JW, Kershaw CJ, Benson MK, et al. The Oxford Knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg Br 1988;70:692-701. [Crossref] [PubMed]
- Christensen NO. Unicompartmental prosthesis for gonarthrosis. A nine-year series of 575 knees from a Swedish hospital. Clin Orthop Relat Res 1991;165-9.
- Engh GA, Ammeen DJ. Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat Res 2014;472:73-7. [Crossref] [PubMed]
- Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty 1996;11:782-8. [Crossref] [PubMed]
- Plancher KD, Dunn AS, Petterson SC. The anterior cruciate ligament-deficient knee and unicompartmental arthritis. Clin Sports Med 2014;33:43-55. [Crossref] [PubMed]
- Boissonneault A, Pandit H, Pegg E, et al. No difference in survivorship after unicompartmental knee arthroplasty with or without an intact anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2013;21:2480-6. [Crossref] [PubMed]
- Marcacci M, Zaffagnini S, Iacono F, et al. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc 1998;6:68-75. [Crossref] [PubMed]
- Bruni D, Iacono F, Russo A, et al. Minimally invasive unicompartmental knee replacement: retrospective clinical and radiographic evaluation of 83 patients. Knee Surg Sports Traumatol Arthrosc 2010;18:710-7. [Crossref] [PubMed]
- Argenson JN, Parratte S, Flecher X, et al. Unicompartmental knee arthroplasty: technique through a mini-incision. Clin Orthop Relat Res 2007;32-6. [Crossref] [PubMed]
- Zaffagnini S, Golanò P, Farinas O, et al. Vascularity and neuroreceptors of the pes anserinus: anatomic study. Clin Anat 2003;16:19-24. [Crossref] [PubMed]
- Bruni D, Iacono F, Raspugli G, et al. Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin Orthop Relat Res 2012;470:1442-51. [Crossref] [PubMed]
- Whiteside LA. Making your next unicompartmental knee arthroplasty last: three keys to success. J Arthroplasty 2005;20:2-3. [Crossref] [PubMed]
- Zaffagnini S, Signorelli C, Lopomo N, et al. Anatomic double-bundle and over-the-top single-bundle with additional extra-articular tenodesis: an in vivo quantitative assessment of knee laxity in two different ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 2012;20:153-9. [Crossref] [PubMed]
- Krishnan SR, Randle R. ACL reconstruction with unicondylar replacement in knee with functional instability and osteoarthritis. J Orthop Surg Res 2009;4:43. [Crossref] [PubMed]
- Tinius M, Hepp P, Becker R. Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2012;20:81-7. [Crossref] [PubMed]
- Ventura A, Legnani C, Terzaghi C, et al. Medial unicondylar knee arthroplasty combined to anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2017;25:675-80. [Crossref] [PubMed]
- Pandit H, Beard DJ, Jenkins C, et al. Combined anterior cruciate reconstruction and Oxford unicompartmental knee arthroplasty. J Bone Joint Surg Br 2006;88:887-92. [Crossref] [PubMed]
- Giffin JR, Stabile KJ, Zantop T, et al. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 2007;35:1443-9. [Crossref] [PubMed]
- Giffin JR, Vogrin TM, Zantop T, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 2004;32:376-82. [Crossref] [PubMed]
- Dejour D, Saffarini M, Demey G, et al. Tibial slope correction combined with second revision ACL produces good knee stability and prevents graft rupture. Knee Surg Sports Traumatol Arthrosc 2015;23:2846-52. [Crossref] [PubMed]
- Suero EM, Citak M, Cross MB, et al. Effects of tibial slope changes in the stability of fixed bearing medial unicompartmental arthroplasty in anterior cruciate ligament deficient knees. Knee 2012;19:365-9. [Crossref] [PubMed]
- Hernigou P, Deschamps G. Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 2004;86:506-11. [Crossref] [PubMed]
- Blunn GW, Walker PS, Joshi A, et al. The dominance of cyclic sliding in producing wear in total knee replacements. Clin Orthop Relat Res 1991;253-60.
- Weston-Simons JS, Pandit H, Jenkins C, et al. Outcome of combined unicompartmental knee replacement and combined or sequential anterior cruciate ligament reconstruction: a study of 52 cases with mean follow-up of five years. J Bone Joint Surg Br 2012;94:1216-20. [Crossref] [PubMed]
- Dervin GF, Conway AF, Thurston P. Combined anterior cruciate ligament reconstruction and unicompartmental knee arthroplasty: surgical technique. Orthopedics 2007;30:39-41.
- Tian S, Wang B, Wang Y, et al. Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction in knees with osteoarthritis and deficient anterior cruciate ligament. BMC Musculoskelet Disord 2016;17:327. [Crossref] [PubMed]
- Mancuso F, Hamilton TW, Kumar V, et al. Clinical outcome after UKA and HTO in ACL deficiency: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:112-22. [Crossref] [PubMed]
- Volpin A, Kini SG, Meuffels DE. Satisfactory outcomes following combined unicompartmental knee replacement and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:2594-601. [Crossref] [PubMed]
Cite this article as: Macchiarola L, Espinosa M, Pirone M, Lucidi GA, Cucurnia I, Grassi A, Marín Fermín T, Zaffagnini S. Simultaneous medial unicompartmental knee replacement and anterior cruciate ligament reconstruction: a narrative review and technical note. Ann Joint 2023;8:6.


