
Current development in surgical techniques, graft selection and additional procedures for anterior cruciate ligament injury: a path towards anatomic restoration and improved clinical outcomes—a narrative review
Introduction
Background
Anterior cruciate ligament (ACL) injuries account for about 50% of knee injuries and are commonly treated with ACL reconstructions (1). Approximately 200,000 people in the United States suffer ACL injuries annually and 120,000 people undergo ACL reconstructions and the incidence of ACL injuries was estimated between 32 and 68.6 per 100,000 (2-5).
ACL reconstruction has long been performed to prevent knee instability and subsequent meniscus damage associated with ACL injury. In the past, ACL reconstruction using transtibial (TT) drilling techniques were widely performed, but this technique failed to create the femoral and tibial tunnel in the exact position (6,7). ACL reconstruction using independent drilling technique has been used to create the tunnel in a more anatomic position, providing greater knee stability and reducing the risk of postoperative osteoarthritis (OA) than the TT technique (8-10). As a further anatomic reconstruction technique, the double-bundle (DB) ACL reconstruction was developed, which showed better knee stability (11). Moreover, surgical techniques for ACL injury are becoming more diverse, including ACL repair (12) and ACL augmentation (13).
Regarding grafts for ACL reconstruction, bone-patella tendon-bone (BTB) autografts were commonly used in ACL reconstruction, but due to concerns about anterior knee pain (14,15), hamstring tendon (HT) autografts are now more commonly used, and quadriceps tendon (QT) autografts are increasingly being used as well (16). In recent years, some institutions have used the peroneus longus tendon (PLT) autografts (17,18), considering the weakness of the muscle strength around the knee and quadriceps-hamstring imbalance (19,20). Allografts and synthetic grafts have also been used as grafts for ACL reconstruction, but the graft failure rate is high and has not improved clinical outcomes (21,22).
Although these various surgical techniques and graft selections are performed, the graft failure rate after ACL reconstruction is as high as 4–17% (23-25), and approximately 20% of patients will develop OA in the long-term follow-up after ACL reconstruction (26).
While lateral extra-articular tenodesis (LET) (27), anterolateral ligament (ALL) reconstruction (ALLR) (28) and anterior closed-wedge high tibial osteotomy (ACW-HTO) (29,30) are now being used as additional procedures in cases of high instability or high posterior tibial slope (PTS) and are expected to improve clinical outcomes (31-33), there is also a need to reconsider current surgical techniques, graft selections and additional procedures in order to improve clinical outcomes and knee stability.
Objective
In this review, we describe the advantages and disadvantages of surgical techniques, graft selections and additional procedures for ACL injury, to summarize current problems, and to improve future surgical techniques. Our hypotheses are that more anatomical reconstructions lead to better clinical outcomes. Grafts are best used with autograft, but the choice of autograft type is a matter of consideration. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-39/rc).
Methods
A PubMed database search was conducted to gather studies on surgical techniques, graft selections, and additional procedures for ACL injury. The selection of articles was based on author-determined credibility, relevancy to the topic, and current trends in managing ACL injury. Specific search terms from Table 1 were utilized, and a summary of the search strategy is provided in Table 2. Furthermore, additional articles were included in the review by referencing the bibliographies of previously acquired articles.
Table 1
| Anterior cruciate ligament reconstruction |
| Anterior cruciate ligament repair |
| Anterior cruciate ligament augmentation |
| Autografts for anterior cruciate ligament reconstruction |
| Allografts for anterior cruciate ligament reconstruction |
| Synthetic grafts for anterior cruciate ligament reconstruction |
| Lateral extra-articular tenodesis |
| Anterolateral ligament reconstruction |
| Anterior closed-wedge high tibial osteotomy |
Table 2
| Items | Specification |
|---|---|
| Date of search | 10/8/2022–5/8/2023 |
| Databases and other sources searched | PubMed |
| Search terms used | Please see Table 1 |
| Timeframe | From origin until 5/8/2023 |
| Inclusion and exclusion criteria | Inclusion criteria: original articles and review articles about surgical techniques, graft selections, and additional procedures of anterior cruciate ligament injury written in English |
| Exclusion criteria: (I) articles not written in English, (II) case reports or studies reporting less than 10 cases | |
| Selection process | Selection was conducted by a single author (Nukuto K) |
Results
Surgical techniques (Table 3)
Table 3
| Surgical techniques | Pros | Cons |
|---|---|---|
| ACL reconstruction | ||
| TT | – | Non-anatomic femoral tunnel position (34,35) |
| Transportal | Femoral tunnel position more anatomical than TT (36) | Stil high graft failure rate and osteo-arthritic changes (23-26) |
| Better rotatory stability of the knee than TT (10,36-39) | The injury of the infrapatellar branch of the saphenous nerve injury (37) | |
| All-inside | Capable of preserving the epiphysis (40) | A long learning curve (41) |
| Less invasive technique (41) | Technically difficult (41) | |
| Over-the-top | Capable of preserving the epiphysis (42) | non-anatomic reconstruction (43) |
| Good knee stability in revision and skeletally immature cases (42,44,45) | High graft failure rate in younger patients (42,45,46) | |
| Double-bundle | Better knee stability than single-bundle (11,47,48) | Long learning curve (49) |
| Similar or better clinical outcomes compared to single-bundle (50-55) | High costs (56) | |
| More anatomical reconstruction (57,58) | Tunnel coalition (59-63) | |
| ACL augmentation | Good indication for partial ACL tear (64-67) | Technically difficult (68) |
| More graft synovial coverage and preservation of proprioceptive function (65,66,69) | Graft hypertrophy (Cyclops and ROM limitation) (13,66,67) | |
| Better knee stability (65,66) | ||
| ACL repair | Good indication for acute proximal ACL tear (70,71) | A higher rerupture rate (72-74) |
| Preserving proprioceptive function and more normal knee joint mechanics (75) | No long-term results with new techniques (76-79) |
ACL, anterior cruciate ligament; TT, transtibial; ROM, range of motion.
ACL reconstruction
ACL reconstructions are performed to restore the knee stability and are essential for young patients with ACL injuries who wish to return to sports (80,81). In the early 1990s, arthroscopic ACL reconstructions were performed with ‘non-anatomic’ reconstruction using the TT technique to create a femoral tunnel. But in this technique the femoral tunnel is created from the tibial tunnel, the femoral tunnel is created in the ‘over-the-top’ position, which is a non-anatomic position (9). Improper positioning of the femoral tunnel resulted in the secondary knee osteoarthritis and clinical failures due to persistent instability (37,82,83). To create a femoral tunnel closer to the anatomical position, the anteromedial portal technique (transportal technique) was developed and is now widely performed as an ‘anatomic’ reconstruction technique (36). The bone tunnel drilled through the anteromedial portal tends to be inclined more towards the lateral cortex of the lateral femoral condyle. This inclination ultimately leads to superior rotatory stabilization of the knee joint when compared to TT technique (38). Compared to the TT technique, the anteromedial portal technique has been reported to provide superior knee stability, better clinical outcomes, and a reduced risk of OA progression (10,37,39).
In recent years, the all-inside technique has been reported as a less invasive technique. This technique uses an outside-in approach to create bony tunnel in both the femur and tibia, and an adjustable suspensory device is used to fix the graft (41). This technique allows for preservation of the epiphysis, and Placella et al. (40) reported that ACL reconstruction using the all-inside technique was performed for ACL injuries in immature bone patients, and all patients returned to sports (average 6.4 months) and no rerupture were observed at 8 years of follow-up. However, the all-inside technique is technically difficult and requires a long learning curve. For example, the graft must keep tension in the socket and must not bottom out in the socket (41).
The over-the-top technique has also been performed as one of the ACL reconstruction techniques (84). This technique has been performed on skeletally immature patients (42) and revision cases (44), and Nagai et al. (45) demonstrated good anterior and rotational stability in both cases. However, in skeletally immature patients, graft failures of 12.5–25% have been reported (42,45,46), possibly due to smaller graft size in younger patients (85). Moreover, there have also been some recent reports of over-the-top techniques combined with LET (86,87). Grassi et al. (87) reported good patient reported outcomes with a minimum 10-year follow-up, with only 3% resulting in revision ACL reconstruction. However, this technique is a non-anatomic reconstruction and may increase stress on the graft (43).
When considering anatomic ACL reconstruction, it should be remembered that the ACL consists of two bundles, anteromedial (AM) and posterolateral (PL) bundles. Since the single-bundle (SB) ACL reconstruction can only reconstruct the AM, the PL or something similar, DB ACL reconstruction technique was developed in the search for a more anatomic restoration of the structure (57,58). In biomechanical studies, Yagi et al. (11) reported that anterior tibial translation of DB ACL reconstruction was closer to intact ACL than SB ACL reconstruction, and that DB ACL reconstruction showed a greater force than SB ACL reconstruction for rotatory loads. In the study using an intraoperative navigation system, Plaweski et al. (47) reported that DB ACL reconstruction was superior in terms of both rotatory and anteroposterior laxity. Moreover, in a meta-analysis of biomechanical comparison, Oh et al. (48) reported that DB ACL reconstruction was superior in terms of anteroposterior stability. In clinical studies, however, most reports indicate that DB and SB ACL reconstruction are not different in clinical outcomes (50-52), although there are some reports that DB ACL reconstruction is superior to SB ACL reconstruction in terms of postoperative rotatory and anteroposterior knee stability (53-55). In the randomized clinical trial with 10 years follow-up, Balasingam et al. (88) reported that there were no significant differences in the pivot-shift grade, anteroposterior stability using KT-1000 knee ligament arthrometer (KT-1000) (MEDmetric Corp., San Diego, CA, USA), a range of motion (ROM) and patients reported outcomes in 39 DB patients and 31 SB patients who were available for 10-year follow-up. In the systematic reviews, Mascarenhas et al. (53) reported that in DB ACL reconstructions, postoperative knee stabilities measured by the pivot-shift testing and KT-1000 were better than SB ACL reconstructions, but clinical outcomes and graft failure rates were no difference between two techniques. Alomari et al. reported that at short-term follow-up, DB ACL reconstructions showed better knee stability and clinical outcomes than SB ACL reconstructions, but at mid- and long- term follow-up, there were no difference in knee stability and clinical outcomes between two techniques (55).
Since there are few reports which demonstrated obvious clinical benefit of DB procedure over SB, DB ACL reconstructions are becoming less frequent due to the difficulty of the procedure (49) and high costs (56).
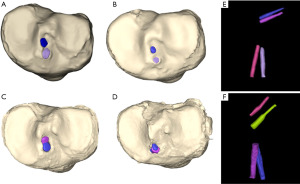
However, there may be some reasons why DB and SB ACL reconstructions have similar results in recent clinical research, even though some biomechanical researches have shown DB ACL reconstructions to be more stable. First, most clinical studies only evaluate knee rotatory instability in terms the clinical grading of the pivot-shift, which may not be an accurate assessment of stability (89-91). In a prospective randomized study comparing DB ACL reconstructions and SB ACL reconstructions, Araki et al. (92) reported that DB ACL reconstructions was superior to SB ACL reconstructions in terms of knee stability as assessed by electromagnetic measurement system (EMS) at 1 year postoperatively. Therefore, it is necessary to evaluate the rotatory knee stability using quantitative evaluation methods and to accumulate data in the future. Next, tunnel coalition is a common surgical complication after DB ACL reconstruction (59-61) (Figure 1), and it literally fails to achieve true double-bundle structure of the ACL. Femoral and tibial tunnel coalition is reported to be 0–64% and 0–77%, respectively (62), and tibial tunnel coalition influenced postoperative rotatory instability, as reported in a clinical study using EMS (63). Therefore, it would be necessary that a ‘true’ DB ACL reconstruction without tunnel coalition is needed to achieve a more anatomical ACL reconstruction technique.
ACL augmentation
Partial ACL tears occur in 10–35% of all ACL injuries (93) and ACL augmentation is a technique to preserve the remaining remnant of a partial ACL tear (64-67). The advantage of preserving the remnant is that blood flow is preserved, which may facilitate the graft healing process (69) and some studies reported that more synovial coverage was identified in ACL augmentation cases (65,66). In addition, proprioceptive function may be preserved, and residual ligaments may contribute to better knee stability in the early postoperative period (69). Nakamae et al. (65) reported that side-to-side difference in anterior translation at 1 year after surgery was better than SB reconstruction and Matsushita et al. (66) reported that knee stability at 1 year after PL augmentation was as good as double-bundle reconstruction. Disadvantages include procedural difficulty and graft hypertrophy. If the surgeon is experienced in the technique, the operation time can be slightly prolonged (68), but the remnant must not be injured. In addition, if graft hypertrophy occurs, it may result in cyclops and ROM limitation (13). Although the frequency of cyclops is only a few percent (66,67), it is important to be aware of it.
ACL repair
ACL repair had hardly been performed since 1976, when Feagin et al. (94) published the 5-year postoperative outcomes of open ACL repair and found that reinjury after ACL repair occurred in 17 of 32 patients and postoperative instability was indicated by 94%. Since then, ACL reconstruction has become the gold standard of surgical treatment for ACL injury. However, ACL reconstruction also has problems such as pain at the graft harvest site (95), muscle weakness (96), anterior knee pain (15), and osteoarthritic change after surgery (26). So, arthroscopic ACL repair again has attracted more attention. ACL repair can preserve the native ACL’s insertion site, thus preserving proprioceptive function and more normal knee joint mechanics and potentially reducing the incidence of postoperative OA (75). In addition, ACL repair has been reported to have no complications related to graft harvesting (97) and faster postoperative functional recovery (81). While recent ACL repair has reported good short-term results (12,98,99), a higher rerupture rate than ACL reconstruction has been also reported (72-74). Achtnich et al. (72) reported that at a mean follow-up of 28 months, ACL repair for acute proximal ACL tears resulted in rerupture in 3/20 (15%) patients, Osti et al. (73) reported that at the 12-month follow-up, primary ACL repair with dynamic intraligamentary stabilization (DIS) resulted in rerupture in 10/57 patients. A young age, a high Tegner score prior to injury and midsubstance tears were identified as risk factors for rerupture after ACL repair (12,99,100). The arterial blood supply to the ACL was more plentiful proximally than centrally or distally (70) and that vascularity was increased in a torn ACL compared to an intact ACL (71). So, from an anatomical point of view, proximal ACL tear seems to be a good indication for ACL repair. Moreover, there are no reports of ACL repair performed at longer intervals after injury, but some recent studies have reported good short-term results with ACL repair performed from 13 days to 2 months after injury (12,98,99), so, ACL repair may be indicated for acute ACL injury.
There are a variety of ACL repair techniques currently being performed, including DIS (76), internal brace ligament augmentation (77), suture anchor primary repair (SAPR) (78), and bridge-enhanced ACL repair (BEAR) (79), each with good short-term results, but ACL repair should be performed in a targeted manner because of the risk of rerupture.
Graft selection (Table 4)
Table 4
| Graft type | Pros | Cons |
|---|---|---|
| HT autograft | Low graft failure rate (2.5–9.0%) (95,101-103) | Extension loss (104-106) |
| Good clinical outcomes (14,15,101) | Higher incidence of deep infections than BTB (107) | |
| Greater mechanical properties in tensile road, stiffness, and cross-sectional area than BTB (81,105) | Increased laxity over time (15) | |
| BTB autograft | Low graft failure rate (2.0–7.0%) (95,101-103) | Anterior knee pain and kneeling pain (14,15) |
| Good clinical outcomes (14,15,101) | Long-term degenerative change (15,108) | |
| Contralateral ACL ruptures more likely than in HT (104) | ||
| QT autograft | Low graft failure rate (2.1–4.1%) (95,109,110) | Lower knee extensor strength than HT (111) |
| Superior to HT and BTB in terms of donor site morbidity (95,109,112) | ||
| Similar clinical outcomes to HT and BTB (95,109,113) | ||
| PLT autograft | High muscle strength (114-116) | A risk of the superficial peroneal nerve (17) |
| Similar clinical outcomes to HT (18) | Potential for decreased clinical outcomes around the foot and ankle (18) | |
| Possible to preserve muscle strength around the knee (18) | ||
| Allograft | No donor site morbidity (117) | Higher revision and graft failure rate in young patients (21) |
| Graft failure rates as same as autograft over age 40 (118) | ||
| Synthetic graft | Good short-term functional outcomes (34,35) | High graft rupture rate at long-term follow-up (119,120) |
| No donor site morbidity (34,35) | Possibility of synovitis and osteoarthritic changes (121-123) |
HT, hamstrings tendon; BTB, bone-patellar tendon-bone; QT, quadriceps tendon; PLT, peroneus longus tendon; ACL, anterior cruciate ligament.
Autograft
HT, BTB, and QT are the most commonly used as autografts for ACL reconstruction, but the gold standard of the graft source still does not exist. Until around 2008, BTB was most frequently used, but HT has gained in popularity since then, accounting for about half of the total in 2020. QT has recently increased since around 2014, and it is currently about 10% of the total (16).
BTB and HT have been reported to have a low graft failure rate (BTB: 2.0–7.0%, HT: 2.5–9.0%) (95,101-103) and similar good clinical outcomes (14,15,101). However, about BTB, anterior knee pain and kneeling pain (14,15), and long-term degenerative change have been reported (15,108). In addition, contralateral ACL ruptures were reported to be more likely than in HT (104). Regarding HT, biomechanical studies showed HT had greater mechanical properties in tensile road, stiffness, and cross-sectional area than BTB or QT (81,105). Meanwhile, some studies have reported that HT was associated with an extension loss (104-106), a higher incidence of deep infections than BTB (107), and an increased laxity over time (15).
QT has been increasing its popularity over the last ten years. The graft failure rate of QT has been reported to be 2.1–4.1%, which is similar to that of HT and BTB (95,109,110). Regarding donor site morbidity such as anterior knee pain, kneeling pain, tenderness and numbness, QT has been reported in recent years to be superior to HT and BTB (95,109,112). In systematic reviews and meta-analyses, clinical outcomes of ACL reconstruction using QT were reported to be similar to those of HT and BTB (95,109), and Brinkman et al. (113) reported that there was no difference in 5-year patient reported outcomes between QT and HT. Furthermore, Cavaignac et al. (124) reported that QT was better than HT in terms of the International Knee Documentation Committee (IKDC) subjective score and the Lysholm score at 3.6 years of follow-up. But some reports of ACL reconstruction using QT showed increased laxity than HT at 24 months postoperatively (125) and lower knee extensor strength at 12 months postoperatively than HT (111), so continued research on the selection of tendon grafts is required.
In recent years, PLT has also been used. Biomechanical studies have reported that it has as much tensile strength as a four-strand HT (114) and that its ultimate tensile strength is approximately equal to that of the native ACL (115,116). In a systematic review, He et al. (18) reported that PLT showed comparable functional outcomes and knee stability compared to HT, with no significant difference in donor site pain. However, the American Orthopaedic Foot and Ankle Society (AOFAS) score, which indicates the clinical outcome of the foot and ankle, is lower than preoperatively (18), and there is a risk of injury to the superficial peroneal nerve during graft harvesting (17), so further research is needed regarding preservation of foot function.
Allograft
Among the allograft options for ACL reconstruction are HT, QT, BTB, tibialis anterior, tibialis posterior, and Achilles tendon (81). It has been reported that allografts are associated with more revisions and graft failures (117,126), and Zhao et al. (21) reported that the failure rate of allografts is 2.63 times higher than that of autografts. However, Kaeding et al. (118) reported that the difference between allograft and autograft failure rates decreases with increasing age, with only a 2% difference in the 40-year-old patients. Therefore, in areas where allografts are available, allografts may be considered for patients older than 40 years.
Synthetic graft
Since the 1980s, many arthroscopic ACL reconstructions using synthetic grafts have been performed, but the long-term results have been poor, with high rates of graft failures, synovitis, and osteoarthritic changes (121-123). In recent years, the Ligament Advanced Reinforcement System (LARS; Surgical Implants and Devices, Arc-sur-Tille, France) has been used in ACL reconstruction (127). Favorable functional outcomes and low graft failure rates in the short-term follow-up have been reported (34,35). Nau et al. (34) reported that any of the subscales of Knee Injury and Osteoarthritis Outcome Score (KOOS) and Tegner score at 2 years postoperatively were not significantly different between LARS and BTB autograft. Gao et al. (35) reported that ACL reconstruction using LARS with a mean follow-up of 50 months showed graft failures in only 3/159 patients and residual grade 2 pivot-shift in 4 patients. While Jia et al. reported a graft failure rate of 4.4% at 7 years postoperatively, many reports showed high graft failure rates (31–39%) at middle and long-term follow-up (119,120). Therefore, the synthetic graft should not be selected as the first-choice graft to be used.
Additional procedures (Table 5)
Table 5
| Additional procedures | Pros | Cons |
|---|---|---|
| Anterolateral ligament reconstruction | Good clinical outcomes and low graft rupture rate for high-grade pivot shift patients (32,128-131) | The presence of ALL is not clear (132) |
| Non-anatomic reconstructive procedure (133) | ||
| Lateral extra-articular tenodesis | Good indication for high-grade pivot shift or revision cases (31,134) | The possibility of lateral osteoarthritis (135) |
| No graft harvesting required for LET (134) | ||
| Anterior closed-wedge high tibial osteotomy | Good indication for high posterior tibial slope and revision ACL reconstruction cases (29,30,136) | Some complications of osteotomy (delayed un-ion, pseudoarthrosis, infection) (137) |
ALL, anterolateral ligament; LET, lateral extra-articular tenodesis; ACL, anterior cruciate ligament.
Additional procedures may be considered for gross rotatory knee laxity or revision ACL reconstruction cases. The main additional techniques for soft tissues are ALLR (28) and LET (27).
ALL is described as a secondary stabilizer for anterior tibial translation and internal rotation, especially at 30°–90° of knee flexion (138,139), and Segond fracture is considered as an avulsion fracture on the tibial attachment of ALL (140,141). A lot of good clinical results have been reported for ALLR (32,128-131). Hamido et al. (131) reported that in male athletes with high-grade pivot shifts, combined ACL reconstruction and ALLR had a lower graft rupture rate and a better postoperative IKDC score. Sonnery-Cottet et al. (32) reported a better long-term ACL graft rupture rate and a lower overall rate of reoperation of combined ACL reconstruction and ALLR at 9 years postoperatively. But, on the other hand, the presence of ALL is not yet clear as a distinct ligamentous structure. Guenther et al. (132) reported that ALL is not a traditional ligament, but part of the anterolateral capsule, like a sheet of tissue. Herbst et al. (133) reported that the anterolateral complex is composed of the iliotibial band and the anterolateral joint capsule. Since ALLR may be a non-anatomical reconstructive procedure, it should be performed with caution.
Regarding LET, cadaver studies have reported that combined ACL reconstruction and LET is more effective in controlling rotatory knee laxity than isolated ACL reconstruction in cases of anterolateral complex injuries (141,142). Some good results in clinical studies have also been reported for LET. Getgood et al. (31) reported that for young patients with ACL injuries of pivot grade 2 or higher and younger than 25 years, combined ACL reconstruction and LET had a lower graft rupture rate and a lower clinical failure rate than isolated ACL reconstruction. According to a meta-analysis which was performed by Park et al. (134) combined ACL reconstruction and LET had better IKDC and Lysholm scores and a lower graft failure rate than isolated ACL reconstruction. Although the possibility of postoperative lateral OA has been reported due to overconstraint of the lateral compartment after LET (135), Declercq et al. (143) reported that the risk of postoperative lateral OA is not increased. So, further research is needed on this complication.
Recently, bony morphology has been reported as a factor to influence ACL injury and residual rotational instability after ACL reconstruction (144,145). The high PTS has particularly gained attention because tension on the ACL during weightbearing increased in the high PTS, and stability would be impaired after ACL reconstruction (146). Therefore, ACW-HTO has been increasingly performed recently to decrease the posterior slope (29,30,33). Some researcher reported that ACW-HTO should be considered if PTS is greater than 12° (29,30,136). Because of various complications of osteotomy, such as delayed union, pseudoarthrosis, and infection, some reports suggest that ACW-HTO should be selectively performed, for example, in revision ACL reconstruction (137).
Strengths and limitations
Strength is that no review article has combined the surgical techniques of ACL reconstruction, ACL repair, and ACL augmentation into a single surgical procedure for ACL injuries, and this review article covers all the important surgical techniques and graft selections for ACL injuries in recent years. This article will be of particular interest to young surgeons. The limitation is that this article is not a systematic review and does not cover all previous papers related to the topic. However, this article clearly describes the advantages and disadvantages of each technique, grafts and additional procedures, so the issues to be aware of in actual surgical preparations can be well understood in this article.
Conclusions
Anatomic ACL reconstruction guarantees good clinical results. Previous DB ACL reconstructions have been failed to demonstrate obvious advantage over anatomic SB, while most of them might not have been successful in restoring double bundle structure due to tunnel coalition. ACL repair has shown good results in recent years, and long-term results are expected in the future. Allografts and synthetic grafts have a high graft failure rate, and autografts should be the first choice, but further study is needed to determine which autograft is best. There may be cases that require additional procedures such as LET or ALLR, but we should first get down to anatomic ACL reconstruction.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-39/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-39/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-39/coif). YH serves as an unpaid editorial board member of Annals of Joint from December 2022 to November 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and Diagnosis of Anterior Cruciate Ligament Injuries. Clin Sports Med 2017;36:1-8. [Crossref] [PubMed]
- Bowman EN, Limpisvasti O, Cole BJ, et al. Anterior Cruciate Ligament Reconstruction Graft Preference Most Dependent on Patient Age: A Survey of United States Surgeons. Arthroscopy 2021;37:1559-66. [Crossref] [PubMed]
- Granan LP, Bahr R, Steindal K, et al. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med 2008;36:308-15. [Crossref] [PubMed]
- Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 2014;42:2363-70. [Crossref] [PubMed]
- Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of Anterior Cruciate Ligament Tears and Reconstruction: A 21-Year Population-Based Study. Am J Sports Med 2016;44:1502-7. [Crossref] [PubMed]
- Kopf S, Forsythe B, Wong AK, et al. Nonanatomic tunnel position in traditional transtibial single-bundle anterior cruciate ligament reconstruction evaluated by three-dimensional computed tomography. J Bone Joint Surg Am 2010;92:1427-31. [Crossref] [PubMed]
- Kopf S, Forsythe B, Wong AK, et al. Transtibial ACL reconstruction technique fails to position drill tunnels anatomically in vivo 3D CT study. Knee Surg Sports Traumatol Arthrosc 2012;20:2200-7. [Crossref] [PubMed]
- Kondo E, Merican AM, Yasuda K, et al. Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med 2011;39:279-88. [Crossref] [PubMed]
- Liu C, Wang Y, Li Z, et al. Tibiofemoral joint contact area and stress after single-bundle anterior cruciate ligament reconstruction with transtibial versus anteromedial portal drilling techniques. J Orthop Surg Res 2018;13:247. [Crossref] [PubMed]
- Rothrauff BB, Jorge A, de Sa D, et al. Anatomic ACL reconstruction reduces risk of post-traumatic osteoarthritis: a systematic review with minimum 10-year follow-up. Knee Surg Sports Traumatol Arthrosc 2020;28:1072-84. [Crossref] [PubMed]
- Yagi M, Wong EK, Kanamori A, et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med 2002;30:660-6. [Crossref] [PubMed]
- Ferreira A, Saithna A, Carrozzo A, et al. The Minimal Clinically Important Difference, Patient Acceptable Symptom State, and Clinical Outcomes of Anterior Cruciate Ligament Repair Versus Reconstruction A Matched-Pair Analysis From the SANTI Study Group. Am J Sports Med 2022;50:3522-32. [Crossref] [PubMed]
- Bosco F, Giustra F, Crivellaro M, et al. Is augmentation the best solution in partial anterior cruciate ligament tears? A literature systematic review and meta-analysis. J Orthop 2023;36:11-7. [Crossref] [PubMed]
- Anderson MJ, Browning WM 3rd, Urband CE, et al. A Systematic Summary of Systematic Reviews on the Topic of the Anterior Cruciate Ligament. Orthop J Sports Med 2016;4:2325967116634074. [Crossref] [PubMed]
- Ciccotti MC, Secrist E, Tjoumakaris F, et al. Anatomic Anterior Cruciate Ligament Reconstruction via Independent Tunnel Drilling: A Systematic Review of Randomized Controlled Trials Comparing Patellar Tendon and Hamstring Autografts. Arthroscopy 2017;33:1062-1071.e5. [Crossref] [PubMed]
- Arnold MP, Calcei JG, Vogel N, et al. ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc 2021;29:3871-6. [Crossref] [PubMed]
- Zhao J, Huangfu X. The biomechanical and clinical application of using the anterior half of the peroneus longus tendon as an autograft source. Am J Sports Med 2012;40:662-71. [Crossref] [PubMed]
- He J, Tang Q, Ernst S, et al. Peroneus longus tendon autograft has functional outcomes comparable to hamstring tendon autograft for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2021;29:2869-79. [Crossref] [PubMed]
- Thomas AC, Wojtys EM, Brandon C, et al. Muscle Atrophy Contributes to Quadriceps Weakness after ACL Reconstruction. J Sci Med Sport 2016;19:7-11. [Crossref] [PubMed]
- Cristiani R, Forssblad M, Engstrom B, et al. Risk Factors for Abnormal Anteroposterior Knee Reconstruction. Arthroscopy 2018;34:2478-84. [Crossref] [PubMed]
- Zhao D, Pan JK, Lin FZ, et al. Risk Factors for Revision or Rerupture After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med 2023;51:3053-75. [Crossref] [PubMed]
- Ventura A, Terzaghi C, Legnani C, et al. Synthetic grafts for anterior cruciate ligament rupture: 19-year outcome study. Knee 2010;17:108-13. [Crossref] [PubMed]
- Leys T, Salmon L, Waller A, et al. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med 2012;40:595-605. [Crossref] [PubMed]
- Kaeding CC, Pedroza AD, Reinke EK, et al. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med 2015;43:1583-90. [Crossref] [PubMed]
- Sanders TL, Pareek A, Hewett TE, et al. Long-term rate of graft failure after ACL reconstruction: a geographic population cohort analysis. Knee Surg Sports Traumatol Arthrosc 2017;25:222-8. [Crossref] [PubMed]
- Ajuied A, Wong F, Smith C, et al. Anterior Cruciate Ligament Injury and Radiologic Progression of Knee Osteoarthritis A Systematic Review and Meta-analysis. Am J Sports Med 2014;42:2242-52. [Crossref] [PubMed]
- Schindler OS. Surgery for anterior cruciate ligament deficiency: a historical perspective. Knee Surg Sports Traumatol Arthrosc 2012;20:5-47. [Crossref] [PubMed]
- Sonnery-Cottet B, Daggett M, Helito CP, et al. Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction. Arthrosc Tech 2016;5:e1253-9. [Crossref] [PubMed]
- Dejour D, Pungitore M, Valluy J, et al. Preoperative laxity in ACL-deficient knees increases with posterior tibial slope and medial meniscal tears. Knee Surg Sports Traumatol Arthrosc 2019;27:564-72. [Crossref] [PubMed]
- Song GY, Ni QK, Zheng T, et al. Slope-Reducing Tibial Osteotomy Combined With Primary Anterior Cruciate Ligament Reconstruction Produces Improved Knee Stability in Patients With Steep Posterior Tibial Slope, Excessive Anterior Tibial Subluxation in Extension, and Chronic Meniscal Poster. Am J Sports Med 2020;48:3486-94. [Crossref] [PubMed]
- Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am J Sports Med 2020;48:285-97. [Crossref] [PubMed]
- Sonnery-Cottet B, Haidar I, Rayes J, et al. Long-term Graft Rupture Rates After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction: A Matched-Pair Analysis From the SANTI Study Group. Am J Sports Med 2021;49:2889-97. [Crossref] [PubMed]
- Bosco F, Giustra F, Giai Via R, et al. Could anterior closed - wedge high tibial osteotomy be a viable option in patients with high posterior tibial slope who undergo anterior cruciate ligament reconstruction ? A systematic review and meta - analysis. Eur J Orthop Surg Traumatol 2023;33:2201-14. [Crossref] [PubMed]
- Nau T, Lavoie P, Duval N. A new generation of artificial ligaments in reconstruction of the anterior cruciate ligament: Two-year follow-up of a randomised trial. J Bone Joint Surg Br 2002;84:356-60. [Crossref] [PubMed]
- Gao K, Chen S, Wang L, et al. Anterior Cruciate Ligament Reconstruction With LARS Artificial Ligament: A Multicenter Study With 3- to 5-Year Follow-up. Arthroscopy 2010;26:515-23. [Crossref] [PubMed]
- O'Donnell JB, Scerpella TA. Endoscopic anterior cruciate ligament reconstruction: modified technique and radiographic review. Arthroscopy 1995;11:577-84. [Crossref] [PubMed]
- Loucas M, Loucas R, D’Ambrosi R, et al. Clinical and Radiological Outcomes of Anteromedial Portal Versus Transtibial Technique in ACL Reconstruction A Systematic Review. Orthop J Sports Med 2021;9:23259671211024591. [Crossref] [PubMed]
- Dargel J, Schmidt-Wiethoff R, Fischer S, et al. Femoral bone tunnel placement using the transtibial tunnel or the anteromedial portal in ACL reconstruction: a radiographic evaluation. Knee Surg Sports Traumatol Arthrosc 2009;17:220-7. [Crossref] [PubMed]
- Liu Z, Jiang J, Yi Q, et al. An increased posterior tibial slope is associated with a higher risk of graft failure following ACL reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc 2022;30:2377-87. [Crossref] [PubMed]
- Placella G, Bartoli M, Peruzzi M, et al. Return to sport activity after anterior cruciate ligament reconstruction in skeletally immature athletes with manual drilling original all inside reconstruction at 8 years follow-up. Acta Orthop Traumatol Turc 2016;50:635-8. [Crossref] [PubMed]
- Lubowitz JH, Ahmad CS, Anderson K. All-inside anterior cruciate ligament graft-link technique: second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy 2011;27:717-27. [Crossref] [PubMed]
- Demange MK, Camanho GL. Nonanatomic anterior cruciate ligament reconstruction with double-stranded semitendinosus grafts in children with open physes: minimum 15-year follow-up. Am J Sports Med 2014;42:2926-32. [Crossref] [PubMed]
- Samitier G, Marcano AI, Alentorn-Geli E, et al. Failure of Anterior Cruciate Ligament Reconstruction. Arch Bone Jt Surg 2015;3:220-40. [PubMed]
- Usman MA, Kamei G, Adachi N, et al. Revision single-bundle anterior cruciate ligament reconstruction with over-the-top route procedure. Orthop Traumatol Surg Res 2015;101:71-5. [Crossref] [PubMed]
- Nagai K, Rothrauff BB, Li RT, et al. Over-the-top ACL reconstruction restores anterior and rotatory knee laxity in skeletally immature individuals and revision settings. Knee Surg Sports Traumatol Arthrosc 2020;28:538-43. [Crossref] [PubMed]
- McIntosh AL, Dahm DL, Stuart MJ. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy 2006;22:1325-30. [Crossref] [PubMed]
- Plaweski S, Grimaldi M, Courvoisier A, et al. Intraoperative comparisons of knee kinematics of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2011;19:1277-86. [Crossref] [PubMed]
- Oh JY, Kim KT, Park YJ, et al. Biomechanical comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction: a meta-analysis. Knee Surg Relat Res 2020;32:14. [Crossref] [PubMed]
- Harner CD, Poehling GG. Double bundle or double trouble? Arthroscopy 2004;20:1013-4. [Crossref] [PubMed]
- Meredick RB, Vance KJ, Appleby D, et al. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament - A meta-analysis. Am J Sports Med 2008;36:1414-21. [Crossref] [PubMed]
- Mayr HO, Bruder S, Hube R, et al. Single-Bundle Versus Double-Bundle Anterior Cruciate Ligament Reconstruction-5-Year Results. Arthroscopy 2018;34:2647-53. [Crossref] [PubMed]
- Irrgang JJ, Tashman S, Patterson CG, et al. Anatomic single vs. double-bundle ACL reconstruction: a randomized clinical trial-Part 1: clinical outcomes. Knee Surg Sports Traumatol Arthrosc 2021;29:2665-75. [Crossref] [PubMed]
- Mascarenhas R, Cvetanovich GL, Sayegh ET, et al. Does Double-Bundle Anterior Cruciate Ligament Reconstruction Improve Postoperative Knee Stability Compared With Single-Bundle Techniques? A Systematic Review of Overlapping Meta-analyses. Arthroscopy 2015;31:1185-96. [Crossref] [PubMed]
- Severyns M, Mallet J, Plawecki S. Comparison of Rotatory and Sagittal Laxity After Single-Bundle Versus Double-Bundle ACL Reconstruction: Outcomes at 7-Year Follow-up. Orthop J Sports Med 2022;10:23259671221104408. [Crossref] [PubMed]
- Alomari MS, Ghaddaf AA, Abdulhamid AS, et al. Single Bundle Versus Double Bundle Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Indian J Orthop 2022;56:1669-84. [Crossref] [PubMed]
- Sernert N, Hansson E. Similar cost-utility for double- and single-bundle techniques in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:634-47. [Crossref] [PubMed]
- Muneta T, Sekiya I, Yagishita K, et al. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy 1999;15:618-24. [Crossref] [PubMed]
- Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy 2004;20:1015-25. [Crossref] [PubMed]
- Kiekara T, Järvelä T, Huhtala H, et al. Tunnel communication and increased graft signal intensity on magnetic resonance imaging of double-bundle anterior cruciate ligament reconstruction. Arthroscopy 2014;30:1595-601. [Crossref] [PubMed]
- Kawaguchi Y, Kondo E, Onodera J, et al. Tunnel Enlargement and Coalition After Anatomic Double-Bundle Anterior Cruciate Ligament Reconstruction With Hamstring Tendon Autografts: A Computed Tomography Study. Orthop J Sports Med 2013;1:2325967113486441. [Crossref] [PubMed]
- Siebold R, Cafaltzis K. Differentiation between intraoperative and postoperative bone tunnel widening and communication in double-bundle anterior cruciate ligament reconstruction: a prospective study. Arthroscopy 2010;26:1066-73. [Crossref] [PubMed]
- Nakanishi Y, Nagai K, Kay J, et al. The incidence of tibial tunnel coalition is higher than femoral tunnel coalition in double-bundle anterior cruciate ligament reconstruction using hamstring autografts: A systematic review. Orthop Traumatol Surg Res 2022;108:103407. [Crossref] [PubMed]
- Nukuto K, Hoshino Y, Yamamoto T, et al. Anatomic double-bundle anterior cruciate ligament reconstruction could not achieve sufficient control of pivot-shift when accompanying tibial tunnel coalition. Knee Surg Sports Traumatol Arthrosc 2021;29:3743-50. [Crossref] [PubMed]
- Yoon KH, Bae DK, Cho SM, et al. Standard anterior cruciate ligament reconstruction versus isolated single-bundle augmentation with hamstring autograft. Arthroscopy 2009;25:1265-74. [Crossref] [PubMed]
- Nakamae A, Ochi M, Deie M, et al. Clinical outcomes of second-look arthroscopic evaluation after anterior cruciate ligament augmentation: comparison with single- and double-bundle reconstruction. Bone Joint J 2014;96-B:1325-32. [Crossref] [PubMed]
- Matsushita T, Kuroda R, Nishizawa Y, et al. Clinical outcomes and biomechanical analysis of posterolateral bundle augmentation in patients with partial anterior cruciate ligament tears. Knee Surg Sports Traumatol Arthrosc 2017;25:1279-89. [Crossref] [PubMed]
- Iwaasa T, Tensho K, Koyama S, et al. Clinical outcome of a new remnant augmentation technique with anatomical double-bundle anterior cruciate ligament reconstruction: Comparison among remnant preservation, resection, and absent groups. Asia Pac J Sports Med Arthrosc Rehabil Technol 2021;25:22-9. [Crossref] [PubMed]
- Adachi N, Ochi M, Uchio Y, et al. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand 2002;73:330-4. [Crossref] [PubMed]
- Xie H, Fu Z, Zhong M, et al. Effects of remnant preservation in anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Front Surg 2022;9:952930. [Crossref] [PubMed]
- Toy BJ, Yeasting RA, Morse DE, et al. Arterial supply to the human anterior cruciate ligament. J Athl Train 1995;30:149-52. [PubMed]
- Takeuchi S, Rothrauff BB, Kanto R, et al. Superb microvascular imaging (SMI) detects increased vascularity of the torn anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2022;30:93-101. [Crossref] [PubMed]
- Achtnich A, Herbst E, Forkel P, et al. Acute Proximal Anterior Cruciate Ligament Tears : Versus Anatomic Single-Bundle Reconstruction. Arthroscopy 2016;32:2562-9. [Crossref] [PubMed]
- Osti M, El Attal R, Doskar W, et al. High complication rate following dynamic intraligamentary stabilization for primary repair of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2019;27:29-36. [Crossref] [PubMed]
- Ateschrang A, Schreiner AJ, Ahmad SS, et al. Improved results of ACL primary repair in one-part tears with intact synovial coverage. Knee Surg Sports Traumatol Arthrosc 2019;27:37-43. [Crossref] [PubMed]
- Kiapour AM, Murray MM. Basic science of anterior cruciate ligament injury and repair. Bone Joint Res 2014;3:20-31. [Crossref] [PubMed]
- Kohl S, Evangelopoulos DS, Schär MO, et al. Dynamic intraligamentary stabilisation: initial experience with treatment of acute ACL ruptures. Bone Joint J 2016;98-B:793-8. [Crossref] [PubMed]
- Heusdens CHW, Hopper GP, Dossche L, et al. Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: a case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 2019;27:60-7. [Crossref] [PubMed]
- DiFelice GS, Villegas C, Taylor S. Anterior Cruciate Ligament Preservation: Early Results of a Novel Arthroscopic Technique for Suture Anchor Primary Anterior Cruciate Ligament Repair. Arthroscopy 2015;31:2162-71. [Crossref] [PubMed]
- Murray MM, Kalish LA, Fleming BC, et al. Bridge-Enhanced Anterior Cruciate Ligament Repair Two-Year Results of a First-in-Human Study. Orthop J Sports Med 2019;7:2325967118824356. [Crossref] [PubMed]
- Musahl V, Karlsson J. Anterior Cruciate Ligament Tear. N Engl J Med 2019;380:2341-8. [Crossref] [PubMed]
- Musahl V, Engler ID, Nazzal EM, et al. Current trends in the anterior cruciate ligament part II: evaluation, surgical technique, prevention, and rehabilitation. Knee Surg Sports Traumatol Arthrosc 2022;30:34-51. [Crossref] [PubMed]
- Leiter JR, Gourlay R, McRae S, et al. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc 2014;22:1061-9. [PubMed]
- Johnson DL, Swenson TM, Irrgang JJ, et al. Revision anterior cruciate ligament surgery: experience from Pittsburgh. Clin Orthop Relat Res 1996;100-9. [Crossref] [PubMed]
- Jonsson H, Elmqvist LG, Kärrholm J, et al. Over-the-top or tunnel reconstruction of the anterior cruciate ligament? A prospective randomised study of 54 patients. J Bone Joint Surg Br 1994;76:82-7. [Crossref] [PubMed]
- Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy 2013;29:1948-53. [Crossref] [PubMed]
- Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL Reconstruction Plus Extra-articular Lateral Tenodesis With Hamstring Tendon Grafts Prospective Evaluation With 20-Year Minimum Follow-up. Am J Sports Med 2017;45:3233-42. [Crossref] [PubMed]
- Grassi A, Macchiarola L, Lucidi GA, et al. Ten-Year Survivorship, Patient-Reported Outcome Measures, and Patient Acceptable Symptom State After Over-the-Top Hamstring Anterior Cruciate Ligament Reconstruction With a Lateral Extra-articular Reconstruction: Analysis of 267 Consecutive Cases. Am J Sports Med 2021;49:374-83. [Crossref] [PubMed]
- Balasingam S, Karikis I, Rostgård-Christensen L, et al. Anatomic Double-Bundle Anterior Cruciate Ligament Reconstruction Is Not Superior to Anatomic Single-Bundle Reconstruction at 10-Year Follow-up: A Randomized Clinical Trial. Am J Sports Med 2022;50:3477-86. [Crossref] [PubMed]
- Kuroda R, Hoshino Y, Kubo S, et al. Similarities and differences of diagnostic manual tests for anterior cruciate ligament insufficiency: a global survey and kinematics assessment. Am J Sports Med 2012;40:91-9. [Crossref] [PubMed]
- Musahl V, Griffith C, Irrgang JJ, et al. Validation of Quantitative Measures of Rotatory Knee Laxity. Am J Sports Med 2016;44:2393-8. [Crossref] [PubMed]
- Noyes FR, Grood ES, Cummings JF, et al. An analysis of the pivot shift phenomenon. The knee motions and subluxations induced by different examiners. Am J Sports Med 1991;19:148-55. [Crossref] [PubMed]
- Araki D, Kuroda R, Kubo S, et al. A prospective randomised study of anatomical single-bundle versus double-bundle anterior cruciate ligament reconstruction: quantitative evaluation using an electromagnetic measurement system. Int Orthop 2011;35:439-46. [Crossref] [PubMed]
- van der List JP, Mintz DN, DiFelice GS. The Location of Anterior Cruciate Ligament Tears A Prevalence Study Using Magnetic Resonance Imaging. Orthop J Sports Med 2016;5:2325967117709966. [PubMed]
- Feagin JA Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med 1976;4:95-100. [Crossref] [PubMed]
- Dai W, Leng X, Wang J, et al. Quadriceps Tendon Autograft Versus Bone–Patellar Tendon–Bone and Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med 2022;50:3425-39. [Crossref] [PubMed]
- Tsai LC, Jeanfreau CM, Hamblin KA, et al. Time, graft, sex, geographic location, and isokinetic speed influence the degree of quadriceps weakness after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2022;30:3367-76. [Crossref] [PubMed]
- Rousseau R, Labruyere C, Kajetanek C, et al. Complications After Anterior Cruciate Ligament Reconstruction and Their Relation to the Type of Graft A Prospective Study of 958 Cases. Am J Sports Med 2019;47:2543-9. [Crossref] [PubMed]
- Hoogeslag RAG, Brouwer RW, Boer BC, et al. Acute Anterior Cruciate Ligament Rupture: Repair or Reconstruction? Two-Year Results of a Randomized Controlled Clinical Trial. Am J Sports Med 2019;47:567-77. [Crossref] [PubMed]
- Kösters C, Glasbrenner J, Spickermann L, et al. Repair With Dynamic Intraligamentary Stabilization Versus Primary Reconstruction of Acute Anterior Cruciate Ligament Tears 2-Year Results From a Prospective Randomized Study. Am J Sports Med 2020;48:1108-16. [Crossref] [PubMed]
- Krismer AM, Gousopoulos L, Kohl S, et al. Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilisation. Knee Surg Sports Traumatol Arthrosc 2017;25:3923-8. [Crossref] [PubMed]
- Gabler CM, Jacobs CA, Howard JS, et al. Comparison of Graft Failure Rate Between Autografts Placed via an Anatomic Anterior Cruciate Ligament Reconstruction Technique: A Systematic Review, Meta-analysis, and Meta-regression. Am J Sports Med 2016;44:1069-79. [Crossref] [PubMed]
- Samuelsen BT, Webster KE, Johnson NR, et al. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin Orthop Relat Res 2017;475:2459-68. [Crossref] [PubMed]
- Zhao L, Lu M, Deng M, et al. Outcome of bone-patellar tendon-bone vs hamstring tendon autograft for anterior cruciate ligament reconstruction: A meta-analysis of randomized controlled trials with a 5-year minimum follow-up. Medicine (Baltimore) 2020;99:e23476. [Crossref] [PubMed]
- Zhou P, Liu JC, Deng XT, et al. Hamstring autograft versus patellar tendon autograft for anterior cruciate ligament reconstruction, which graft has a higher contralateral anterior cruciate ligament injury rate? A meta-analysis of 5561 patients following the PRISMA guidelines. Medicine (Baltimore) 2020;99:e21540. [Crossref] [PubMed]
- West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg 2005;13:197-207. [Crossref] [PubMed]
- Goldblatt JP, Fitzsimmons SE, Balk E, et al. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy 2005;21:791-803. [Crossref] [PubMed]
- Bansal A, Lamplot JD, VandenBerg J, et al. Meta-analysis of the Risk of Infections After Anterior Cruciate Ligament Reconstruction by Graft Type. Am J Sports Med 2018;46:1500-8. [Crossref] [PubMed]
- Poehling-Monaghan KL, Salem H, Ross KE, et al. Long-Term Outcomes in Anterior Cruciate Ligament Reconstruction: A Systematic Review of Patellar Tendon Versus Hamstring Autografts. Orthop J Sports Med 2017;5:2325967117709735. [Crossref] [PubMed]
- Hurley ET, Mojica ES, Kanakamedala AC, et al. Quadriceps tendon has a lower re-rupture rate than hamstring tendon autograft for anterior cruciate ligament reconstruction - A meta-analysis. J ISAKOS 2022;7:87-93. [Crossref] [PubMed]
- Mouarbes D, Menetrey J, Marot V, et al. Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Outcomes for Quadriceps Tendon Autograft Versus Bone–Patellar Tendon–Bone and Hamstring-Tendon Autografts. Am J Sports Med 2019;47:3531-40. [Crossref] [PubMed]
- Johnston PT, Feller JA, McClelland JA, et al. Knee strength deficits following anterior cruciate ligament reconstruction differ between quadriceps and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 2022;30:1300-10. [Crossref] [PubMed]
- Slone HS, Romine SE, Premkumar A, et al. Quadriceps tendon autograft for anterior cruciate ligament reconstruction: a comprehensive review of current literature and systematic review of clinical results. Arthroscopy 2015;31:541-54. [Crossref] [PubMed]
- Brinkman JC, Tummala S V, Hassebrock JD, et al. Mid-Term Outcomes of the All-Soft Quadriceps Tendon Autograft are Non-Inferior to Hamstring Autograft in Primary Anterior Cruciate Ligament Reconstruction: Comparison with Minimum 5-year Follow up. Arthroscopy 2023;39:1008-13. [Crossref] [PubMed]
- Edi Mustamsir R, Yuarno Phatama K. Tensile strength comparison between peroneus longus and hamstring tendons: A biomechanical study. Int J Surg Open 2017;9:41-4. [Crossref]
- Woo SL, Hollis JM, Adams DJ, et al. Tensile properties of the human femur- anterior cruciate ligament-tibia complex the effects of specimen age and orientation. Am J Sports Med 1991;19:217-25. [Crossref] [PubMed]
- Aguila CM, Delcroix GJ, Kaimrajh DN, et al. Effects of gamma irradiation on the biomechanical properties of peroneus tendons. Open Access J Sports Med 2016;7:123-7. [Crossref] [PubMed]
- Bottoni CR, Smith EL, Shaha J, et al. Autograft Versus Allograft Anterior Cruciate Ligament Reconstruction: A Prospective, Randomized Clinical Study With a Minimum 10-Year Follow-up. Am J Sports Med 2015;43:2501-9. [Crossref] [PubMed]
- Kaeding CC, Aros B, Pedroza A, et al. Allograft Versus Autograft Anterior Cruciate Ligament Reconstruction: Predictors of Failure From a MOON Prospective Longitudinal Cohort. Sports Health 2011;3:73-81. [Crossref] [PubMed]
- Tulloch SJ, Devitt BM, Porter T, et al. Primary ACL reconstruction using the LARS device is associated with a high failure rate at minimum of 6-year follow-up. Knee Surg Sports Traumatol Arthrosc 2019;27:3626-32. [Crossref] [PubMed]
- Iliadis DP, Bourlos DN, Mastrokalos DS, et al. LARS Artificial Ligament Versus ABC Purely Polyester Ligament for Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med 2016;4:2325967116653359. [Crossref] [PubMed]
- Paulos LE, Rosenberg TD, Grewe SR, et al. The GORE-TEX anterior cruciate ligament prosthesis A long-term followup. Am J Sports Med 1992;20:246-52. [Crossref] [PubMed]
- Maletius W, Gillquist J. Long-term Results of Anterior Ligament Reconstruction with Prosthesis Cruciate a Dacron The Frequency of Osteoarthritis After Seven to Eleven Years. Am J Sports Med 1997;25:288-93. [Crossref] [PubMed]
- Murray AW, Macnicol MF. 10-16 year results of Leeds-Keio anterior cruciate ligament reconstruction. Knee 2004;11:9-14. [Crossref] [PubMed]
- Cavaignac E, Coulin B, Tscholl P, et al. Is Quadriceps Tendon Autograft a Better Choice Than Hamstring Autograft for Anterior Cruciate Ligament Reconstruction? A Comparative Study With a Mean Follow-up of 3.6 Years. Am J Sports Med 2017;45:1326-32. [Crossref] [PubMed]
- Lind M, Strauss MJ, Nielsen T, et al. Quadriceps tendon autograft for anterior cruciate ligament reconstruction is associated with high revision rates: results from the Danish Knee Ligament Registry. Knee Surg Sports Traumatol Arthrosc 2020;28:2163-9. [Crossref] [PubMed]
- Wright RW, Huston LJ, Haas AK, et al. Effect of graft choice on the outcome of revision anterior cruciate ligament reconstruction in the Multicenter ACL Revision Study (MARS) Cohort. Am J Sports Med 2014;42:2301-10. [Crossref] [PubMed]
- Dericks G. Ligament advanced reinforcement system anterior cruciate ligament reconstruction. Oper Tech Sports Med 1995;3:187-205. [Crossref]
- Zhang H, Qiu M, Zhou A, et al. Anatomic Anterolateral Ligament Reconstruction Improves Postoperative Clinical Outcomes Combined with Anatomic Anterior Cruciate Ligament Reconstruction. J Sports Sci Med 2016;15:688-96. [PubMed]
- Sonnery-Cottet B, Saithna A, Cavalier M, et al. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am J Sports Med 2017;45:1547-57. [Crossref] [PubMed]
- Pioger C, Gousopoulos L, Hopper GP, et al. Clinical Outcomes After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction With Bone–Patellar Tendon–Bone Grafts: A Matched-Pair Analysis of 2018 Patients From the SANTI Study Group. Am J Sports Med 2022;50:3493-501. [Crossref] [PubMed]
- Hamido F, Habiba AA, Marwan Y, et al. Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc 2021;29:1173-80. [Crossref] [PubMed]
- Guenther D, Rahnemai-Azar AA, Bell KM, et al. The Anterolateral Capsule of the Knee Behaves Like a Sheet of Fibrous Tissue. Am J Sports Med 2017;45:849-55. [Crossref] [PubMed]
- Herbst E, Albers M, Burnham JM, et al. The anterolateral complex of the knee: a pictorial essay. Knee Surg Sports Traumatol Arthrosc 2017;25:1009-14. [Crossref] [PubMed]
- Park YB, Lee HJ, Cho HC, et al. Combined Lateral Extra-articular Tenodesis or and Anterior Cruciate Ligament Reconstruction Improves Outcomes Compared to Isolated Reconstruction for Anterior Cruciate Ligament Tear : A Network Meta-analysis of Randomized Controlled Trials. Arthroscopy 2023;39:758-76.e10. [Crossref] [PubMed]
- Castoldi M, Magnussen RA, Gunst S, et al. A Randomized Controlled Trial of Bone–Patellar Tendon–Bone Anterior Cruciate Ligament Reconstruction With and Without Lateral Extra-articular Tenodesis: 19-Year Clinical and Radiological Follow-up. Am J Sports Med 2020;48:1665-72. [Crossref] [PubMed]
- Li Y, Zhang H, Zhang J, et al. Clinical outcome of simultaneous high tibial osteotomy and anterior cruciate ligament reconstruction for medial compartment osteoarthritis in young patients with anterior cruciate ligament-deficient knees: a systematic review. Arthroscopy 2015;31:507-19. [Crossref] [PubMed]
- Akoto R, Alm L, Drenck TC, et al. Slope-Correction Osteotomy with Lateral Extra-articular Tenodesis and Revision Anterior Cruciate Ligament Reconstruction Is Highly Effective in Treating High-Grade Anterior Knee Laxity. Am J Sports Med 2020;48:3478-85. [Crossref] [PubMed]
- Kennedy MI, Claes S, Fuso FA, et al. The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. Am J Sports Med 2015;43:1606-15. [Crossref] [PubMed]
- Kraeutler MJ, Welton KL, Chahla J, et al. Current Concepts of the Anterolateral Ligament of the Knee: Anatomy, Biomechanics, and Reconstruction. Am J Sports Med 2018;46:1235-42. [Crossref] [PubMed]
- Claes S, Luyckx T, Vereecke E, et al. The Segond fracture: a bony injury of the anterolateral ligament of the knee. Arthroscopy 2014;30:1475-82. [Crossref] [PubMed]
- Geeslin AG, Chahla J, Moatshe G, et al. Anterolateral Knee Extra-articular Stabilizers: A Robotic Sectioning Study of the Anterolateral Ligament and Distal Iliotibial Band Kaplan Fibers. Am J Sports Med 2018;46:1352-61. [Crossref] [PubMed]
- Inderhaug E, Stephen JM, Williams A, et al. Anterolateral Tenodesis or Anterolateral Ligament Complex Reconstruction: Effect of Flexion Angle at Graft Fixation When Combined With ACL Reconstruction. Am J Sports Med 2017;45:3089-97. [Crossref] [PubMed]
- Declercq J, Schuurmans M, Tack L, et al. Combined lateral extra-articular tenodesis and anterior cruciate ligament reconstruction: risk of osteoarthritis. Eur J Orthop Surg Traumatol 2023;33:1075-82. [Crossref] [PubMed]
- Bayer S, Meredith SJ, Wilson KW, et al. Knee Morphological Risk Factors for Anterior Cruciate Ligament Injury: A Systematic Review. J Bone Joint Surg Am 2020;102:703-18. [Crossref] [PubMed]
- Misir A, Sayer G, Uzun E, et al. Individual and Combined Anatomic Risk Factors for the Development of an Anterior Cruciate Ligament Rupture in Men: A Multiple Factor Analysis Case-Control Study. Am J Sports Med 2022;50:433-40. [Crossref] [PubMed]
- Brandon ML, Haynes PT, Bonamo JR, et al. The association between posterior-inferior tibial slope and anterior cruciate ligament insufficiency. Arthroscopy 2006;22:894-9. [Crossref] [PubMed]
Cite this article as: Nukuto K, Hoshino Y, Kataoka K, Kuroda R. Current development in surgical techniques, graft selection and additional procedures for anterior cruciate ligament injury: a path towards anatomic restoration and improved clinical outcomes—a narrative review. Ann Joint 2023;8:39.


