
Glenoid augmentation for subcritical bone loss: a narrative review
Introduction
Anterior shoulder instability typically presents in young and active individuals, with those participating in contact sports or high-risk activities being particularly susceptible. Although anterior labral tears have been referred to as the “essential lesion” in the pathogenesis of anterior shoulder instability (1), severe initial trauma and subsequent instability events precipitate further instability and worsening pathology (2-4). Among the sequelae of recurrent anterior shoulder instability, increasing magnitudes of anterior glenoid bone loss (GBL) have been identified as perhaps the most significant risk factor for recurrent instability (5-7).
Although glenoid bone defects were originally felt to be uncommon (1), Sugaya et al. demonstrated that 50% of shoulders with recurrent instability had an osseous Bankart lesion, while another 40% had loss of the normal anterior glenoid contour, without an identifiable osseous fragment (8). Griffith et al. similarly showed a high prevalence of bone loss (86%) in patients with unilateral recurrent dislocations and further stratified patients quantitatively, demonstrating a small majority of patients (51%) had less than 10% GBL and 37% had between 10% and 20% GBL (9).
The success of surgical repair is predicated upon the identification of GBL deficiency. Many analyses have defined thresholds of GBL, termed “critical defects”, above which GBL was deemed too large to overcome with soft tissue procedures alone. Initially, thresholds around 25% GBL (relative to glenoid width) were often cited (10-14), but Shin et al. demonstrated that 17% GBL was an inflection point for failure of isolated labral repair (6). However, more recent clinical analyses have honed in on lesser magnitudes of GBL, raising concerns that this threshold should actually be considerably lower. These lesser magnitudes of GBL have been termed subcritical bone loss and are typically classified as greater than 13.5% (15).
Although the upper limit of subcritical GBL remains somewhat controversial, opposite the classically defined critical bone loss thresholds, in each patient with some appreciable degree of GBL, concerns persist regarding the effectiveness of arthroscopic Bankart repair (ABR) alone in restoring shoulder stability. This concern is evident from the number of recently published studies designed to assess other procedures, such as glenoid augmentation and ABR with remplissage, for patients with subcritical bone loss (16-19). However, as evidenced by two ongoing randomized controlled trials (20,21) a great deal of uncertainty remains as to the ideal surgical treatment for this population. Accordingly, this review article focuses on the current evidence and controversies associated with the treatment of anterior shoulder instability in the setting of subcritical GBL, highlighting ongoing debate between open augmentation procedures and ABR with remplissage for this population. We present this article in accordance with the Narrative Review reporting checklist (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-36/rc).
Methods
A narrative review of the current existing literature was conducted with a focus on subcritical bone loss in anterior glenoid stabilization procedures, including review of forward citation and reference lists of selected articles. PubMed, MEDLINE, SPORT Discus, and Cochrane Database of Systematic Reviews databases were searched using the terms “subcritical bone loss” and “shoulder stabilization” from January 2000 through March 2023 (Table 1). Articles written in the English language were considered with peer-reviewed publication only, excluding case reports, technique guides, animal studies and conference abstracts.
Table 1
| Items | Specification |
|---|---|
| Date of search | March 12, 2023 |
| Databases and other sources searched | PubMed, MEDLINE, SPORT Discus and Cochrane Database of Systematic Reviews; review of forward citation and reference lists of selected article |
| Search terms used | “Subcritical” AND “glenoid bone loss” AND “shoulder stabilization” OR “glenoid augmentation” |
| Timeframe | January 2000 through March 2023 |
| Inclusion and exclusion criteria | Inclusion: peer reviewed articles, written in the English language, related to subcritical bone loss in anterior glenoid stabilization procedures. Exclusion: case reports, technique guides, conference abstracts and animal studies |
| Selection process | D.J.C. conducted the selection process independently; any questions were discussed with the senior author A.J.S. |
| Additional considerations | As subcritical bone loss is gaining significant popularity in the current literature in regards to surgical management, yet limited comparative and prospective studies currently exist in the literature, a traditional systematic review was purposefully not conducted. Instead, a narrative review was conducted to describe the current evidence and controversies that exist associated with the surgical treatment of anterior shoulder instability in the setting of the specific population with subcritical glenoid bone loss |
Pathoanatomy
The glenohumeral joint is an inherently unstable joint given its tremendous mobility and relatively limited bony constraint. The shallow articulation of the glenoid makes the shoulder dependent on soft tissue stabilizers such as the labrum, rotator cuff, glenohumeral ligaments and capsule, but insults to the bony architecture during initial or recurrent instability events have devastating effects on shoulder stability (2,3).
Most clearly, increasing magnitudes of GBL reduce the amount of force required to translate the humeral head, but anterior GBL also results in a loss of concavity/depth of the glenoid, further reducing glenohumeral constraint (22). Other glenoid parameters, such as glenoid version, have also been implicated as risk factors for recurrent instability (23-25). However, the extent to which they play a role may be more variable. For example, decreased retroversion may only serve as a clinically evident risk factor in individuals with concomitant subcritical bone loss (23). Similarly, sex-based differences in glenoid morphology in patients with and without instability also suggest that the pathophysiology and anatomic risk factors for instability may be different for males and females requiring distinct treatment considerations (26).
To discuss only GBL in anterior shoulder instability would be an incomplete characterization of the pathoanatomy. Although this review focuses on GBL as a key variable, when formulating a treatment plan, surgeons must consider other factors such as humeral-sided bone loss, ligamentous laxity, age, mechanism of injury, number of prior instability events and goals for future performance/activity, as these are all risk factors for continued instability and treatment failure (5,27,28).
Regarding the importance of soft tissue stabilizers, it is important to assess for combined labral injuries, extending posteriorly and/or superiorly (29-31). Failure to address the full extent of labral pathology will result in an inadequate recreation of the hammock suspension of the labral, capsular and inferior ligamentous complex, predisposing patients to an incomplete resolution of symptoms and recurrence. This also often serves as the rationale by some surgeons to perform diagnostic arthroscopy prior to open anterior glenoid augmentation procedures (32).
Next, similar to GBL, humeral-sided bone loss has important implications on treatment strategy. During a dislocation event the posterolateral humeral head often collides with the posterior rim of the glenoid causing an impaction type injury, or defect to bone and cartilage, termed a Hill-Sachs lesion. Afterward, the Hill-Sachs lesion decreases the arc of concentric glenohumeral joint motion and may engage on the anteroinferior glenoid, translating the humeral head and predisposing to further instability. Recognition of humeral bone loss (alongside GBL) helped establish the bipolar bone loss paradigm, which ultimately transformed the way surgeons think about shoulder instability. This enhanced understanding of the pathoanatomy has led to the utilization of surgical procedures that have been proposed to directly address deranged anatomy. Accordingly, a procedure such as remplissage, can directly address a Hill-Sachs lesion, whereas glenoid augmentation was designed to restore glenoid architecture in the setting of critical bone defects. However, more recently, both remplissage and glenoid augmentation procedures have seen increasingly utilization outside of these classic indications, especially in patient with subcritical bone loss, given their greater magnitude of effect on stabilization as compared to the ABR alone.
Finally, demographic factors such as age, participation in contact/overhead sports and ligamentous laxity factor into management decisions. While they are often thought of more subjectively than thresholds of bone loss, they undoubtedly influence treatment decisions. The Nonoperative Injury Severity Index Score (NSIS) includes six risk factors for failure of non-operative management of anterior shoulder instability including age >15 years, bone loss, type of instability, contact sport, male sex and arm dominance (33). Tokish et al. found low risk patients (NSIS <7) had an overall high return to sport rate (97%) when treated non-operatively (33). In order to encourage their inclusion in decision making and more objectively guide management, scoring systems such as the Instability Severity Index Score (ISIS) (34) and Glenoid Track Instability Management Score (GTIMS) (35) have been described. However, the validity of these scoring systems is still in question (35-38), in part due to their own designs, which utilize imprecise radiographic determinations of bipolar bone loss in order to maintain their simplicity and utility. The limitations of these scoring systems notwithstanding, what is truly important is for surgeons is to understand the risk factors for recurrence and to consider each of them when formulating a treatment plan.
Imaging
When evaluating patients with anterior shoulder instability, a standard radiographic series includes a Grashey, axillary (or axillary equivalent) and scapular Y-view. Magnetic resonance imaging (MRI) is the advanced imaging modality of choice for shoulder instability. In the days to weeks following a shoulder instability event, hematoma from the injury may act similarly to contrast in an MR arthrogram in delineating injuries of the chondrolabral junction and/or glenohumeral ligaments. However, in subacute or chronic injuries magnetic resonance arthrography enhances the sensitivity and specificity for diagnosing intraarticular pathology (39) While several reports have demonstrated the utility of MRI in accurately measuring GBL (40), computed tomography (CT) is perhaps the modality of choice for obtaining precise measurements of GBL. More recently, 3D CT reconstructions with and without humeral head subtraction have also been increasingly utilized to characterize the extent of bone loss. As an alternative, 3D MRI measurements for bone loss in glenohumeral instability using isotropic volumetric interpolated breath-hold examination (VIBE) sequencing has been shown to be equivalent to 3D CT models and nearly two times cheaper than MRI and CT with 3D reconstructions (41,42).
Assessment of GBL is performed via sagittal advanced imaging, wherein the inferior glenoid is modeled as a circle and the extent of bone missing from the circle is bone loss. There are several techniques to characterize bone loss this way, including as a percentage of the glenoid diameter, wherein the width of the bone loss (in mm) is divided by the diameter of the circle (Figure 1). Other techniques include utilizing the area (mm2) of bone loss and the area of the circle. Also relevant to a discussion of subcritical bone loss is the study by Lansdown et al. which demonstrated that identification of a flat anterior glenoid corresponds to 12.8%±3% GBL (43).
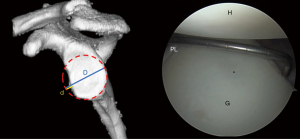
Finally, an assessment of Hill-Sachs lesion size, location and on-track/off-track status may help inform surgical management. A Hill-Sachs lesion is termed off-track when the Hill-Sachs lesion interval is greater than the glenoid track, with the glenoid track being defined as 0.83(D)-d, where D is the diameter of the circle modeled on the inferior glenoid and d is the extent of GBL (Figure 1). Although on-track and off-track have previously been defined as binary, more recent analyses suggest that it may be a spectrum of risk, with lesions that are closer to off-track status, termed “near-track lesions”, still being at higher risk of failure (44).
Surgical management of subcritical bone loss
In 2000, Burkhart and De Beer (13) proposed the concept of the inverted pear glenoid, an arthroscopic indicator of a substantial glenoid bone defect which is at high risk of failure with ABR. Later, Lo et al. (10) quantified the GBL associated with an inverted pear glenoid, demonstrating in cadavers that this geometry was the result of a mean GBL of 28.8% (Figure 2). Yamamoto et al. then performed a biomechanical cadaveric study demonstrating that 26% GBL (relative to the glenoid width) significantly diminished shoulder stability (11). The authors concluded that patients with this level of bony deficiency were not candidates for arthroscopic soft tissue repairs (11). Boileau et al. also noted recurrent instability after ABR was associated with GBL >25% (5). Altogether these studies created the basis for so called “critical bone loss”, deemed so severe that an ABR would not suffice.

Subsequently, the durability of soft tissue repairs in patients with even less bone loss was questioned. Shin et al. first raised concerns that GBL of 15% or more was a critical defect, wherein soft tissue repair could not restore glenohumeral translation (7). However, clinically the same group (6) found that 17% GBL was a more accurate critical threshold for shoulder function and surgical failure, as have others (45). Later, Shaha et al. defined “subcritical bone loss” in a young, military population to be 13.5%, wherein patients had lower WOSI scores above this threshold (15). However, currently subcritical bone loss corresponds to >13.5% GBL, with no clear upper threshold, making comparison of subsequent and recent studies difficult. Nevertheless, we will highlight the available evidence in this population of patients, demonstrating the growing body of literature in support of operations aside from isolated ABR.
It should be noted that primary ABR remains the predominate surgery performed for primary anterior shoulder instability, while glenoid augmentation and open Bankart repair continue to be used sparingly in the United States (31). Rightfully so, Dickens et al. (46) showed that intercollegiate football players with <13.5% GBL went on to successful outcomes with ABR alone, with low rates of recurrent instability. However, when Dekker et al. analyzed more than 400 patients undergoing ABR at a minimum of four years follow-up, >15% GBL was a risk factor for recurrent instability and inferior clinical outcomes (47).
Historically, the Latarjet procedure was considered for substantial glenoid defects, but the illumination of subcritical bone loss, with and without Hill-Sachs lesions (i.e., bipolar bone loss), has expanded its indications. Min et al. (48) retrospectively compared ABR to open Latarjet procedures for subcritical bone loss, defined as 13.5–24% GBL. They found no significant difference in WOSI scores, but the Latarjet cohort had higher SANE scores (48). Similarly, Rossi et al. analyzed a population of rugby players with GBL <20% undergoing Latarjet, against a historical treatment group of ABRs, finding higher rates of recurrent instability (20% vs. 4%) and rates of reoperation (16% vs. 4%) for the ABR group as compared to the Latarjet group (49). Importantly, this study was born out of the authors transitioning their instability practice in Rugby players to Latarjet, given conspicuously high rates of recurrent instability with ABR. While the results clearly favor the Latarjet procedure in this specific subpopulation with <20% GBL, it is difficult to assess the exact role of subcritical bone loss given the majority of patients did not have any appreciable bone loss and these contact athletes are obviously exposed to unique risks for recurrence. Jeon et al. (50) similarly retrospectively reviewed patients undergoing ABR or Latarjet, for what the authors termed “borderline” bone defects from 15–20% GBL. While they concluded that both provide satisfactory clinic outcomes, the Latarjet procedure resulted in a lower rate of recurrent instability and less external rotation loss and thus they concluded it may be a more reliable option in this cohort. While Jeon et al. (50) excluded patients with off-track Hill-Sachs lesions, Yang et al. evaluated ABR plus remplissage versus Latarjet in a population of patients with off-track lesions and subcritical bone loss, which they defined as <25% (51). Notably, their mean GBL was 10.4%±6.8% and 12.3%±8.79% for ABR plus remplissage and Latarjet, respectively. Multivariate analysis revealed that Latarjet procedures had lower odds of recurrent instability in the revision setting than ABR plus remplissage and that the odds of recurrence were also lower in collision athletes and those with 10–15% bone loss and >15% bone loss.
Contrary to the results suggesting the supremacy of Latarjet over arthroscopic, soft tissue-only repairs, Horinek et al. recently demonstrated that ABR and remplissage yields similar 2 year outcomes to Latarjet in patients with >15% GBL (52). This lead the authors to conclude that remplissage is a consideration in patients with GBL >15% and it is notable that their cohort includes patients well beyond subcritical bone loss thresholds, with mean GBL in both groups of 25%. The same authors also published a similar comparative study on a wider range of GBL, wherein remplissage resulted in similar or better outcomes as compared to Latarjet, despite marginally higher preoperative GBL and a higher rate of off-track lesions in the remplissage group (53). Their work is also consistent with that from Pathak et al. reporting on ABR with remplissage in patients with GBL <20% and large Hill-Sachs lesions (54). While it appears that remplissage may be robust enough to rival the Latarjet procedure mid-term and long-term follow-up of these populations, with subcritical bone loss, undergoing these procedures are still need to provide a definitive answer as to the most appropriate treatment option.
Aside from the Latarjet procedure, utilization of distal tibial allograft (DTA) and local autograft is becoming increasingly prevalent. However, there has been limited study in a subcritical bone loss population. A recent cadaveric and CT scan based study demonstrated that Latarjet and distal clavicle grafts were able to completely or near completely restore the glenoid at 20% and 30% GBL, however scapular spine grafts could only restore the glenoid in two-thirds of 20% defects (55). However, in a population of subcritical bone loss, scapular spine autograft has already been shown to result in satisfactory outcomes at 2-year follow-up, with no episodes of recurrent instability (18), suggesting the other grafts also represent viable solutions for subcritical bone loss.
Finally, transfer of the long head of the biceps to the glenoid, termed dynamic anterior stabilization (DAS), has been shown to reduce anterior translation in a 15% glenoid defect model when combined with ABR as compared with ABR alone (56). However, Latarjet remained the most effective procedure at reducing anterior translation. Similarly, in another cadaveric study of 20% GBL, Latarjet also demonstrated significantly higher loads to dislocate than the long head of biceps tendon and finally a series of patients with GBL <20% undergoing DAS with ABR demonstrated a 13.6% (3/23) recurrence rate at 3.2 years follow-up leaving questions as to the role and utility of this procedure (17,57).
To a lesser extent, arthroscopic conjoint tendon transfer has also been described to produce a dynamic-sling effect using suspensory and interference fixation as an option for patients with a failed labral repair with subcritical bone loss <15% and an on-track Hill-Sachs lesion (58). In this small case series of eight patients, median WOSI scores improved with 100% return to sport and no further dislocation event at median follow-up of 31 months. Similar results have been shown in a case series for treatment of traumatic shoulder instability with 25% or greater GBL and an engaging Hill-Sachs lesion with follow-up of 31 months (59). However, outcomes from this procedure have only been described in case series with limited follow-up.
In an effort to answer many of the questions posed already, two prospective efforts, the STABLE (20) and OASIS (21) trials are ongoing. The STABLE Trial is a randomized controlled trial (RCT) comparing ABR with remplissage to Latarjet, and the OASIS Trial is a RCT comparing ABR with remplissage to open Bankart repair to Latarjet in patients with subcritical bone loss (Tables 2,3). The successful execution of these efforts will assuredly offer critical information as to the optimal treatment approach to recurrent shoulder instability observed in the setting of subcritical GBL.
Table 2
| Pros/cons | Arthroscopic Bankart | Arthroscopic Bankart + Remplissage | Open Bankart | Glenoid Augmentation/Latarjet |
|---|---|---|---|---|
| Pros | Most common stability procedure | Enhanced stability compared to isolated Bankart | Able to perform large capsular shift | Restores glenoid architecture |
| Easy to address pan-labral pathology | Addresses concomitant Hill-Sachs lesion | Utilization of arthroscopic implants/tools remains helpful | Low rates of recurrent instability | |
| Bone to bone healing | ||||
| Cons | Questionable long-term stability | External rotation loss | Decreasing utilization since early 2000s | Concern regarding high complication rates |
| Concern regarding damage to infraspinatus | Unclear if truly superior to arthroscopic repair | Arthroscopic augmentation has significant learning curve | ||
| Allografts have substantial cost |
Table 3
| Author | Surgical procedure | N | Follow-up | Population | Outcomes |
|---|---|---|---|---|---|
| Shaha et al., 2015 (15) | ABR | 72 | 48.3 months | 0–35.5% GBL | Worse WOSI scores for patients >13.5% GBL |
| Dickens et al., 2017 (46) | ABR | 50 | 3.2 years | <20% GBL, intercollegiate football players, off-track/engaging HSL excluded | All patients with GBL >13.5% (n=3) had recurrence instability, none with GBL <13.5% (n=47) did |
| Yamamoto et al., 2019 (45) |
ABR | 43 | 32 months | <25% GBL | WOSI sores significant lower for >17% GBL, than <17%. Authors consider 17–25% subcritical bone loss |
| Dekker et al., 2020 (47) | ABR | 405 | 61 months | 0–25% GBL | Multivariate analysis revealed >15% GBL associated with 3× greater odds of recurrent instability |
| Collin et al., 2022 (17) | ABR + DAS | 22 | 3.2 years | <20% GBL | Recurrence rate: 13.6% |
| Pathak et al., 2022 (54) | ABR + Remp | 24 | Min 2 years | <20% GBL and substantial HSL | 4% (n=1) recurrent instability rate |
| Jeon et al., 2018 (50) | ABR vs. Latarjet | 149 | 28.9 months | 15–20% GBL | Recurrence rate: ABR: 22.9%, Latarjet: 6.5% (P=0.40) |
| Rossi et al., 2021 (49) | ABR vs. Latarjet | 130 | 40 months | <20% GBL, rugby players | Recurrence rate: ABR: 20%, Latarjet: s4% (P=0.01) |
| Min et al., 2023 (48) | ABR vs. Latarjet | 47 | Min 2 years | 13.5–24% GBL | No difference in WOSI scores, but higher SANE scores for Latarjet |
| Horinek et al., 2022 (52) | ABR + Remp vs. Latarjet | 47 | 2 years | >15% GBL, included off-track lesions | ABR + Remp and Latarjet provided similar outcomes, no recurrent dislocations in either group |
| Horinek et al., 2022 (53) | ABR + Remp vs. Latarjet | 258 | Min 2 years | 0–47% GBL, off track lesions included | ABR + Remp had similar or better outcomes as compared to Latarjet; Recurrence rate: ABR + Remp: 1.4% (n=1), Latarjet: 3.2% (n=6) (P=0.678) |
| Yang et al., 2018 (51) | ABR + Remp vs. Latarjet | 189 | 3.2 years | <25% GBL and off-track lesion | Multivariate analysis showed increased risk of recurrence with ABR + Remp compared to Latarjet, including 6.48 odds ratio for >15% GBL |
| Xiang et al., 2021 (18) | Arthroscopic scapular spine autograft | 27 | Min 2 years | 10–15% GBL | No episodes of recurrent instability, significantly improved Constant-Murley score, DASH score and VAS score |
ABR, Arthroscopic Bankart repair; WOSI, Western Ontario Shoulder Instability Index; GBL, glenoid bone loss; SANE, Single Assessment Numeric Evaluation; HSL, Hill-Sachs lesion; DAS, dynamic anterior stabilization; Remp, Remplissage; Min, minimum; DASH, disabilities of the arm, shoulder and hand; VAS, visual analog scale for pain.
Conclusions
There is no consensus regarding the optimal treatment approach to recurrent shoulder instability in the setting of subcritical GBL. Conversely, there is a growing agreement that isolated ABR is likely inadequate and subcritical GBL should prompt consideration of a more robust operation. To this end, interest in glenoid augmentation continues to grow as a reliable technique for recreating the native architecture and restoring glenohumeral stability.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jonathan D. Hughes and Albert Lin) for the series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” published in Annals of Joint. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-36/rc
Peer Review File: Available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-36/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoj.amegroups.com/article/view/10.21037/aoj-23-36/coif). The series “Bone Loss in Shoulder Instability and Shoulder Arthroplasty” was commissioned by the editorial office without any funding or sponsorship. D.J.C. reports being an editorial board member for Arthroscopy and receiving research support from AANA unrelated to the current work. M.T.D. reports being a board or committee member AAOS Resident Assembly and an editorial board member for Arthroscopy. R.U.H. reports receiving personal fees from Stryker, Arthrex, Lippincott Williams & Wilkins, and Arthroscopy, being a board member for AANA and America Shoulder and Elbow Surgeons, receiving research support from AANA unrelated to the current work. A.J.S. reports receiving personal fees from Arthroscopy and research support from Embody Inc., unrelated to the current work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder-joint. Br J Surg 1938;26:23-9. [Crossref]
- McMahon PJ, Yang BY, Chow S, et al. Anterior shoulder dislocation increases the propensity for recurrence: a cadaveric study of the number of dislocations and type of capsulolabral lesion. J Shoulder Elbow Surg 2013;22:1046-52. [Crossref] [PubMed]
- Milano G, Grasso A, Russo A, et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med 2011;39:1870-6. [Crossref] [PubMed]
- Dickens JF, Slaven SE, Cameron KL, et al. Prospective Evaluation of Glenoid Bone Loss After First-time and Recurrent Anterior Glenohumeral Instability Events. Am J Sports Med 2019;47:1082-9. [Crossref] [PubMed]
- Boileau P, Villalba M, Héry JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755-63. [Crossref] [PubMed]
- Shin SJ, Kim RG, Jeon YS, et al. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. Am J Sports Med 2017;45:1975-81. [Crossref] [PubMed]
- Shin SJ, Koh YW, Bui C, et al. What Is the Critical Value of Glenoid Bone Loss at Which Soft Tissue Bankart Repair Does Not Restore Glenohumeral Translation, Restricts Range of Motion, and Leads to Abnormal Humeral Head Position? Am J Sports Med 2016;44:2784-91. [Crossref] [PubMed]
- Sugaya H, Moriishi J, Dohi M, et al. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 2003;85:878-84. [Crossref] [PubMed]
- Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol 2008;190:1247-54. [Crossref] [PubMed]
- Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy 2004;20:169-74. [Crossref] [PubMed]
- Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 2009;37:949-54. [Crossref] [PubMed]
- Itoi E, Lee SB, Berglund LJ, et al. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 2000;82:35-46. [Crossref] [PubMed]
- Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000;16:677-94. [Crossref] [PubMed]
- Bigliani LU, Newton PM, Steinmann SP, et al. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med 1998;26:41-5. [Crossref] [PubMed]
- Shaha JS, Cook JB, Song DJ, et al. Redefining "Critical" Bone Loss in Shoulder Instability: Functional Outcomes Worsen With "Subcritical" Bone Loss. Am J Sports Med 2015;43:1719-25. [Crossref] [PubMed]
- Horinek JL, Menendez ME, Callegari JJ, et al. Consideration May Be Given to Lowering the Threshold for the Addition of Remplissage in Patients With Subcritical Glenoid Bone Loss Undergoing Arthroscopic Bankart Repair. Arthrosc Sports Med Rehabil 2022;4:e1283-9. [Crossref] [PubMed]
- Collin P, Nabergoj M, Denard PJ, et al. Arthroscopic Biceps Transfer to the Glenoid With Bankart Repair Grants Satisfactory 2-Year Results for Recurrent Anteroinferior Glenohumeral Instability in Subcritical Bone Loss. Arthroscopy 2022;38:1766-71. [Crossref] [PubMed]
- Xiang M, Yang J, Chen H, et al. Arthroscopic Autologous Scapular Spine Bone Graft Combined With Bankart Repair for Anterior Shoulder Instability With Subcritical (10%-15%) Glenoid Bone Loss. Arthroscopy 2021;37:2065-74. [Crossref] [PubMed]
- Haroun HK, Sobhy MH, Abdelrahman AA. Arthroscopic Bankart repair with remplissage versus Latarjet procedure for management of engaging Hill-Sachs lesions with subcritical glenoid bone loss in traumatic anterior shoulder instability: a systematic review and meta-analysis. J Shoulder Elbow Surg 2020;29:2163-74. [Crossref] [PubMed]
- Khan M, Bedi A, Degen R, et al. A pilot multicenter randomized controlled trial comparing Bankart repair and remplissage with the Latarjet procedure in patients with subcritical bone loss (STABLE): study protocol. Pilot Feasibility Stud 2022;8:20. [Crossref] [PubMed]
- Popchak A, Dickens JF. Open Versus Arthroscopic Stabilization of Shoulder Instability With Subcritical Bone Loss: The OASIS Trial (OASIS). University of Pittsburgh; 2022. NCT04809064.
- Yamamoto N, Muraki T, Sperling JW, et al. Stabilizing mechanism in bone-grafting of a large glenoid defect. J Bone Joint Surg Am 2010;92:2059-66. [Crossref] [PubMed]
- Li RT, Sheean A, Wilson K, et al. Decreased Glenoid Retroversion Is a Risk Factor for Failure of Primary Arthroscopic Bankart Repair in Individuals With Subcritical Bone Loss Versus No Bone Loss. Arthroscopy 2021;37:1128-33. [Crossref] [PubMed]
- Aygün Ü, Çalik Y, Işik C, et al. The importance of glenoid version in patients with anterior dislocation of the shoulder. J Shoulder Elbow Surg 2016;25:1930-6. [Crossref] [PubMed]
- Sheean AJ, Owens BD, Lesniak BP, et al. The Effect of Glenoid Version on Glenohumeral Instability. J Am Acad Orthop Surg 2022;30:e1165-78. [Crossref] [PubMed]
- Cohn MR, DeFroda SF, Huddleston HP, et al. Does native glenoid anatomy predispose to shoulder instability? An MRI analysis. J Shoulder Elbow Surg 2022;31:S110-6. [Crossref] [PubMed]
- Phadnis J, Arnold C, Elmorsy A, et al. Utility of the Instability Severity Index Score in Predicting Failure After Arthroscopic Anterior Stabilization of the Shoulder. Am J Sports Med 2015;43:1983-8. [Crossref] [PubMed]
- Ahmed I, Ashton F, Robinson CM. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability: functional outcomes and identification of risk factors for recurrence. J Bone Joint Surg Am 2012;94:1308-15. [Crossref] [PubMed]
- Swan ER, Lynch TB, Sheean AJ, et al. High Incidence of Combined and Posterior Labral Tears in Military Patients With Operative Shoulder Instability. Am J Sports Med 2022;50:1529-33. [Crossref] [PubMed]
- Song DJ, Cook JB, Krul KP, et al. High frequency of posterior and combined shoulder instability in young active patients. J Shoulder Elbow Surg 2015;24:186-90. [Crossref] [PubMed]
- Cognetti DJ, Tenan MS, Dickens JF, et al. The Glenoid Track Paradigm Does Not Reliably Affect Military Surgeons' Approach to Managing Shoulder Instability. Arthrosc Sports Med Rehabil 2023;5:e403-9. [Crossref] [PubMed]
- Arrigoni P, Huberty D, Brady PC, et al. The value of arthroscopy before an open modified latarjet reconstruction. Arthroscopy 2008;24:514-9. [Crossref] [PubMed]
- Tokish JM, Thigpen CA, Kissenberth MJ, et al. The Nonoperative Instability Severity Index Score (NISIS): A Simple Tool to Guide Operative Versus Nonoperative Treatment of the Unstable Shoulder. Sports Health 2020;12:598-602. [Crossref] [PubMed]
- Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 2007;89:1470-7. [Crossref] [PubMed]
- Di Giacomo G, Peebles LA, Pugliese M, et al. Glenoid Track Instability Management Score: Radiographic Modification of the Instability Severity Index Score. Arthroscopy 2020;36:56-67. [Crossref] [PubMed]
- Dekker TJ, Peebles LA, Bernhardson AS, et al. Limited Predictive Value of the Instability Severity Index Score: Evaluation of 217 Consecutive Cases of Recurrent Anterior Shoulder Instability. Arthroscopy 2021;37:1381-91. [Crossref] [PubMed]
- Chan AG, Kilcoyne KG, Chan S, et al. Evaluation of the Instability Severity Index score in predicting failure following arthroscopic Bankart surgery in an active military population. J Shoulder Elbow Surg 2019;28:e156-63. [Crossref] [PubMed]
- Ruiz Ibán MA, Asenjo Gismero CV, Moros Marco S, et al. Instability severity index score values below 7 do not predict recurrence after arthroscopic Bankart repair. Knee Surg Sports Traumatol Arthrosc 2019;27:3905-11. [Crossref] [PubMed]
- Chandnani VP, Yeager TD, DeBerardino T, et al. Glenoid labral tears: prospective evaluation with MRI imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol 1993;161:1229-35. [Crossref] [PubMed]
- Owens BD, Burns TC, Campbell SE, et al. Simple method of glenoid bone loss calculation using ipsilateral magnetic resonance imaging. Am J Sports Med 2013;41:622-4. [Crossref] [PubMed]
- Lander ST, Liles JL, Kim BI, et al. Comparison of computed tomography and 3D magnetic resonance imaging in evaluating glenohumeral instability bone loss. J Shoulder Elbow Surg 2022;31:2217-24. [Crossref] [PubMed]
- Stillwater L, Koenig J, Maycher B, et al. 3D-MR vs. 3D-CT of the shoulder in patients with glenohumeral instability. Skeletal Radiol 2017;46:325-31. [Crossref] [PubMed]
- Lansdown DA, Wang K, Yanke AB, et al. A Flat Anterior Glenoid Corresponds to Subcritical Glenoid Bone Loss. Arthroscopy 2019;35:1788-93. [Crossref] [PubMed]
- Barrow AE, Charles SJ, Issa M, et al. Distance to Dislocation and Recurrent Shoulder Dislocation After Arthroscopic Bankart Repair: Rethinking the Glenoid Track Concept. Am J Sports Med 2022;50:3875-80. [Crossref] [PubMed]
- Yamamoto N, Kawakami J, Hatta T, et al. Effect of subcritical glenoid bone loss on activities of daily living in patients with anterior shoulder instability. Orthop Traumatol Surg Res 2019;105:1467-70. [Crossref] [PubMed]
- Dickens JF, Owens BD, Cameron KL, et al. The Effect of Subcritical Bone Loss and Exposure on Recurrent Instability After Arthroscopic Bankart Repair in Intercollegiate American Football. Am J Sports Med 2017;45:1769-75. [Crossref] [PubMed]
- Dekker TJ, Peebles LA, Bernhardson AS, et al. Risk Factors for Recurrence After Arthroscopic Instability Repair-The Importance of Glenoid Bone Loss >15%, Patient Age, and Duration of Symptoms: A Matched Cohort Analysis. Am J Sports Med 2020;48:3036-41. [Crossref] [PubMed]
- Min KS, Wake J, Cruz C, et al. Surgical treatment of shoulder instability in active-duty service members with subcritical glenoid bone loss: Bankart vs. Latarjet. J Shoulder Elbow Surg 2023;32:771-5. [Crossref] [PubMed]
- Rossi LA, Tanoira I, Gorodischer T, et al. Recurrence and Revision Rates With Arthroscopic Bankart Repair Compared With the Latarjet Procedure in Competitive Rugby Players With Glenohumeral Instability and a Glenoid Bone Loss <20. Am J Sports Med 2021;49:866-72. [Crossref] [PubMed]
- Jeon YS, Jeong HY, Lee DK, et al. Borderline Glenoid Bone Defect in Anterior Shoulder Instability: Latarjet Procedure Versus Bankart Repair. Am J Sports Med 2018;46:2170-6. [Crossref] [PubMed]
- Yang JS, Mehran N, Mazzocca AD, et al. Remplissage Versus Modified Latarjet for Off-Track Hill-Sachs Lesions With Subcritical Glenoid Bone Loss. Am J Sports Med 2018;46:1885-91. [Crossref] [PubMed]
- Horinek JL, Menendez ME, Narbona P, et al. Arthroscopic Bankart Repair With Remplissage as an Alternative to Latarjet for Anterior Glenohumeral Instability With More Than 15% Glenoid Bone Loss. Orthop J Sports Med 2022;10:23259671221142257. [Crossref] [PubMed]
- Horinek JL, Menendez ME, Narbona P, et al. Remplissage Yields Similar 2-Year Outcomes, Fewer Complications, and Low Recurrence Compared to Latarjet Across a Wide Range of Preoperative Glenoid Bone Loss. Arthroscopy 2022;38:2798-805. [Crossref] [PubMed]
- Pathak S, Haidermota MJ. Arthroscopic Bankart and Remplissage for Anteroinferior Instability With Subcritical Bone Loss Has a Low Recurrence Rate. Arthrosc Sports Med Rehabil 2022;4:e695-703. [Crossref] [PubMed]
- Rodriguez S, Mancini MR, Kakazu R, et al. Comparison of the Coracoid, Distal Clavicle, and Scapular Spine for Autograft Augmentation of Glenoid Bone Loss: A Radiologic and Cadaveric Assessment. Am J Sports Med 2022;50:717-24. [Crossref] [PubMed]
- Nicholson AD, Carey EG, Mathew JI, et al. Biomechanical analysis of anterior stability after 15% glenoid bone loss: comparison of Bankart repair, dynamic anterior stabilization, dynamic anterior stabilization with Bankart repair, and Latarjet. J Shoulder Elbow Surg 2022;31:2358-65. [Crossref] [PubMed]
- Lobao MH, Abbasi P, Murthi AM. Long head of biceps transfer to augment Bankart repair in chronic anterior shoulder instability with and without subcritical bone loss: a biomechanical study. J Shoulder Elbow Surg 2022;31:1062-72. [Crossref] [PubMed]
- Patel V, Pearse E, Arnander M, et al. Two-year results of arthroscopic conjoint tendon transfer procedure for the management of failed anterior stabilization of the shoulder. JSES Int 2021;5:519-24. [Crossref] [PubMed]
- Douoguih WA, Goodwin D, Churchill R, et al. Conjoined Tendon Transfer for Traumatic Anterior Glenohumeral Instability in Patients With Large Bony Defects and Anterior Capsulolabral Deficiency. Arthroscopy 2018;34:12-20. [Crossref] [PubMed]
Cite this article as: Cognetti DJ, DeFoor MT, Hartzler RU, Sheean AJ. Glenoid augmentation for subcritical bone loss: a narrative review. Ann Joint 2024;9:15.


